2010 Group Project 1
Ultrasound
Introduction
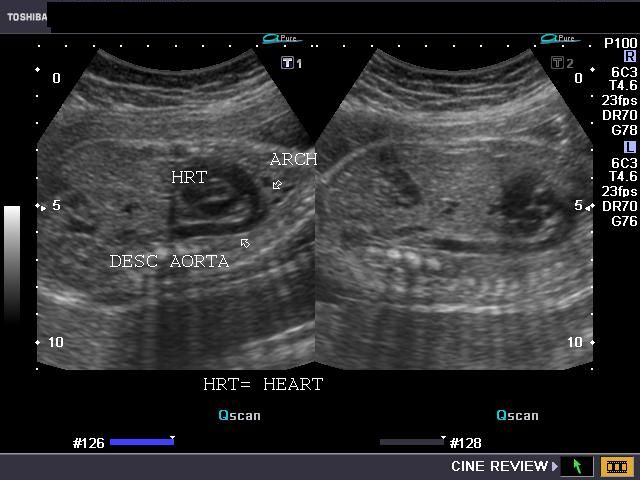
Today, ultrasound is known to almost everyone in the developed world as the "normal" prenatal examination that pregnant women undergo to assess the development of their pregnancy. Ultrasound scans reveal the size and position of the fetus, its sex, approximate gestational age, the number of fetuses, and generally useful information to chart the progress of the growing fetus. Ultrasound can also be of great help in the prenatal diagnosis of structural abnormalities, revealing before birth physical developmental defects such as cleft lip or abnormal limb growth and allowing parents and physicians to prepare for these situations and make early decisions about important issues such as termination and treatment.
History Time Line
Interest and research into ultrasound began as early as the 1700’s and has been developing continuously even until today. It has transformed from a simple piece of machinery that was mainly used for navigation in World War I and as a powerful locator for ships and seafaring vessels to a more complex machine in modern times, and is now used as a main prenatal and medical diagnostic tool. Generating heat for patient therapy was initially the main use of ultrasound in the medical field, but it was later developed into a therapeutic tool (e.g. using vibrations to stimulate regrowth of bone in immobilised fractures) and more recently has become important in prenatal diagnosis, as well as in the diagnosis of diseases and injuries. [1]
The following time line briefly highlights some of the important discoveries in relation to ultrasound.
- 1794- Lazzaro Spallanzani proposed that bats use hearing rather than sight to move with the aid of "high-frequency ultrasound"
- 1826- Jean Daniel Colladon successfully measured the speed of sound underwater
- 1880- Pierre Curie and Jacques Curie described the piezoelectric effect which lead to the creation of the transducer
- 1914- Reginald Fessenden created the first operating sonar system to detect icebergs underwater
- 1920- Paul Langévin invented the "hydrophone" - the first successful transducer
- 1938- Raimar Pohlman demonstrated the therapeutic uses of ultrasound by creating ultrasonic physiotherapy
- 1942- Lynn and Putnam destroyed brain cells using ultrasound waves
- 1963- Donald and MacVicar detected the gestational sac of the embryo using ultrasound
- 1972 -Hugh Robinson used ultrasound to detect fetal heart beats and crown-to-rump length
- 1973- George Radovanovitch and David Carpenter created grey-scale images of prenatal embryos
- 1965- Walter Krause and Richard Soldner created a real time scanner which could capture 15 images per second
- 1984- Kazunori Baba first invented 3-D ultrasound
- 1996- Nelson researches on 4-D (motion 3-D) fetal echocardiography[1]
Link for more history | History of Ultrasound
1970s
Lazzaro Spallanzani discovered one of the earliest forms of high-frequency sound by experimenting on bats. He claimed that bats use their hearing rather than sight for navigating which became the basic backbone for other researchers to investigate ultrasound. His research work was then used later by other scientist to create a high-frequency sound that is non-audible to humans.
1980s
Jean Daniel successfully used a bell to obtain the most accurate speed of sound underwater which later became the basis of the ultrasound amplifier. However, in the late 80’s Pierre Curie and Jacques Curie discovered the “piezoelectric effect”. The piezoelectric effect is found in some types of crystal that, when mechanically stressed, will produce electric potentials. These findings were very important in the creation of the ultrasound transducer.
