User:Z3418702: Difference between revisions
No edit summary |
No edit summary |
||
| Line 25: | Line 25: | ||
Lab 7 --[[User:Z3418702|Z3418702]] ([[User talk:Z3418702|talk]]) 11:16, 17 September 2014 (EST) | Lab 7 --[[User:Z3418702|Z3418702]] ([[User talk:Z3418702|talk]]) 11:16, 17 September 2014 (EST) | ||
Lab | Lab 9 --[[User:Z3418702|Z3418702]] ([[User talk:Z3418702|talk]]) 12:20, 8 October 2014 (EST) | ||
==Online Assessments== | ==Online Assessments== | ||
Revision as of 11:22, 8 October 2014
--Z3418702 (talk) 12:45, 6 August 2014 (EST)
Lab attendance
Lab 1----Z3418702 (talk) 12:57, 6 August 2014 (EST)
http://www.ncbi.nlm.nih.gov/pubmed
<pubmed>25084016</pubmed>
Lab 2 --Z3418702 (talk) 12:20, 13 August 2014 (EST)
Lab 3 ----Z3418702 (talk) 13:08, 20 August 2014 (EST)
Lab 4- --Z3418702 (talk) 12:34, 27 August 2014 (EST)
Lab 5 --Z3418702 (talk) 12:58, 3 September 2014 (EST)
Lab 6 --Z3418702 (talk) 12:45, 10 September 2014 (EST)
Lab 7 --Z3418702 (talk) 11:16, 17 September 2014 (EST)
Lab 9 --Z3418702 (talk) 12:20, 8 October 2014 (EST)
Online Assessments
Lab 1
Article 1: <pubmed>24592092</pubmed>
This study was conducted by the IVF Center at Kocaeli University, Turkey. It aimed to test the effect of biochemical markers in follicular fluid, such as nitrous oxide (NO), reduced glutathione (GSH) and malondialdehyde (MDA) on the outcome of in vitro fertilisation. The researchers selected 62 infertile women, all of whom were aged between 25 and 32, were non-smokers, had no systemic diseases, and were suffering from unexplained infertility with no signs of hormonal or ovulatory issues.
Ovulation was first induced in the women using long and short agonists along with a microdose flare-up, after which an oocyte was collected. This was followed by intracytoplasmic sperm injection (ICSI) as the preferred method of fertilisation, then the transfer of the embryo took place. To collect the FF samples, the dominant follicles were chosen and samples were centrifuged, supernatants were removed and stored.
To measure MDA levels, MDA was mixed with thiobarbaturic acid (TBA) which reacted to form a red compound. This mixture was incubated, cooled and assayed to read the absorbance of the butanol phase, and results were expressed in micromoles of MDA. Similarly, levels of GSH were measured in micromoles/L after being supplemented with metaphosphoric acid and assayed. However, NO levels were measured indirectly by measuring the nitrate and nitrite sample concentrations, deproteinising the sample, then measuring absorbance at 545nm using Griess reagent, expressing NO levels in nanomoles/L.
The embryos were then graded in terms of the size of the blastomere and degree of fragmentation, into Grades A-C, A being an even blastomere with <10% fragmentation. A single Grade A embryo was then transferred into each woman on Day 3 of the trial, after which they were categorised into 2 groups based on blood concentration of human chorionic gonadotropin; successful pregnancy (Group 1) and unsuccessful pregnancy (Group 2).
Finally, to analyse these results, the researchers used the women’s pregnancy status following IVF as the primary outcome measure. Statistic analysis was carried out according to non-parametric Mann-Whitney U test. The study found that the successful pregnancy group had significantly lower levels of fluid NO and significantly higher levels of fluid MDA than the unsuccessful pregnancy group. In analysing the correlation between IVF parameters and oxidative stress, the findings showed a positive weak correlation of MDA with fertilisation rate and the number of Grade A embryos. Also, ROC curve analysis implicated MDA as a highly sensitive predictor of pregnancy. Due to this significant difference in MDA levels between groups 1 and 2, the study concluded that MDA was the most suitable indicator of IVF success out of the 3 biochemical markers chosen for analysis.
