2010 Group Project 4
Percutaneous Umbilical Cord Blood Sampling
INTRODUCTION
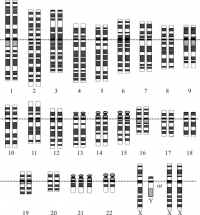
Percutaneous Umbilical Cord Blood Sampling (PUBS) is an invasive pre-natal diagnostic procedure performed during the second trimester (between week 18 to 22) where a sample of fetal blood is extracted from the umbilical vein in the umbilical cord using a fine needle via the abdomen of the mother. The extracted blood can then be used to detect certain anomalies including chromosome abnormalities such as Down Syndrome, blood disorders such as Fetal Haemolytic Disease and intrauterine infection, growth retardation, and some birth defects as well as metabolic disorders. PUBS is often used when other diagnostic tests such as Ultrasound, Amniocentesis and Chorionic Villus Sampling do not yield conclusive results. This pre-natal diagnostic technique is also used to deliver certain therapies such as the administration of medicine and transfusion of blood directly to the fetus.
Although it is a very useful diagnostic technique, there are many complications associated with the procedure from haemorrhage and fetal bradycardia to premature birth and fetal death. The mortality rate associated directly to procedural factors has been found to be approximately 1 to 2 times out of every 100 procedures. The long list of associated risks have been found to be related to procedural factors such as duration and the number of punctures as well as individual circumstances of the patient for example gestational age.
Despite the risks involved, the one of the benefits of PUBS over that of other pre-natal diagnostic techniques such as Amniocentesis and Chorionic Villus Sampling (CVS), is that genetic information also known as Karyotypes is available much sooner after the procedure. This is especially important in cases requiring rapid diagnosis and/or management.
[1][2][3][4][5]
| Advantages | Disadvantages |
|---|---|
|
|
HISTORY
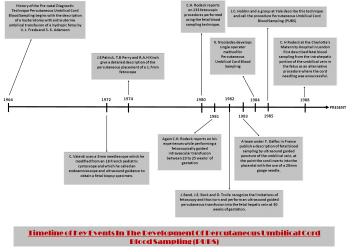
Obtaining fetal blood during pregnancy for pre-natal diagnosis has been possible since 1964 however the method used, fetoscopy was extremely limited and thus only employed in a very few cases. Yet with the introduction of the modern day PUBS using ultrasound to obtain fetal blood samples in 1982 by Fernand Daffos has made the procedure simpler and relatively safe in comparison to before. The development of this safe and effective technique evolved over many years and required the minds of many world class scientist and doctors to make PUBS the pre-natal diagnostic technique it is today.
Timeline of Key Events In The Development Of Percutaneous Umbilical Cord Blood Sampling (PUBS)
| Year | Key developments |
|---|---|
| 1964 | History of the Pre-natal Diagnostic Technique Percutaneous Umbilical Cord Blood Sampling begins with the description of a hysterotomy with extra uterine umbilical transfusion of a hydropic fetus by V. J. Freda and S. K. Adamson |
| 1972 | C. Valenti uses a 5mm needlescope which he modified from an 18 French pediatric cystoscope and which he called an endoamnioscope and ultrasound guidance to obtain a fetal biopsy specimen. |
| 1974 | J.E Patrick, T.B Perry and R.A.H Kinch give a detailed description of the percutaneous placement of a 1.7mm fetoscope |
| 1980 | C.H. Rodeck reports on 133 fetoscopic procedures performed using the fetal blood sampling technique. |
| 1981 | Again C.H. Rodeck reports on his experiences while performing a fetoscopically guided intravascular transfusion between 23 to 25 weeks’ of gestation |
| 1982 | J. Band, J.E. Bock and D. Trolle recognize the limitations of fetoscopy and thus turn and perform an ultrasound guided percutaneous transfusion into the fetal hepatic vein at 30 weeks of gestation. |
| 1983 | A team under F. Daffos in France publish a description of fetal blood sampling by ultrasound guided puncture of the umbilical vein, at the point the cord inserts into the placental with the use of a 20mm gauge needle. |
| 1984 | K. Nicolaides develops single operator method for Percutaneous Umbilical Cord Blood Sampling |