Early 1900s
After the Titanic sank there was a lot of research and many inventions were created to find the missing ship. The popularity of the research lead to first sonar system being produced by Reginald Fessenden. Reginald Fessenden then created the first working ultrasound machine. Although the machine used low frequency sound it was a major step as the idea of using a receiver was brought about. The machine was able to detect icebergs underwater from up to 2 miles away, laying the foundation for the ultrasound machine. Paul Langevin then created a high-frequency machine called hydrophone. The machine converted sound into electrical energy and was also used to detect submarines and icebergs and had a successful transducer.
Mid 1900s
In the 1990s ultrasound was first used to treat diseases rather than diagnose them. Raimar Pohlman developed ultrasonic imaging by using the ultrasound waves for therapy and physiotherapy. The research was continued by Lynn and Putnam who claimed that ultrasound waves had the ability to destroy brain cells and tranformed this research into the earliest real therapeutic use for ultrasound in biology. The ultrasound was further used to destroy parts of the brain and to treat Parkinson diseases.
Late 1900s
The research and development into ultrasound and its uses continued rapidly in the late 1990s. Its uses spread from general medical therapy to prenatal diagnosis as a result of Donald and MacVicar detecting the gestational sac of embryo and the measurement of crown-to-rump length which is crucial for modern diagnosis and of George Radovanovitch and David Carpenter making prenatal diagnosis more easy to visualise by creating a greyscale ultrasound machine. Ultrasound technology was then further developed by incorporating the technology to capture many still images per minute, as well as the development of 3- and 4-dimensional ultrasound machines. 3-D ultrasound is now increasingly used for prenatal diagnosis since it allows better visualisation of external structural defects and positions of the baby and placenta. Ultrasound is still developing today, trying for better resolution and improved technology.
How It Works
The basic principle of ultrasound is similar to that of sonar – that is, sending out pulses of high-frequency sound waves, receiving back the echoes of those waves after they bounce off surrounding materials, and constructing a picture of those materials from the received sounds. In medical ultrasound, or sonography, pulses of ultrasound are repeatedly sent into the body where they bounce off the edges of organs and tissues, relaying that anatomical information back to the ultrasound machine. [2]
There are three main elements in an ultrasound system: the transducer, the machine and the recording devices [3].
The Transducer
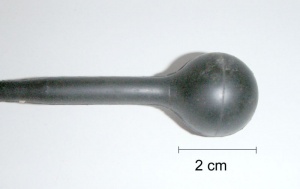
The transducer is the piece of equipment in contact with the patient. It emits the ultrasound pulses and receives the echoes of those pulses. Information about the patient’s tissues is generated by calculating the time it takes for the ultrasound pulses to scatter and bounce off those tissues and travel back to the transducer. The ultrasound waves will take longer or shorter amounts of time to travel through different tissues depending on their properties.
Since air diminishes the integrity of the ultrasound signals (the ultrasound can bounce off even a thin layer of air, almost completely preventing the penetration of the ultrasound into the patient’s tissues), a medium such as a water-soluble gel is applied between the transducer and the patient’s skin to improve the interface between the two. There are several kinds of transducers producing different kinds of ultrasound images, discussed below. Transducers can be non-invasive (for prenatal diagnosis, pressed against the woman's pelvis or abdomen) or they can be invasive (transvaginal transducers, for example, are inserted into the vagina to obtain better views of the ovaries, fallopian tubes, uterus, and surrounding structures).