Article 2: <pubmed>24914407</pubmed>
The objective of this study was to research the possible association between levels of plasma D-dimer, a haemostatic marker, and the success or failure of pregnancy in women undergoing IVF. The researchers selected 105 infertile women from the Ortona General Hospital’s Assisted Reproduction Unit who were undergoing IVF, indicated by factors such as tubal factor, endometriosis, male factor, anovulation and unexplained infertility.
The participants underwent ovarian stimulation by receiving daily subcutaneous injections of recombinant FSH (follicle stimulating hormone) with doses varying based on basal FSH level, the age of the woman and antral follicle count. This stimulation was begun upon complete pituitary suppression on the 3rd day of the menstrual cycle, and throughout the stimulation, hormonal fluctuations of luteinising hormone (LH) were controlled by injecting agonists and antagonists of GnRH.
Following the collection of oocytes, intracytoplasmic sperm injection (ICSI) was used to perform IVF and an embryo transfer was carried out, 14 days after which a pregnancy test was taken. The presence of a gestational sac with a fetal heartbeat after 7 weeks of gestation was the criterion for a clinical pregnancy.This ovarian stimulation protocol was followed by a venous blood sample to test D-dimer concentrations, where a latex quantitative assay was used with 200ng/mL being the threshold level for an abnormal D-dimer level. These assay levels were statistically analysed using a Mann-Whitney U-test and T-test.
The results of the study indicated significantly higher levels of circulating D-dimer in women with a failed pregnancy following IVF in comparison to those with a clinical or successful pregnancy. This difference was statistically valid even when taking age and vascular risk factors into account. It was found that women with concentrations of D-dimer above the threshold had a more dismal pregnancy outcome, and that D-dimer levels increased after the one-week administration of GnRH. Overall, only 38% of the participants had achieved a clinical pregnancy and the study concluded that high D-dimer concentrations are implicated in a higher risk of a failed pregnancy following IVF. This was consistent with previous postulations that a possible mechanism for failure is unsuccessful implantation and placentation, owing to a hypercoagulable vascular state, leading to increased risk of thrombolic events in maternal vessels to the placenta.
--Mark Hill - Both these papers are recent and present interesting findings. It would have helped you summary in the second paper if you had described what plasma D-dimer was. Your summaries are both correct and concise (5/5).
Lab 2
Fertilisation of medusa eggs by spermatozoids in vitro in sea water[1]
--Mark Hill (talk) 16:28, 21 August 2014 (EST) This is all correct, I have fixed the reference link below. Please in future use a shorter image title and do not use .jpg in the image description above (I have removed for you). (4/5)
Lab 3
Adrenal gland
<pubmed>7011178</pubmed> <pubmed>24116052</pubmed>
Gonad development
<pubmed>17237341</pubmed> <pubmed>7623307</pubmed>
Placenta
<pubmed>10419690</pubmed> <pubmed>7673080</pubmed>
--[[User:Z8600021|Mark Hill] These references are appropriate, you should have included some descriptions, even a single line, with the reference (4/5).
Lab 4
Summary of research article
This study by Chang et al. observed the effect of varying the intratracheal transplantation time of umbilical cord blood (UCB)-derived mesenchymal stem cells (MSCs) on the attenuation of hyperoxic lung injury in neonatal rats. It was concluded that the optimal time window for stem cell transplantation was narrow; efficient only during the early but not late phases of inflammation. The findings were in line with previous research that the anti-inflammatory properties of UCB-derived MSCs play a crucial therapeutic role in the alleviation of bronchopulmonary dysplasia (BPD), through reducing hypoxia-induced injuries including increased apoptosis and impaired alveolarisation.
Tissue sampling and analysis of lung histopathology found that the Hypoxia Control (HC) group showed fewer, larger and more abnormally-sized alveoli compared to the Normoxia Control (NC) group. However, upon transplantation of UCB-derived MSCs, these alveolar impairments and changes in morphology were attenuated, especially when added on post-natal day 3 (HT3) than on post-natal day 10 (HT10).