| 1985 | J.C. Hobbin and a group at Yale describe this technique and call the procedure Percutaneous Umbilical Cord Blood Sampling (PUBS) |
| 1988 | C. H Rodeck at the Charlotte's Maternity Hospital in London first described fetal blood sampling from the intrahepatic portion of the umbilical vein in the fetus as an alternative procedure where the cord needling was unsuccessful. |
Key Scientist and Doctors in Percutaneous Umbilical Cord Blood Sampling
Fernand Daffos
Fernand Daffos and a team of doctors such as François Forestier and Martine Capella-Pavlovsky in 1982 developed a new and improved technique for the collection of fetal blood samples. The new and improved technique for collection of pure samples of fetal blood were obtained from the umbilical cord more precisely the large vein using a twenty-gauge spinal needle that was guided by real time ultrasound images. Fetal blood was collected from the cord approximately 2.5cm from the connection to the placenta into a syringe which is attached to the need where 1 to 2 millilitres of blood is collected. Fernand Daffos’s procedure was a dramatic improvement in fetal blood collection compare to other methods for prenatal diagnosis of disease. Thus he is can be deemed the father of modern day pubs.
Professor Stuart Campbell
In 1982 Professor Campbell aside from looking at fetal malformation using real time ultrasound started systematic investigation in many other areas, pioneering work in areas such as ovarian cancer screening with ultrasound, Doppler fetal and utero-placental blood flow in many pre-natal pathological conditions. Stuart Campbell also investigated ovarian follicular developments, routine ultrasound population screening and umbilical and placental blood sampling. Yet most importantly Professor Stuart Campbell introduced the concept of actually screening for the later development of pre-eclampsia and intra-uterine growth retardation basing on early uteroplacental waveforms.
Kypros Nicolaides
Kypros Nicolaides was one of the first doctors that discarded the fetoscope and practiced all blood sampling procedures by extracting blood from the placental cord insertion which was then termed Percutaneous Umbilical Cord Blood Sampling . Like stated above the technique of PUBS or Cordocentsis was initially pioneered in France in 1983 by Fernand Daffos however, it was Kypros Nicolaides who actually developed the single operator method. This allowed him and many other doctors to study many aspects of fetal physiology and pathophysiology such as fetal blood gases. The single operator method developed also allowed Nicolaides to investigate the correlations between fetal blood gases and Doppler, fetal metabolism, endocrinology, immunology, haematology, biochemistry in diabetic pregnancies.
PERCUTANEOUS UMBILICAL CORD BLOOD SAMPLING (PUBS) IN COMPARISON WITH OTHER DIAGNOSTIC TECHNIQUES
PUBS is usually performed after non-invasive procedures such as ultrasound and biochemical markers, have indicated the possibility of genetic disorders. Because, these tests generally produce highly sensitive results, they are not always reliable at giving an accurate diagnosis. Therefore, an invasive technique such as PUBS is employed to in an attempt to provide more conclusive and accurate information.[15]
PUBS may also be used when other invasive pre-natal diagnostic tests including chorionic villi sampling (CVS) and amniocentesis do not yield conclusive results. These methods are similar in that they involve the examination of cell samples obtained directly from the developing fetal structures.
| PUBS | Chorionic Villi Sampling | Amniocentesis | |
|---|---|---|---|
| Risk of complications | 1-2% | 2% | 0.5-1% |
| Recommended time period for testing | 18-23 weeks | 8-11 weeks | 16-18 weeks |
| Available diagnostic analyses |
|
|
|
| Time taken for samples to be cultured | 72 hours | 9-10 days | 10-11 days |
Further Information on Other Pre-Natal Diagnostic Techniques
PROCEDURE
When is Percutaneous Umbilical Cord Blood Sampling (PUBS) Performed?