Within the transducer are elements made of silicon crystals. The pulses of ultrasound are created using the piezoelectric effect – when silicon crystals experience electrical impulses they mechanically deform on a microscopic level, producing high-frequency sound waves. Returning sound waves (echoes) will similarly deform the silicon crystals, and these deformations are converted to electrical impulses which are then sent to the ultrasound machine for processing. Different kinds of transducers will produce different kinds of images, or scans. High-frequency transducers (5MHz or greater) give better resolution of images, but low frequency transducers penetrate deeper into tissues and so provide images of deeper structures. [4]
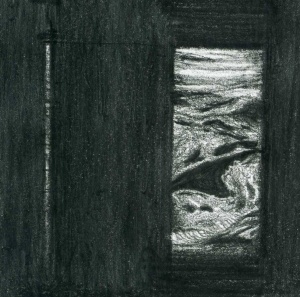
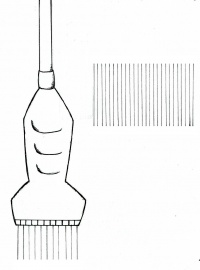
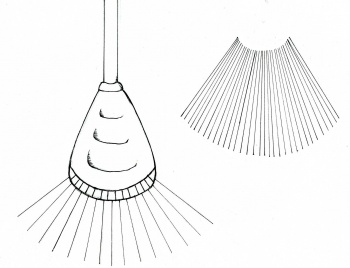
Sending one ultrasound pulse into the body will generate a line of dots – this represents one line of echo information, or one scan line. Not all of that pulse bounces back off one single anatomical structure; instead, most of the pulse continues through to deeper structures where some of the pulse bounces back from each structure it passes through. This is what generates the line of dots representing an internal view of the patient. Since the echoes of a single pulse generate one scan line of information, generating several scan lines next to one another in an ordered sequence will generate a cross-sectional image of the patient (see the diagram on the right). This way of directing pulses through the tissues is termed “scanning” or “sweeping”. Scanning is performed quickly and automatically by an “array” of organised group of transducer elements, creating many still images or frames which are viewed in sequence, like a movie. Thus, ultrasound exams are performed in real-time. [5]
Different transducers have different arrays of piezoelectric elements, and produce a variety of different scans or images:
The Ultrasound Machine and Recording Devices
The ultrasound machine itself is comprised of the computer hardware and software needed to convert the signals picked up by the transducer into an image that can be viewed. The image is in greyscale, using various shades from black to white to indicate different tissues and tissue features.
The other basic part of the ultrasound system is the recording equipment – that is, a range of devices such as multiformat cameras, video printers and video recorders used to store information from the patient’s examination.
So far, what has been explained are the basic principles of how a normal 2D ultrasound image is generated. There have been are, however, some developments in ultrasound technology that allow the generation of slightly different images to the normal 2D ones, providing more diagnostic information. These are the Doppler ultrasound and 3D ultrasound imaging.
Link to more ultrasound images | Ultrasound Images
Doppler Ultrasound
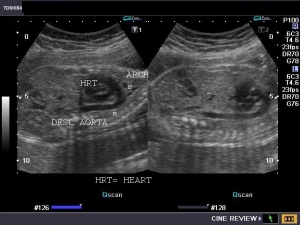
Doppler ultrasound utilises the Doppler effect to view moving structures, such as the flow of blood through major blood vessels of the heart. The Doppler effect refers to the change in frequency of a wave relative to the motion of the wave source and the observer. In a Doppler ultrasound, sound waved are reflected from moving structures with a shift in frequency of those sound waves proportional to the velocity of the moving structure.[6]
Continuous-wave Doppler ultrasound detects signals from anything moving in the path of the pulse, and cannot distinguish well between separate vessels. Pulsed Doppler ultrasound uses a pulse in a thin, focused beam and detects signals from only one point in that beam, allowing the imaging of specific vessels. Colour Doppler imaging is a type of pulsed Doppler ultrasound where software is used to overlay the greyscale image with colours representing frequency shifts. Different colours are assigned to indicate movement towards or away from the transducer. [7][8]
Link to more ultrasound images | Ultrasound Images
Link to video of the Doppler Effect | Assignment Discovery: the Doppler Effect
3D Ultrasound
Three-dimensional ultrasound images are produced in one of several ways. The first is to have several arrays of 2D transducers working together to collect a series of 2D cross-sections and combine these into a 3D image, though this can be difficult. 3D ultrasound images can also be made with the use of arrays of 1D transducers to create 2D B-scan images of known areas in 3D space. The 1D arrays can either by swept across the patient by machine or by the technician. 3D ultrasound images are particularly useful for visualising the volumes of structures, and better viewing complex 3D structures. However, even today it is mostly 2D ultrasound that is used, with 3D ultrasound only used in select applications. [9][10]
Link to more ultrasound images | Ultrasound Images
Link to a review of 3D ultrasound imaging | Three-dimensional ultrasound imaging
Current Uses in Prenatal Diagnosis
Ultrasound imaging is an effective non-invasive technique currently used in three main capacities in terms of prenatal diagnosis: guiding invasive tests, detecting abnormalities in at-risk patients, and as a widely-used screening test for abnormalities in the general population during the second trimester of pregnancy.