The study’s comparison of the levels of pro-inflammatory cytokines such as IL-6α, IL-6β and TNF-α before and after the addition of the UCB-derived MSCs found that such molecular markers were significantly lower after HT3 transplantation than HT10 transplantation. These levels were much lower than the initial starting levels exhibited by the NC group, indicating the therapeutic effect of the cord cells. Furthermore, the hypoxia-induced reduction in VEGF and HGF levels and increase in lung collagen levels were both attenuated by the addition of the MSCs.
These findings led to the conclusion that the therapeutic efficacy of UCB-derived MSCs on treating BPD is indeed time-dependent; having potent effects in the early inflammatory process, which is then reduced in later stages. The study also tested any potential synergistic effects of combined early and late MSCs intratracheal transplantation, but none were found.
<pubmed>23349686</pubmed>
Vascular shunts
The 3 developmental vascular shunts in the fetal circulation that close postnatally are:
a) Ductus arteriosus (Ductus Botalli): Connects the pulmonary artery to the proximal descending part of the aortic arch and prevents the output of the right ventricle from entering the unexpanded fetal lung, which is fluid-filled and non-functioning. This shunt transfers medium oxygen saturated blood and becomes the ligamentum arteriosum after closing at birth.
b) Ductus venosus: Shunts blood from the left umbilical vein to the inferior vena cava. This carries well-oxygenated blood and allows placental blood to bypass the liver ultimately to the fetal brain.
c) Foramen ovale (Foramen Botalli): Shunts blood that is highly saturated with oxygen from the right atrium to the left atrium and becomes the fossa ovalis after closing at birth.
Lab 5
Bronchogenic Cysts
Bronchogenic cysts (BCs) are an unusual and rare congenital abnormality of the bronchial tree; a generally benign type of malformation of the bronchopulmonary foregut. The classification of these cysts is into; those occurring in the mediastinum (65-90%), which have equal prevalence between the sexes, or those of intrapulmonary origin (lung or pleura) which display a slight male predominance [1] Other sites such as intradiaphragmatic and retroperitoneal are rare, and consequently require close attention.
These lesions are characteristically unilocular, mucus field cysts which arise from the posterior walls of airway membranes during embryonic development. They currently account for 20-30% of congenital cystic bronchopulmonary foregut abnormalities and for only 5-10% of paediatric mediastinal masses. [1] Although the exact cause of bronchogenic cysts is yet to be established, current research postulates that that their developmental cause is the abnormal budding of the tracheal diverticulum and proximal bronchial structures during embryogenesis in weeks 4-6. Bronchogenic cysts stem from abnormal buds from the tracheobronchial tree or primitive esophagus which fail to extend to the site of alveolar differentiation. Generally, early separation causes the system to move into the mediastinum, however it is when this separation occurs late that a BC forms [1]. Histologically, these abnormal bronchogenic cysts are lined by pseudostratified, ciliated, columnar or cuboidal secretory respiratory epithelium and their walls comprise typical structural components of the airways such as smooth muscle, cartilage and mucinous glands. Cysts are typically not filled with air as they lack communication with the bronchial tree, but contain fluid comprising blood, proteinaceous fluid and calcium oxalate, resulting in a solid lesion manifesting on radiographic imaging such as MRI and CT scans [2]
BCs are considered to be the most common form of foregut duplication cysts and are a congenital anomaly as they are asymptomatic and rarely arise in infants with diagnosis usually occurring post-natally. The clinical presentation of cysts is usually either asymptomatic or through airway obstruction causing respiratory distress or cystic infection causing compression of central lung parenchyma [3]
Lab 7
Research article- Pax6 is essential for establishing ventral-dorsal cell boundaries in pituitary gland development
This study by Kioussi et al. investigated the role of the transcription factor Pax6 in creating a dorsal-ventral boundary between cell types of the developing pituitary gland. The researchers considered the physical location of the six cell types in the pituitary that originate from a common primordium- corticotropes, thyrotropes, menalotropes, gonadotropes, somatotropes and lactotropes. They specifically focused on the regulation of cell differentiation by Pax6 and the effects of its absence.