PUBS is an invasive procedure and as a result, it carries with it a relatively high risk of complications. Therefore, it is generally to be used in the case of high-risk pregnancies. A high-risk pregnancy is classified as such due to various factors that indicate a significantly increased likelihood of genetic defects. These may include:
- An advanced maternal age of 35 and over
- A previous pregnancy affected with chromosomal disorder
- Family history of genetic disorders (E.g. monogenic disease carrier status or balanced chromosomal translocation in a parent, history of X-linked or inborn metabolic disorders etc.)
- Abnormal results identified on a previously performed non-invasive procedure, such as ultrasound or maternal serum biochemistry screening
Steps of the Percutaneous Umbilical Cord Sampling Procedure
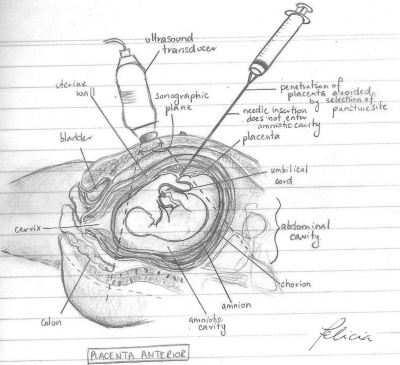
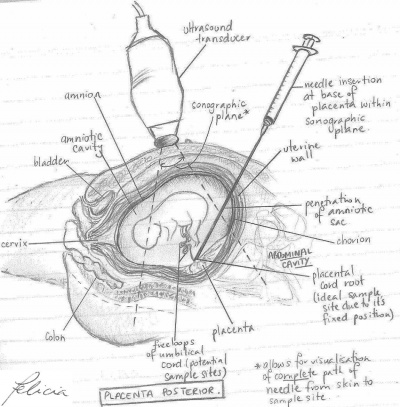
Percutaneous Umbilical Cord Sampling (PUBS) is the performed by the advancement of a needle within a ultrasound visual field to a targeted puncture site and consists of three fundamental steps.
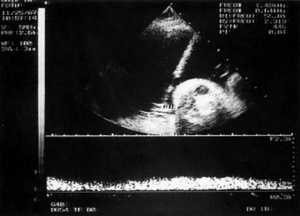
Step 1 - Imaging
An advanced imaging ultrasound is used to determine the location of where the umbilical cord inserts into the placenta. This ultrasound image is then used throughout the procedure in order to guide a thin needle through the abdomen and uterine wall of the mother and into the umbilical vein running through the cord.
Step 2 - Retrieval of Fetal Blood Sample
The needle is then inserted into the cord to retrieve a small sample of fetal blood. There are two main routes for the retrieval of fetal blood. The method used to perform the procedure is determined by the position of the placenta in the uterus and point of connection with the umbilical cord. The ideal sample site for PUBS is located at the root of the umbilical cord due to its stable fixed position which is less susceptible to disturbances caused by fetal movement compared to the free loops of the cord.
| Placenta Anterior | Placenta Posterior | |
| Description | Placenta attached to anterior wall of uterus - the needle is inserted straight into the umbilical cord without penetrating the amnion and amniotic cavity | Placenta located on posterior wall of uterus - the needle must travel through the amniotic sac to reach the umbilical cord. This may cause some temporary bleeding and cramps |
| Diagram |
There are two techniques that can be used when obtaining the sample: freehand and needle-guided. The choice of technique is dependent on a number of factors including the location of the cord root and the preferences of the physician performing the procedure.
1. Freehand - allows lateral readjustment of needle direction once within the uterus. A transducer is used to navigate the needle to the specific sample site and is the more preferred technique due to the increased range of movement
2. Needle-guided - involves the insertion of a separate needle straight into the targeted puncture site with the aid of the transducer, which forms a fixed passage through with a second smaller needle passes to retrieve the fetal blood. Despite permitting precise alignment of the needle tract with the vessel, the range of movement is limited to a single plane of travel
[19]
It is also important to note when performing PUBS, that if the mother is Rh–negative, Rh Immune-Globulin (RhIG) is administered to the mother in order to prevent the development of Rh incompatibility and further sensitization.