Guiding Invasive Procedures
Invasive procedures for detecting abnormalities such as amniocentesis and chorionic villus sampling have become safer with the guidance of ultrasound, as the physician is no longer operating “blind”. The ultrasound machine can show in real-time the movement and position of the needle, reducing the risk of damage to surrounding anatomical structures. [11]
Furthermore, if these invasive tests guided by ultrasound reveal that the patient is a high-risk for fetal abnormalities, a high resolution ultrasound can then be employed to attempt to visually diagnose potential structural abnormalities.
Diagnosis of Abnormalites
Ultrasound can be used to detect the three main groups of fetal abnormalities: neural tube defects, chromosomal defects and congenital heart abnormalities. [12]
Neural Tube Defects
These are a relatively common assembly of structural abnormalities, some of which are spina bifida, anencephaly, and encephalocoele. If serum examinations of the maternal alpha-fetoprotein level reveal it to be high ultrasound imaging can be used to guide the needle for invasive but more specific tests such as amniocentesis, as well as to define the gestational age of the fetus. [13] Ultrasound imaging of the cranium is also a diagnostic test for neural tube defects, and rates detection of spina bifida with ultrasound have been relatively high with high-quality ultrasound systems. [14] In open neural tube defects, decreased hydrostatic pressure in the spinal canal causes the cerebellum to take on a “V”-like shape as well as causing ‘bossing’ of the frontal bones (the ‘lemon sign’), and in some cases dilation of ventricles. [15] Ultrasound imaging of the spine in transverse, coronal and sagittal planes may also reveal defects, including closed defects which may not lead to the diagnostic high alpha-fetoprotein levels in the amniotic fluid.
Women at high risk for neural tube defects (those with a family history, Type 1 Diabetes, and those on some medications) should always be referred for prenatal ultrasound examination to screen for the defects.
Chromosomal Abnormalities
Chromosomal anomalies appear in approximately 1% of pregnancies lasting beyond 20 weeks, a great number of which are not associated with any significant structural defects, and about 40% of miscarriages are linked to chromosome abnormalities in the fetus[16]. Autosomal trisomies contribute to about half of that 40%, with the most common being trisomies 13, 18 and 21. Where trisomies 13 and 18 are generally lethal trisomy 21 or Down Syndrome is not; however, it does cause some structural malformation and impaired intellectual ability.
| Trisomy 21 | Trisomy 18 | Trisomy 13 |
|---|---|---|
| Duodenal atresia | Exomphalos | Craniofacial defects in the midline of the face |
| Significant cardiac defects (such as atrioventricular canal defects) | Enlargement of cisterna magna |
There are two main clusters of symptoms caused by autosomal trisomies that can be detected with ultrasound, major and minor signs. The major signs have a high predictability for trisomies, but are not often seen. Minor signs are fairly indicative of trisomies but can also be seen in unaffected fetuses.
| Major Signs | Minor Signs |
|---|---|
| Cystic hygroma (congenital lymphatic lesion) | Brachycephaly ("flat head") |
| Significant cardiac defects (such as atrioventricular canal defects) | Cysts of choroid plexus |
| Duodenum without orifice or absent | Shortened humerus and/or femur |
| Exomphalos (weakening of the abdominal wall at the join of the umbilicus) | Clinodactyly (curvature of the 5th finger away from the midline) |
| Ventriculomegaly | Nuchal fold larger than 6 mm |
| Craniofacial defects in the midline | Absent/hypoplastic fifth middle phalanx |
| Widely-spaced toes | |
| Pyelectasis (dilation of the pelvis of the kidney) |
Congenital Heart Abnormalities
Relatively common abnormalities, these could affect up to 1% of fetuses. Though a great number are asymptomatic, some – like a hypoplastic left ventricle – can be life-threatening. With the introduction of Doppler ultrasound, physicians now can study the flow of blood in the fetus, which has had a significant impact on the prenatal diagnosis of heart valve defects – if blood can be seen passing through valves that should be sealed closed, that indicates an abnormality, and vice versa.
