2010 BGD Practical 3 - Oogenesis and Ovulation
Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 | Quiz
Introduction
This page covers gametogenesis within the ovary. With the help of the tutors and other students you will work your way through identifying features described in the text.
Begin by looking at the ovary and the formation of the follicle containing the egg which matures and is released upon ovulation. The images are arranged in series so that progressive stages of the maturing follicle can be seen. The final image on this current page is a link to a movie showing follicle development and ovulation. Use the series of images of the cat ovary below to identify the key features described in the associated text.
Note: This should be a revision of the Ovary Histology Practical you have already completed. If you have trouble with the terms, there is a glossary at the bottom of each page.
Practical Audio
|
BGD Cycle A 2010 Audio - Dr Mark Hill Monday 12th May 2010 12-2pm G2G4.
listen Part 2 | download (1.7 Mb MP3 14:16) |
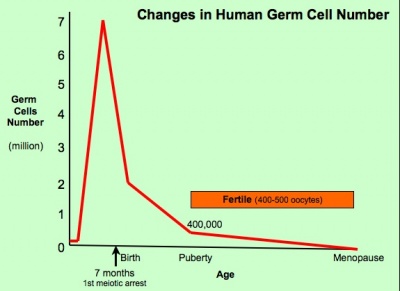
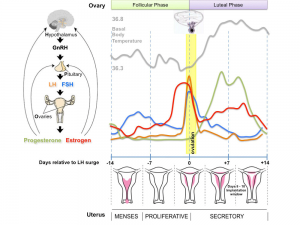
Oogenesis
The graph below shows the changes in human germ cell numbers in the ovary with age, peaking at about 7 million (occuring in early fetal development) and then decreasing by apopotic cell death. At puberty there remain only about 400,000 and only about 10% of these will be released through reproductive life. (More? Menstrual Cycle)
(Based on data from: Hassold, etal., Environ Mol Mutagen 1996. 28: 167-175)
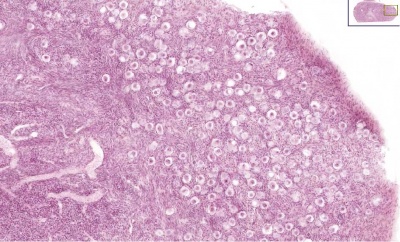
Whole Ovary
Ovary (cat, cross-section) showing histology and maturation of follicle.
Image (low magnification) showing cortical primordial follicles with primary (preantral) and secondary (antral) follicles lying deeper. Mesovarium at lower right and blood vessels in medullary region.
At this magnification, the overall organization of the ovary can be observed, cortex/medulla organization and arrangement of the maternal blood vessels, but few specific follicle details can be seen.
The next image is of the ovarian cortical region.
Ovary Cortex (low power)
Ovary cortex showing primordial follicles.
At the top of the image, is the outside of the ovary.
The thick connective tissue outer layer is the tunica albuginea. Over which a single layer of cells called the germinal epithelium (not visible) cover the surface of the ovary.
The next layer contains the earliest primordial follicles, single cells with pale cytoplasm and darkly stained nuclei.
The next layer contains many growing follicles at various stages of maturity and development. There is also evidence of degeneration as atretic follicles.
At the bottom of the image, is the medullary region of the ovary. Note the large number of maternal blood vessels which are the circulatory conduits for the estrogens and progesterones produced by the theca surrounding the ovarian follicles.
Note: [[G#germinal epithelium|germinal epithelium], tunica albuginea, primordial and atretic follicles. Note larger preantral follicle with (from the centre out) nucleus of maturing oocyte, oocyte cytoplasm, zona pellucida (pink ring), follicle cells, stromal cells.
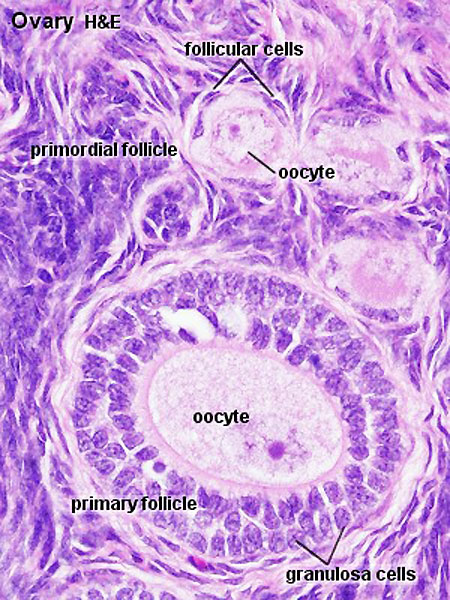
Ovary Cortex Primordial and Primary Follicles
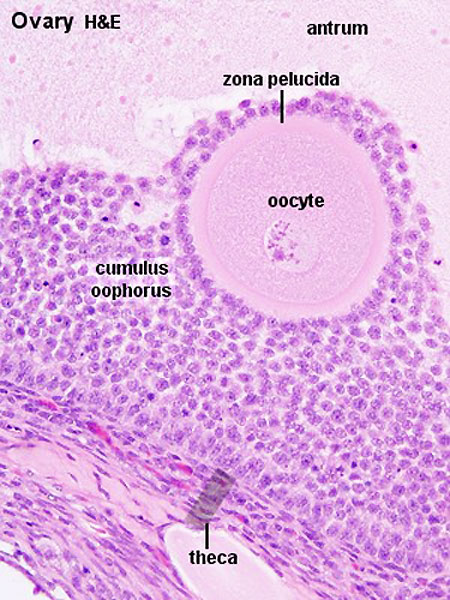
View of cortical ovary region showing primordial follicles and a single preantral follicle, with atretic follicle to its left. Bottom of picture shows outer cells of antral follicle.