Step 3 - Sample Analysis
The fetal blood sample is sent to a lab where it is screened for genetic defects and other disorders. Prior to this, in order to confirm the sample obtained is fetal blood, the Kleihauer—Betke test performed. [21] The results for the test are usually available within 72 hours however under some circumstances, may take a few weeks to obtain the results. In the event of diagnosis, implementation of the most suitable procedure for management of the condition occurs or in extreme cases, the pregnancy is terminated.[22]
Percutaneous Umbilical Cord Blood Sampling Procedure Animation
ASSOCIATED RISKS AND COMPLICATIONS
As mentioned earlier, PUBS is an invasive diagnostic procedure which carries a number of risks and complications which are associated with a number of factors from procedure-related, experience of the staff performing the procedure to gestational age. However the risks involved in each case varies according to the indications of the procedure. For example, fetuses which are structurally abnormal or had growth deficiencies were found to be more susceptible to the associated risks and complications of PUBS.[23] Some of the main risks include:
- Transient bleeding of the umbilical cord at the puncture site is common and occurs in approximately 20% of cases. Often the bleeding spontaneously stops within a short time period (within 1 minute) while in a small number of cases, continued bleeding may prove fatal especially for those with blood disorders i.e. alloimune thrombocytopenia
- Transient fetal bradycardia - where the heart rate of the fetus falls below 100bpm is also a common complication (about 8% of cases) has been found to occur during or immediately after PUBS was performed. This occurs due to the puncture causing changes in the circulation and/or inducing reflexes and release of substances within the fetal circulation. In most cases, short term changes in fetal heart rate during PUBS has not reported long term fetal injury except for when there are underlying fetal disorders. Manual compression through the maternal abdomen is currently the preferred method of fetus revival [24]
- Failure to obtain a sample is also a complication occurring in a small number of cases which may require further PUBS procedures that could potentially increase the likelihood of fetal distress and preterm labour
- Preterm labour may be induced upon which the medical team overseeing the procedure must be prepared to perform an immediate emergency caesarean delivery
- Fetal loss reported to occur in less than 2% of cases is attributed to a number of factors including procedural time, gestational age (those earlier in pregnancy due to the size of the fetus are believed to be at higher risk of procedure-related injury), underlying medical conditions, expertise of the operator, pregnancy complications and fetal movement [25]
Links for futher information
DISORDERS AND ABNORMALITIES FOUND BY PUBS
Percutaneous Umbilical Blood Sampling, also known as Cordocentesis, as stated above is a pre-natal diagnostic test that is usually preformed to detect abnormalities such as Trisomy 21 (Down Syndrome), Trisomy 18 (Edwards Disease) and blood disorders for example Fetal Haemolytic Disease. However, PUBS may generally be performed to help diagnose any of the concerns listed below:
- Fetal anemia
- Malfunction of the fetus
- Isoimmunisation
- Fetal platelet count of the mother
- Fetal infections like rubella or toxoplasmosis
- Respiratory illnesses
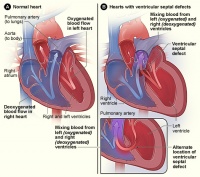
- Congenital heart defects
However one major disadvantage when comparing PUBS to other major testing methods for example Amniocentesis, is that PUBS does not help test for neural tube defects such as Spina Bifida
Table of Diseases and Disorders Percutaneous Umbilical Cord Blood Sampling Can Detect
| Disorder | Type of Disorder | Cause | Background Information | Recurrence | Picture |
|---|---|---|---|---|---|
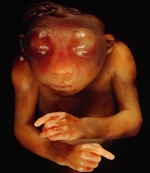
| Trisomy 21 | Genetic Disorder | The cause of Trisomy 21 is caused by the presence of all or part of an extra 21st chromosome. | Trisomy 21 also known as Down syndrome is associated with either major or minor impairments of cognitive ability and physical growth with a particular set of facial characteristics. Suffers tend to have a lower than average cognitive ability which often ranges from mild to moderate disabilities. The average IQ of a child with Down Syndrome is approximately 50.[26][27] | 1 for every 800 to 1,000 births | |