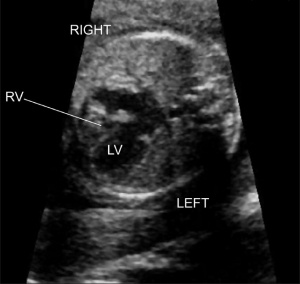
To diagnose heart defects, the ultrasound examiner first obtains a single view of the four chambers of the heart. One problem is that some of these defects may not be visible at 18-20 weeks, the general time for an ultrasound screening examination to be administered. If a defect is detected, the fetus is often also tested for chromosomal abnormalities, since the two are often linked. [19]
| Pulmonary or aortic atresia | A malformation of the pulmonary or aortic valves in which the opening fails to form, meaning the valves obstruct the blood flow to the lungs or aorta |
|---|---|
| Double inlet ventricle | The left or right ventricle has two separate atrioventricular openings and valves |
| Ebstein anomaly | The improper placement of the tricuspid valve further toward the apex of the heart, resulting in a large right atrium and small right ventricle |
| Large ventricular septal defect | A large hole in the septum between the left and right ventricles of the heart, resulting in shunting of blood from the left to the right ventricle; can be fatal |
| Atrioventricular canal defect | A malformation of the atrioventricular septum of the heart |
Other Abnormalities
Ultrasound can be used to detect a vast number of structural defects in any area of the fetal anatomy.
| Facial defects | Cleft lip | This can also be more clearly visualised with the use of 3D ultrasound imaging to indicate the extent of the malformation[22] |
|---|---|---|
| Intracranial abnormalities | Hydrocephalus | Indicated by the transverse measurement of the atrium of the lateral ventricle being larger than 1cm |
| Thoracic abnormalities | Diaphragmatic hernia | Visible in a sagittal section, where an abdominal organ has herniated through the diaphragm to sit in the thoracic cavity, can compress lung/s |
| Gastrointestinal defects | Gastroschisis | The intestines and/or abdominal organs develop outside the abdomen, visible upon examination as a mass on the abdomen separate from the umbilical cord |
| Skeletal defects | Osteogenesis imperfecta | A brittle bone syndrome which may be recognised by ultrasound imaging showing shortening and bowing of long bones (femurs, humerus and tibia) |
Normal Prenatal Screening
Ultrasound scans are widely used in the second trimester (weeks 18-20) to screen for any structural abnormalities in the developing fetus. This is useful for detecting abnormalities in fetuses in patients considered low-risk (e.g. with no history of affected children or no family history of birth defects) who would not otherwise consider that their fetus may have a physical developmental issue.
It is important to note that whilst in the diagnosis of fetal abnormalities in patients suspected of having said abnormalities, ultrasound imaging can be more specific in that the sonographer or sonologist knows that they are looking for, and be more specific in their examination (i.e. focus on particular anatomical areas, collecting several images of the structure in question). As a screening tool, however, less obvious defects like small ventricular septal defects are easy to miss during a broad, non-focused examination, even if the ultrasound technician does obtain an image of the chambers of the heart. [23]
Risks and Regulations
Epidemiological studies have not indicated any identifiable risks associated with the use of ultrasound as a diagnostic tool. Animal studies have indicated that only at intensities higher than expected in pertinent tissues during ultrasound imaging are any bioeffects evident. The World Health Organization has given the statement that, “the benefits of this imaging modality far outweigh any presumed risks”[24][25] As there is currently no known risk but there are known benefits of the procedure, it is considered safe, but a conservative approach should still be taken to ensure that ultrasound exams are not given unnecessarily or excessively. [26]
There is however a risk of misdiagnosis by the ultrasound technician, which could cause undue parental anxiety. This can, for the most part, be avoided by ensuring ultrasound operators are all sufficiently trained and experienced. [27]
Advantages and Disadvantages of Ultrasound Imaging for Prenatal Diagnosis
| Advantages | Disadvantages |
|---|---|
| Non-invasive | Quality of exam and diagnosis can depend on the skill of the examiner, as exam is in real-time |
| Relatively inexpensive (in Australia) | Images may not be obtainable or clear due to position of the fetus |
| Early diagnosis can mean prompt treatment upon birth | Misdiagnosis can create unnecessary parental anxiety |
| Blood flow can be imaged with Doppler ultrasound, which can diagnose cardiovascular defects prenatally | Ultrasound waves have a penetration depth limit and cannot always image all angles of the fetus |
| Ultrasound exams are not currently associated with any discernible risk to the patient or fetus |
Current Research and Future Uses in Prenatal Diagnosis
Ultrasound is currently being used in various fields for multiple purposes such as diagnosing major diseases of fetused. It is also used to detect the placental location and “vascular system”. Moreover, recent discoveries have made the mother-fetus interaction able to be visualised by being able to see the development of placenta and the changes in blood vessels during pregnancy [28]. Ultrasound is an important prenatal diagnostic tool because of its visual capability, making it possible to measure crown-rump length for growth and enable physicians to see both superficial and deep layers of the embryo. With modern 3-D ultrasound technology detection of morphological changes presented diseases is easily recognisable.