High power view of ovary cortical region showing primordial follicles and a single preantral follicle.
Features: germinal epithelium, tunica albuginea, preantral follicle, nucleus of oocyte, oocyte cytoplasm, zona pellucida, Call-Exner body, stratum granulosa, basement membrane, theca, blood vessels surrounding follicle in theca layer.
Ovary Cortex and Medulla
Low power view of ovary cortex and medullary region. Note 3 stages of follocle development (primordial, preantral and antral).
Features:
- cortical primordial follicles
- oocyte
- follicular cells
- stromal cells
- preantral follicle- zona pellucida, stratum granulosa, theca
- early preovulatory follicle (Graafian) - oocyte, zona pellucida, corona radiata, cumulus oophorus, liquor folliculi, stratum granulosa, theca interna, theca externa, blood vessels surrounding follicle
Follicle Development
The development of a primordial follicle to a preovulatory follicle takes in excess of 120 days. After it has become a primary follicle of about 0.2 mm diameter it takes about 65 days to develop into a preovulatory follicle. Cohorts of follicles continually develop but only one is most sensitive to hormonal stimulation and is "selected", becoming the dominant follicle. All others in this cohort will undergo atresia.
Fertility Treatments
Superovulation therapy is a fertility drug treatement (oral clomiphene citrate and/or injectable FSH with or without LH) aimed at stimulating development/release of more than one follicle during a single menstrual cycle.
Follicle Classification
The above images show the histological changes that occur with follicle development (folliculogenesis). In humans, this entire process occurs over the timecourse of at least 3 menstrual cycles. This means that within the ovary during each cycle (at any point in time) many follicles can be either developing (folliculogenesis), regressing (atresis) and only a single follicle will be selected as ready for release. The selected follicle readied for release, generally one of the largest antral follicle, and can be classifed or described as: an antral preovulatory follicle or Graafian follicle or type 8 follicle (depending upon the classification used).
Classification systems - There are several different nomenclatures for the stages of follicle maturation (shown below) all of which makes the literature very confusing. The simplest is primordial, preantral, antral, Preovulatory (Graffian). You can also use the 5 step follicle classification: Primordial, Primary, Secondary, Tertiary, Preovulatory. Note that some classifications refer to the antral follicle as a secondary follicle and do not use the term tertiary follicle.
Primordial Follicle
Alternative nomenclature: small follicle or type 1, 2, 3 (25 cells) less than 50 micron diameter
Preantral Follicle
Alternative nomenclature: preantral follicle or type 4 (26-100 cells), type 5 (101-300 cells) up to 200 micron diameter
Antral Follicle
Alternative nomenclature: small antral type 6 (301-500 cells), large antral type 7 (501-1000 cells) small antral 500 micron diameter, large antral 1000-6000 micron diameter
Preovulatory Follicle
Alternative nomenclature: largest antral follicle or Graafian follicle or type 8 (>1000 cells) greater than 6000 micron diameter
Atresia
At any one time the majority of follicles are destined not to complete maturation and at any stage (from type 4-7) degeneration of the follicle can occur, this process is called atresia.
Ovulation
Movie (click image to play) showing process of ovulation (release of oocyte and follicular fluid). Click on movie to start.
Note that following ovulation the remnant of the follicle will degenerate if implantation does not occur (non-pregnant) forming a corpus albicans or following implantation (pregnancy) a corpus luteum which provides endocrine support to the uterus.
An endocrine signal (hCG human Chorionic Gonadotropin) from the implanting conceptus syncitiotrophoblasts maintains the corpus luteum, which in turn supports the uterine functional lining, preventing menstruation.
Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 | Quiz
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Additional Information
The information below is not part of today's Practical.
Links: Female Reproductive Tract Histology
Terms
- antral follicle - the stage following preantral in the decription of the sequence ovarian follicle development.
- antrum - (L. a cave), cavity; a nearly-closed cavity or bulge. In the ovary this refers to the follicular fluid-filled space within the follicle.
- atretic follicle - An ovarian follicle that fails to mature and degenerates. Also called "atresia" refering to the process of degeneration of the ovarian follicle. This process can occur at any stage of follicle development (folliculogenesis).
- clomiphene citrate - drug taken orally to promote the process of follicle/egg maturation.
- corona radiata - Layer of follicle cells of cumulus oophorus remaining attached to zona pellucida of oocyte after ovulation. Also called granulosa cells.
- corpus albicans - (L. corpus = body, L. albicans = whitish); a degenerating corpus luteum in ovary.