Following analysis of mutant mice embryos with a Small eye (Sey) mutation and Pax6 gene deletion, the study found that Pax6 plays a significant role as an early dorsal marker of the pituitary gland’s development. They found that Pax6 transcripts were expressed and present in the nascent Rathke’s pouch, however excluded from the ventral section of the Sonic hedgehog (Shh) pouch, leading to the formation of a ventral zone between cells expressing Pax6 and those expressing Shh. A dorsal-ventral gradient for cell differentiation was evident and Pax6 was seen to be excluded from the rostral zone of the pituitary. These two particular findings suggested that Pax6 may be an essential element of the ‘transcriptional apparatus’ responsible for determining the position of the six pituitary cell lineages.
Furthermore, the research concluded that the absence of Pax6 leads to a decrease in dorsal cell types from the Pit-1 lineage (somatotropes and lactotropes) and an increase in cell types with ventral phenotypes such as thyrotropes. This was confirmed by discovering that the expression patterns of four molecular ventral markers such as GATA2 were uniformly dorsalised, leading to further increase in the population of thyrotropes.
Hence, these results implicated that Pax6 functions as a transcriptional regulator in opposition to ventral signalling molecules, thus clearly delineating the developing dorsal cells from ventral cells in the differentiation stage of pituitary gland development. It has a key regulatory role in the formation of a sharp dorsal-ventral cell type margin through the inhibition of Shh ventral signals.
<pubmed>10588713</pubmed>
Tooth development
The cells and their layers that contribute to tooth development through odontogenesis (from week 6 of development) include:
- Odontoblasts: Mesenchymal cells of neural crest origin that produce predentin, which calcifies forming dentin in the process of dentinogenesis. Enamel epithelium causes odontoblast differentiation and these cells contribute to the outer dental pulp
- Ameloblasts: Derived from ectodermal cells of oral epithelium tissue. They differentiate from preameloblasts, activated by ectomesenchymal cells and produce enamel proteins such as amelogenin and enamelin to form enamel, the outer covering of the tooth’s crown.
- Peridontal ligament: Composed of connective tissue (bundles of collagen fibres), which secures the root of the tooth in the alveolar socket so it is not displaced. It surrounds the cementum of the tooth root.
Lab 8
Ovary development
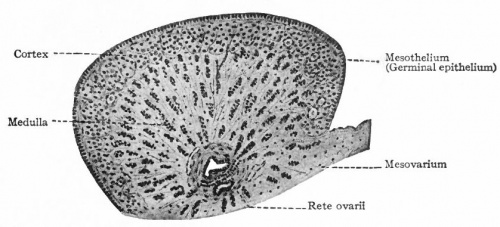
Initially, the genital systems of both sexes are morphologically similar and sexual development hence begins as an indifferent stage with an indifferent (‘bipotential’) gonad later forming either the testis or ovary. Both gonads have contributions from; mesothelium of the posterior abdominal wall cavity, mesenchyme beneath this and primordial germ cells (PGCs) that later differentiate to form sex cells.
In Week 5 of development, a thickening of mesothelium forms on the medial portion of the primitive kidney (the mesonephros). The formation of the gonadal ridge results from the proliferation of the mesothelium and mesenchymal tissue beneath it, as a bulge on the medial mesonephros. Projection of finger-like gonadal (epithelial) cords into the mesenchyme follows, segmenting the indifferent gonad into an internal medulla (covered by germinal epithelium) and external cortex. For embryos with a sex chromosome complex of XX, the medulla regresses while the cortex of the indifferent gonad differentiates to form the ovary.
PGCs reside among dorsal endodermal cells of the umbilical vesicle whose dorsal part is incorporated into the embryo during folding. They are the first cell type migrating through the primitive streak in gastrulation (3rd week) and then reside at the junctional region of the hindgut yolk sac. Following this, there is migration of the PGCs to the gonadal ridge along the hindgut’s dorsal mesentery, regulated by BMP-4, fragilis and stella genes. In week 6, these germ cells are incorporated into the gonadal cords and are called oogonia, having entered underlying mesenchyme.
In female embryos, ovary development is a slow process, with the ovary not histologically identifiable until week 10. Ovary development relies on the genes of the XX chromosome along with an autosomal gene. Gonadal cords form a basic rete ovarii (network of canals) by extension into the internal medulla, although the cords are not notable in the embryonic ovary. The rete ovarii and gonadal cords usually degrade and cease to exist.
Transverse section of the ovary of a fox embryo