Another example of current research would be using ultrasound to detect the early FASD (fetal alcohol spectrum disorder) symptoms in alcoholic mothers by examining the abnormal facial features of the fetus for better prevention and treatment, since it is known to result many birth defects such as impaired growth and cognitive dysfunction[29].
Previously all an ultrasound machine could do was detect the presence of a heart-beat, however the recent research shows that cardiac defects could be detected via ultrasound from as early as week 11-13 so that there would be minimal complications for both the mother and the child.[30]
In addition, there is also a media report that claimed 3-D ultrasound shows “complex behaviors” which would be considered impossible for a neonate. These actions include yawning, sucking, smiling, crying and scratching in the womb. The findings were considered a powerful psychological tool to study behaviours in unborn infants.[31]
For more information about the Report|BBC news
In terms of further uses, researches are aiming to develop a better resolution and more interactive ultrasound machines for better prenatal diagnosis and treatment. Today, many more diseases have been detected via ultrasound than were able to be detected previously, hence when ultrasound systems are more developed and have greater functions, fetal abnormalities would be quickly detected and potentially could be greatly reduced which would not only help save lives, but also lead to better health care.
Links For Further Reading
More ultrasound images | Ultrasound Images
A review of 3D ultrasound imaging | Three-dimensional ultrasound imaging
History of ultrasound | History of Ultrasound
An article on ultrasound diagnosis and chromosomal abnormalities | The ultrasound detection of chromosomal anomalies
Glossary
Atresia: A situation in which an orifice or channel of the body is closed or not present
Atrioventricular canal defect: A malformation of the atrioventricular septum of the heart
B-scan: A way to map the body or an area of the body using a sensing device
Bioeffects: Adverse biological effects
Brachycephaly: Or “flat head”, when the coronal sutures fuse before they should, resulting in a reduced anteroposterior diameter of the cranium
Clinodactyly: Curvature of the 5th finger away from the midline across the 4th digit
Cystic hygroma: A lymphatic lesion usually present in the posterior triangle of the neck; generally benign but sometimes disfiguring
Diaphragmatic hernia: When abdominal organs herniated through the diaphragm to lie in the thoracic cavity
Doppler ultrasound: A kind of imaging utilising the Doppler principle to examine moving structures like blood flow
Double inlet ventricle: The left or right ventricle has two separate atrioventricular openings and valves
Ebstein anomaly: The improper placement of the tricuspid valve further toward the apex of the heart, resulting in a large right atrium and small right ventricle
Exomphalos: A weakness of the abdominal wall where the umbilicus joins it
FASD: Fetal alcohol spectrum disorder; a collection or spectrum of defects caused by the consumption of alcohol by the mother during pregnancy
Gastroschisis: Intestines and/or abdominal organs develop outside the body
Hydrocephalus: Colloquially known as “water on the brain” this is a condition where large amounts of cerebrospinal fluid collect in the ventricles of the brain, which can lead to increased intracranial pressure
Hypoplastic left ventricle: A condition where the left ventricle is severely underdeveloped; often fatal
Large ventricular septal defect: A large hole in the septum between the left and right ventricles of the heart, resulting in shunting of blood from the left to the right ventricle; can be fatal
Linear image: A rectangular image produced by a transducer with elements next to each other, giving off ultrasound pulses in parallel lines
Modified sector scan: A fan-shaped image with a curved top produced by a transducer with elements next to each other that also emit pulses in different directions
Osteogenesis imperfecta: A genetic brittle bone syndrome caused by mutations in genes for procollagens
Piezoelectric effect: When silicon crystals experience electrical impulses they mechanically deform on a microscopic level, producing high-frequency sound waves
Pulmonary or aortic atresia: A malformation of the pulmonary or aortic valves in which the opening fails to form, meaning the valves obstruct the blood flow to the lungs or aorta