- corpus luteum - (L. corpus = body, L. luteum = yellow) The remains of ovarian follicle after ovulation that acts as an endocrine organ supporting pregnancy and preventing menstruation (loss of the endometrial lining). de Graaf first observed it in the ovary of a cow as a yellow structure.
- cortical - (L. corticalis) at the outside (like the bark of a tree), usually combined with medulla meaning the core.
- cumulus oophorus - (L. cumulus = a little mound G. oon = egg + phorus = bearing); part of the wall of an ovarian follicle surrounding and carrying the ovum (oocyte).
- follicle - (L. folliculus = little bag,dim. of L. follis). A structure which develops in the ovary and contains a developing egg (oocyte).
- follicular fluid - the fluid found in the antrum of a secondary follicle. Secreted by cells in the wall of the follicle. This fluid is released along with the oocyte at ovulation.
- germinal epithelium - cellular component covering surface of ovary, it is continuous with mesothelium covering mesovarium. Note that it is a historical misnomer, as it is not the actual site of germ cell formation.
- Graafian follicle - named after Regnier de Graaf (1641-1673), an historic Dutch physician embryologist who studied pregnancy using rabbits.
- granulosa cells - the supporting cells that surround the developing egg within the follicle thecal layers.
- mesovarium - mesentry of the ovary formed from a fold of the broad ligament that attaches the ovary
- medullary - (L. medius = in the middle) relating to the medulla; pith, marrow, inner portion of an organ. Usually combined with cortex (cortical) meaning the outer layer.
- oocyte - (Greek, oo = egg, ovum) The term used to describe the haploid egg or ovum formed within the ovary (female gonad) and released to enter the uterine tube and be transported to the uterus. The mature oocyte is the cell released from the ovary during ovulation.
- oocyte retrieval - (egg retrieval) A clinical in vitro fertilization (IVF) procedure to collect the eggs contained in the ovarian follicles.
- oogenesis - (Greek, oo = egg + genesis = origin, creation, generation) process of diploid oogonia division and differentiation into an haploid oocyte (egg) within the ovary (female gonad). Mammalian meiosis will only be completed within the oocyte if fertilization occurs.
- oogonia - (Greek, oo = egg) diploid germ cells within the ovary (female gonad) which provide the primary oocytes for oocyte (egg) formation. In humans, all oogonia form primary oocytes within the ovary before birth.
- oophorus - (Greek, oo = egg + phorus = carrying, egg-bearing) cumulus oophorus, used to describe the granulosa cells within the follicle that tether or link the oocyte to the wall of the follicle.
- ovulation - release of the oocyte from the mature follicle. In humans generally a single oocyte is released from a cohort of several maturing follicles.
- preantral follicle - the stage following primordial in the description of the sequence ovarian follicle development.
- primary follicle - the stage following primordial in the description of the sequence ovarian follicle development.
- primordial follicle - the first stage in the description of the sequence ovarian follicle development. Present in the ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. The primordial follicle is the oocyte and the surrounding follicular cells.
- primordial germ cell - oocyte present in the primordial follicle ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. The primordial follicle is the oocyte and the surrounding follicular cells.
- secondary follicles - the stage following primary in the description of the sequence ovarian follicle development.
- stromal cells - in the ovary, cells surrounding the developing follicle that form a connective tissue sheath (theca folliculi). This layer then differentiates into 2 layers (theca interna, theca externa). This region is richly vascularized and involved in hormone secretion.
- superovulation therapy - a fertility drug treatement (oral clomiphene citrate and/or injectable FSH with or without LH) aimed at stimulating development/release of more than one follicle during a single menstrual cycle.
- tertiary follicle - the stage following secondary in the description of the sequence ovarian follicle development.
- theca folliculi - stromal cells in the ovary, cells surrounding the developing follicle that form a connective tissue sheath. This layer then differentiates into 2 layers (theca interna, theca externa). This region is vascularized and involved in hormone secretion.
- theca externa - stromal cells forming the outer layer of the theca folliculi surrounding the developing follicle. Consisting of connective tissue cells, smooth muscle and collagen fibers.
- theca interna - stromal cells forming the inner layer of the theca folliculi surrounding the developing follicle. This vascularized layer of cells respond to LH (leutenizing hormone) synthesizing and secreting androgens which are processed into estrogen.
- tunica albuginea - dense connective tissue layer lying between germinal epithelium and cortical region of ovary.
- uterus - site of embryo implantation and development. Uterine wall has 3 major layers: endometrium, myometrium, and perimetrium. Endometrium can be further divided into the functional layer (shed/lost during menstruation) and basal layer (not lost during menstruation).
- zona pellucida - extracellular layer lying directly around the oocyte underneath follicular cells. Has an important role in egg development, fertilization and blastocyst development. This thick extracellular matrix consists of glcosaminoglycans and 3 glycoproteins (ZP1, ZP2, ZP3).
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
- 2010 BGD: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12
Cite this page: Hill, M.A. (2026, March 13) Embryology 2010 BGD Practical 3 - Oogenesis and Ovulation. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_BGD_Practical_3_-_Oogenesis_and_Ovulation
- © Dr Mark Hill 2026, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G