| Trisomy 18 | Genetic Disorder | Trisomy 18 is caused by the presence of three as opposed to two copies of chromosome 18 in a fetus or infant’s cell. | Also known as Edwards Disease or Trisomy E have increase incidence as the mother maternal age increases. The syndromes has an extremely low survival rate and this is a direct result of heart abnormalities, kidney malformations as well as other internal organ disorders caused by the syndrome itself. It is also the second most common autosomal trisomy after trisomy 21 also know as Down Syndrome that actually carries to term.[28] | 1 in 3,000 live births[29] | |
| Congenital Heart Defect | Structural Defect | Not Known | CHD is a defect in the structure of the heart and great vessels which is present at birth. There are many different type of CHD but most either obstruct blood flow within the heart or the vessels close by or it causes blood to flow through the heart in an abnormal pattern. It is one of the most common birth defect and is the leading cause of birth defect related deaths. Most CHDs don’t need treatment, but some are so complex they require medication or surgery.[30][31] | Approximately 9 in 1000 births.[32] | |
| Congenital Rubella Syndrome (CRS) | Infection – Viral | Congenital Rubella Syndrome can occur in a developing fetus of a pregnant woman who has contracted rubella during the term of her pregnancy | The classic triad for congenital rubella syndrome consist of:
However other manifestation of CRS may also include:
|
|
|
| Haemolytic Disease of the Fetus | Alloimmune condition | It develops in a fetus when IgG molecules (a type of antibody) produced by the mother passes through the placenta and subsequently begins attacking and breaking down the Red Blood Cells in fetal circulation. | The fetus can then develop problems such as reticulocytosis and anemia as a result of this disease. The severity of Haemolytic Disease ranges from mild to very severe, and can also lead to fetal death following heart failure (hydrops fetalis). When the disease is moderate or severe, many erythroblasts are present in the fetal blood and thus can be referred to as erythroblastosis fetalis.[34] | 10.2 cases per 10,000 total births |
REASONS FOR AND AGAINST THE USE OF PERCUTANEOUS UMBILICAL BLOOD SAMPLING
The reason for individuals to test or not to test using PUBS actually vary between each and every person with the individual's physicians also a playing a major role in the decision.
| For | Against |
|---|---|
|
|
Yet it is important to discuss the risk and benefits of testing thoroughly with the individual’s healthcare professional or physician. The physician should help the individual evaluate whether the benefits from the procedure's results are able to outweigh any risks associated with the procedure.
THE FUTURE OF PERCUTANEOUS UMBILICAL CORD SAMPLING
The use of PUBS as a pre-natal diagnostic tool has provided the opportunity to extend knowledge on the fetus by contributing to the understanding of human fetal physiology, metabolism and disease. However, like any other invasive diagnostic technique the procedure does carry some risks. As PUBS has only been available for two decades it can be said that it is one of the relatively new diagnostic techniques, andthe current associated research is mainly associated with finding non-invasive methods of fetal genetic diagnosis eliminating the risks associated with invasive procedures. The next section in this page will discuss the current research on PUBS.[35]
Fetal Cell in Maternal Blood
All nucleated fetal cells from the same individual contain identical genetic information. As a result of this finding, research efforts are currently focused on noninvasive method of fetal genetic diagnosis. An attractive potential population are the rare fetal that cross the placenta and circulate within the mother, The fetal cell types currently being studied include the trophoblast and nucleated erthyrocyte[36]. Genetic diagnoses that have already been made successfully in fetal cells isolated from maternal blood include both Down syndrome and Edwards Disease, Klinefelter syndrome and Rhesus D genotype[37]. On the basis of these encouraging preliminary results, a multicenter clinical evaluation designed to evaluate cytogenetic accuracy if fetal cells in maternal blood in comparison with that of percutaneous umbilical blood sampling. Results of this trial have shown a 78% detection rate for at least one aneuploid cell in maternal blood when the fetus has aneuploidy[38]. The major limitation in the clinical use of this technique appear to be the very small number of fetal cells present in most maternal blood samples.