Pulse-echo technique: A technique in ultrasound where short pulses of ultrasound are emitted into the area to be studied, and echoes are received and interpreted to give information about the internal anatomical structures by calculating the time taken for the ultrasound echoes to return to the transducer
Pyelectasis: Dilation of the pelvis of the kidney
Scan line: The line of dots representing the information from one pulse of ultrasound
Sonographer: A trained ultrasound technician
Sonography: Medical anatomical imaging using ultrasound
Sonologist: A medical practitioner who is a trained ultrasound technician
Sector scan: A fan-shaped image produced by a transducer with ultrasound pulses emitting from the same point but in different directions
Three-dimensional ultrasound: A type of imaging where a 3D rendering of the fetus in the womb is produced by one of several means
Transducer: The part of the ultrasound apparatus that is in contact with the patient; it emits the pulses and receives the echoes of ultrasound
Trisomy: Having three copies of a chromosome due to incorrect meiosis; can be fatal or cause developmental deformities or impairments
Ventriculomegaly: When the ventricles of the brain are dilated and enlarged
References
- ↑ 1.0 1.1 Woo, Joseph (2002) A short history of the development of ultrasound in obstetrics and gynecology. Accessed 13/9/2010<http://www.ob-ultrasound.net/history1.html>
- ↑ Kremkali, F.W. (2006) Diagnostic Ultrasound Principles and Instruments (7th ed.) St Louis: Saunders Elsevier. pp3-5
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 28-31
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 28-31
- ↑ Kremkali, F.W. (2006) Diagnostic Ultrasound Principles and Instruments (7th ed.) St Louis: Saunders Elsevier. pp3-9
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 30
- ↑ Kremkali, F.W. (2006) Diagnostic Ultrasound Principles and Instruments (7th ed.) St Louis: Saunders Elsevier. pp 185-186
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 30
- ↑ Kremkali, F.W. (2006) Diagnostic Ultrasound Principles and Instruments (7th ed.) St Louis: Saunders Elsevier. pp. 6
- ↑ <pubmed>20349815</pubmed>
- ↑ Anderson, J.C. (1995) Amniocentesis, chorionic villus sampling and fetal blood sampling. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 28-31
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 31
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 31
- ↑ Tyrell, S., Howell, D., Bark, M. Allibone, E. and Lilford, R.J. (1988) Should alpha-fetoprotein estimation be carried out in centres where ultrasound screening is routine? A sensitivity analysis approach. ‘’American Journal of Obstetrics and Gynecology’’ 158: 1092-9
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 32
- ↑ Young, I.D. (1992) Inceidence and genetics of congenital malformations. In “Prenatal Diagnosis and Screening,’’ ed. DJH Brock, C.H Rodeck and M.A. Ferguson-Smith, pp. 171-87. Edinburgh: Churchill Livingstone.
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 40-43
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 36
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 40
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 42
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 41-50
- ↑ Wayne, C., Cook, K., Sairam, S., Hollis, B., Thilaganathan, B. (2002) Sensitivity and accuracy of routine antenatal ultrasound screening for isolated facial clefts. ‘’British Journal of Radiology,’’ 75: 584-589
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 32
- ↑ World Health Organization: ‘’Environmental health criteria 22: ultrasound’’, Geneva, 1982, The Organization.
- ↑ World Health Organization: Ultrasound. In Nonionizing radiation protection, ed 2, Geneva, 1989, The Organization.
- ↑ Kremkali, F.W. (2006) Diagnostic Ultrasound Principles and Instruments (7th ed.) St Louis: Saunders Elsevier. pp332-333
- ↑ Ellwood, D.A. (1995) The Role of Ultrasound in Prenatal Diagnosis. In Trent, R.J. (Ed.), Handbook of Prenatal Diagnosis. Cambridge, England: Cambridge University Press, pp. 29
- ↑ <pubmed>20034427</pubmed>
- ↑ <pubmed>19444822</pubmed>
- ↑ <pubmed>16570262</pubmed>
- ↑ BBC, Scans uncover secrets of the womb. Accessed 13/9/2010<http://news.bbc.co.uk/2/hi/health/3846525.stm>
2010 ANAT2341 Group Projects
Project 1 - Ultrasound | Project 2 - Chorionic villus sampling | Project 3 - Amniocentesis | Group Project 4 - Percutaneous Umbilical Cord Blood Sampling | Project 5 - Fetal Fibronectin | Project 6 - Maternal serum alpha-fetoprotein | Group Assessment Criteria
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2026, March 1) Embryology 2010 Group Project 1. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Group_Project_1
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G