Cell-Free Fetal DNA in Maternal Plasma and Serum
In 1997, Lo and associates first describe the circulation of large amounts of cell-free fetal DNA in maternal plasma and serum samples. A multitude of potential clinical application for the non-invasive diagnosis of the complication of pregnancy from this DNA has since been reported. These applications have largely focused on the quantitation of male fetal DNA in maternal plasma or serum samples and its associated increase in conditions such as fetal trisomy 21, preeclampsia, invasive placenta and preterm labor. In addition, qualitative detection of uniquely fetal DNA sequences in maternal plasma or serum has facilitated the non-invasive prenatal diagnosis of Rhesus D genotype, myotonic dystrophy and achondroplasia. It is likely that in the near future, non invasive diagnosis of fetal Rhesus D genotype will be preformed exclusively through the analysis of fetal DNA in maternal plasma or serum. The presence of amplified Rh D product in a sample from an Rh D-negative woman can come only from an Rh D – positive fetus.
USEFUL LINKS
Search Bookshelf Percutaeous Umbilical Cord Blood Sampling
Search Pubmed Now: Percutaeous Umbilical Cord Blood Sampling
WikipediaPercutaneous Umbilical Cord Blood Sampling
Further Information on Cordocentesis
GLOSSARY
Alloimmune Thrombocytopenia: A disease that affects fetuses and newborns. It involves genetic differences between the fetus and mother that may result in the expression of certain antigens by fetal platelets, not expressed by the mother.
Amniocentesis: The surgical insertion of a hollow needle through the abdominal wall and into the uterus of a pregnant female to obtain amniotic fluid especially to examine the fetal chromosomes for an abnormality and for the determination of sex.
Amnion: An extraembryonic membrane ectoderm and extraembryonic mesoderm in origin and forms the innermost fetal membrane, produces amniotic fluid.
Amniotic Cavity: The fluid-filled (amniotic fluid) extraembryonic coelom (cavity) formed initially by epiblast and then ectoderm and surrounding extraembryonic mesoderm. In humans, it forms the innermost fetal membrane, produces amniotic fluid expanding to fuse with the chorionic membrane during week 8 of development.
Amnion Sac: The amnion sac is the sac that is formed by the amnion, containing the amniotic fluid.
Anaemia: A condition in which the blood is deficient in red blood cells, in haemoglobin, or in total volume.
Choronic Villi Sampling: The biopsy of the chorion frondosum through the abdominal wall or by way of the vagina and uterine cervix at 10 to 12 weeks of gestation to obtain fetal cells for the prenatal diagnosis of chromosomal abnormalities - abbreviation CVS.
Chromosomal Translocation: A chromosome translocation is a chromosome abnormality caused by rearrangement of parts between non homologous chromosomes. A gene fusion may be created when the translocation joins two otherwise separated genes, the occurrence of which is common in cancer.
Congenital: Anything mainly diseases that are acquired during development in the uterus and not through heredity for example congenital syphilis.
Cordocentesis: The withdrawal of a sample of fetal blood from the umbilical cord by transabdominal insertion of a needle guided by ultrasound.
Cytogenetic: The branch of biology that deals with the study of heredity and variation by the methods of both cytology and genetics.
Cytogenic Analysis: The branch of genetics devoted to cellular constituents concerned in heredity, i.e. chromosomes.
Down syndrome: A congenital condition characterized by moderate to severe mental retardation, upward slanting eyes usually with epicanthic folds, a broad short skull, broad hands with short fingers, decreased muscle tone, and by trisomy of the human chromosome numbered 21 - called also trisomy 21.
Edwards Disease: A congenital condition that is characterized especially by mental retardation and by craniofacial, cardiac, gastrointestinal, and genitourinary abnormalities, is caused by trisomy of the human chromosome numbered 18, and is typically fatal especially within the first year of life.
Endocrinology: A science dealing with the endocrine glands.
Extra Uterine: Extrauterine means situated or occurring outside the uterus.
Fetal Bradycardia: An abnormally slow fetal heart rate, usually below 100 beats/min.
Fetal Haemolytic Disease: An alloimmune condition that develops in a fetus, when the IgG molecules produced by the mother pass through the placenta.
Fetoscopy: The examination of the pregnant uterus by means of a fiber-optic tube.
Haemorrhage: A copious discharge of blood from the blood vessels.
Hydropic: Characterized by swelling and taking up of fluid-used of a type of cellular degeneration.
Hysterotomy: A surgical incision of the uterus.
Intrauterine: Intrauterine means situated in, used in, or occurring within the uterus.
Isoimmunisation: The production by an individual of antibodies against constituents of the tissues of another individual of the same species (as when transfused with blood from one belonging to a different blood group).
Karyotype: The chromosomal characteristics of a cell as well as the chromosomes themselves or a representation of them.
Monogenetic Disease: An inherited disease which is controlled by a single pair of genes.
Placenta: The vascular organ in mammals except monotremes and marsupials that unites the fetus to the maternal uterus and mediates its metabolic exchanges through a more or less intimate association of uterine mucosal with chorionic and usually allantoic tissues permitting exchange of material by diffusion between the maternal and fetal vascular systems but without direct contact between maternal and fetal blood and typically involving the interlocking of finger like vascular chorionic villi with corresponding modified areas of the uterine mucosa.
Pre-Eclampsia: A serious condition developing in late pregnancy that is characterized by a sudden rise in blood pressure, excessive weight gain, generalized edema, severe headache, and visual disturbances and that may result in eclampsia if untreated.
Rhesus factor (Rh): A genetically determined protein on the red blood cells of some people that is one of the substances used to classify human blood as to compatibility for transfusion and that when present in a fetus but not in the mother causes a serious immunogenic reaction in which the mother produces antibodies that cross the placenta and attack the red blood cells of the fetus.
Rh Immune - Globulin: A specific immune globulin derived from human blood plasma containing antibody to the erythrocyte factor Rh0(D); used to prevent Rh-sensitization of Rh-negative females and thus prevents haemolytic anaemia of the fetus in subsequent pregnancies.
Rubella: Also known as the German measles in a pregnant woman may cause developmental anomalies in the fetus when occurring during the first trimester.
Spina Bifida: A neural tube defect marked by congenital cleft of the spinal column usually with hernial protrusion of the meninges and sometimes the spinal cord.
Toxoplasmosis: Infection with or disease that invades the tissues and may seriously damage the central nervous system especially of infants.
Umbilical Cord: (placental cord) The placental cord is the structure connecting the embryo/fetus to the placenta. It is initially extra-embryonic mesoderm forming the connecting stalk within which the placental blood vessels (arteries and veins) form. In human placental cords the placental blood vessels are initially paired, later in development only a single placental vein remains with a pair of placental arteries. This structure also contains the allantois, an extension from the hindgut cloaca then urogenital sinus. Blood collected from the placental cord following delivery is a source of cord blood stem cells.
Umbilical Vein: The vein that passes through the umbilical cord to the fetus and returns the oxygenated and nutrient blood from the placenta to the fetus.
Ultrasound: A non-invasive technique for visualizing and prenatal diagnosis of several features of development including: follicles in the ovaries, the gestational sac, fetus in the uterus, fetal parameters, and the placenta. The technique uses high-frequency sound waves that are reflected off internal structures.
Uteroplacental: Uteroplacental means of or relating to the uterus and the placenta for example uteroplacental circulation.
REFERENCES
- ↑ http://www.mombaby.org/index.php?c=-1&s=14&p=45
- ↑ http://en.wikibooks.org/wiki/Handbook_of_Genetic_Counseling/Percutaneous_Umbilical_Blood_Sampling
- ↑ http://www.labtestsonline.org/understanding/wellness/second_cordo.html
- ↑ http://www.americanpregnancy.org/prenataltesting/percutaneousumbilical.html
- ↑ http://www.umm.edu/pregnancy/000229.htm
- ↑ http://www.lpch.org/DiseaseHealthInfo/HealthLibrary/hrpregnant/fbs.html
- ↑ A short History of Amniocentesis, Fetoscopy and Chorionic Villus Sampling, Dr. Joseph Woo. http://www.ob-ultrasound.net/amniocentesis.html
- ↑ <pubmed> 6881235</pubmed>
- ↑ <pubmed> 14277637</pubmed>
- ↑ <pubmed> 5913854 </pubmed>
- ↑ <pubmed> 4653838 </pubmed>
- ↑ <pubmed> 4842594</pubmed>
- ↑ <pubmed> 7397075 </pubmed>
- ↑ <pubmed> 6110859 </pubmed>
- ↑ <pubmed>8907774</pubmed>
- ↑ <pubmed>18292841</pubmed>
- ↑ <pubmed>20193481</pubmed>
- ↑ <pubmed>18292841</pubmed>
- ↑ <pubmed>8739583</pubmed>
- ↑ Henderson, J, Weiner, C, Glob. libr. women's med.,(ISSN: 1756-2228) 2008; DOI 10.3843/GLOWM.10212
- ↑ <pubmed>16530195</pubmed>
- ↑ http://adam.about.com/encyclopedia/Percutaneous-umbilical-cord-blood-sampling-series.htm
- ↑ <pubmed>9793976</pubmed>
- ↑ Henderson, J, Weiner, C, Glob. libr. women's med.,(ISSN: 1756-2228) 2008; DOI 10.3843/GLOWM.10212
- ↑ <pubmed>16530195</pubmed>
- ↑ http://www.merck.com/mmhe/sec23/ch266/ch266b.html#sec23-ch266-ch266b-420
- ↑ http://en.wikipedia.org/wiki/Down_syndrome#cite_note-weiss-3
- ↑ http://en.wikipedia.org/wiki/Trisomy_18
- ↑ http://www.nlm.nih.gov/MEDLINEPLUS/ency/article/001661.htm#Causes,%20incidence,%20and%20risk%20factors
- ↑ http://www.merck.com/mmhe/sec23/ch265/ch265b
- ↑ http://en.wikipedia.org/wiki/Congenital_heart_defect
- ↑ <pubmed>9793976</pubmed>
- ↑ http://en.wikipedia.org/wiki/Congenital_rubella_syndrome
- ↑ http://en.wikipedia.org/wiki/Hemolytic_disease_of_the_newborn
- ↑ http://www.glowm.com/?p=glowm.cml/section_view&articleid=212#ref
- ↑ <pubmed> 2333281</pubmed>
- ↑ <pubmed>7485357</pubmed>
- ↑ <pubmed> 12124698</pubmed>
- ↑ http://www.nlm.nih.gov/medlineplus/mplusdictionary.html
2010 ANAT2341 Group Projects
Project 1 - Ultrasound | Project 2 - Chorionic villus sampling | Project 3 - Amniocentesis | Group Project 4 - Percutaneous Umbilical Cord Blood Sampling | Project 5 - Fetal Fibronectin | Project 6 - Maternal serum alpha-fetoprotein | Group Assessment Criteria
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, February 26) Embryology 2010 Group Project 4. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Group_Project_4
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G