Talk:2010 BGD Practical - Fetal Development: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
[[2010 BGD Practical - Fetal Development|Practical 12]]: [[2010 BGD Practical 12 - Embryo to Fetus]] | [[2010 BGD Practical 12 - Second Trimester]] | [[2010 BGD Practical 12 - Third Trimester]] | [[2010 BGD Practical 12 - | [[2010 BGD Practical - Fetal Development|Practical 12]]: [[2010 BGD Practical 12 - Embryo to Fetus|Embryo to Fetus]] | [[2010 BGD Practical 12 - Second Trimester|Second Trimester]] | [[2010 BGD Practical 12 - Third Trimester|Third Trimester]] | [[2010 BGD Practical 12 - Birth]] | [[2010 BGD Practical 12 - Abnormalities|Abnormalities]] | | ||
[[2010 BGD Practical 12 - Embryo to Fetus]] | [[2010 BGD Practical 12 - Embryo to Fetus]] | ||
Revision as of 11:23, 22 May 2010
The fetal period (9-36 weeks) is about continued differentiation of organs and tissues, most importantly this period is about growth both in size and weight. The tables showing second and third trimester on this page are to indicate some selected systems developmental changes, you are not required to know detailed timings or events.
Practical 12: Embryo to Fetus | Second Trimester | Third Trimester | 2010 BGD Practical 12 - Birth | Abnormalities |
2010 BGD Practical 12 - Embryo to Fetus
- Week 8 Stage 23
- Week 10 Fetus
2010 BGD Practical 12 - Second Trimester
- Early fetal - week 10, week 12
- placental changes and fetal membrane changes
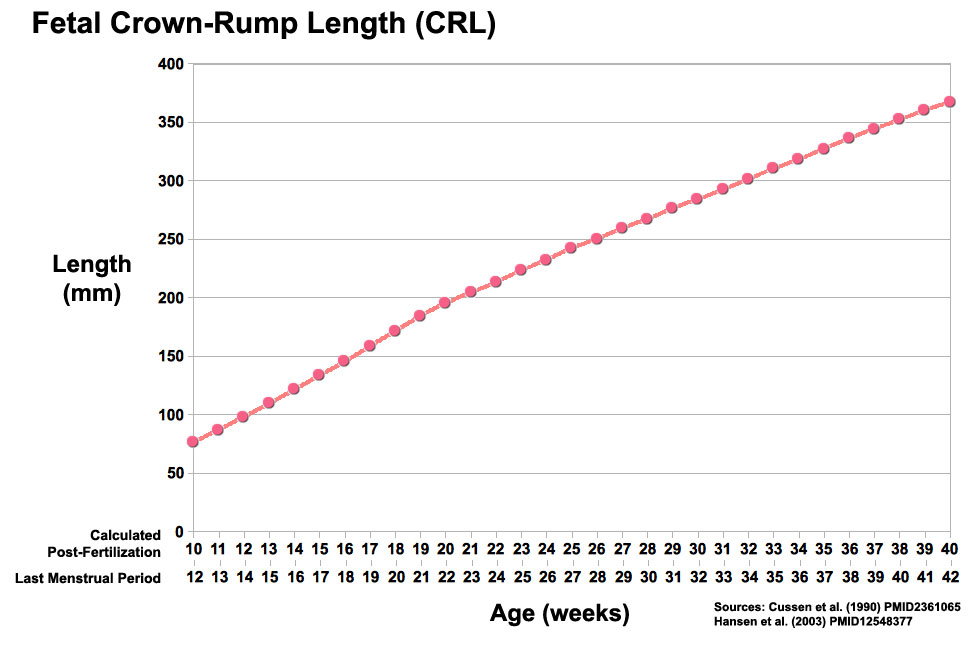
- length changes
- clinical diagnosis (ultrasound), genetic
- survival issues for early delivery
- Fetal Endocrine
2010 BGD Practical 12 - Third Trimester
- Fetal Neural
- Fetal Respiratory
- Fetal Cardiovascular
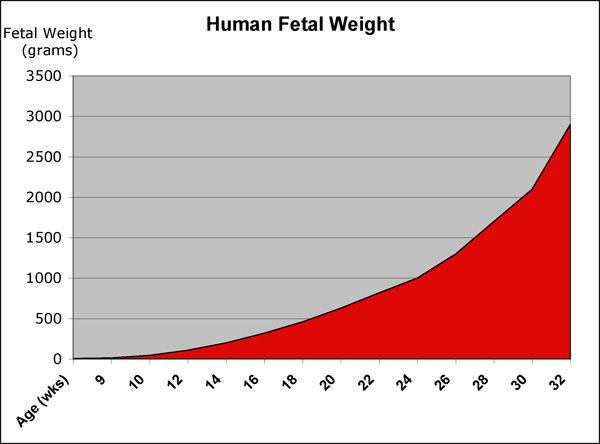
- fetal weight
- fetal origins hypothesis
- parturition
- neonatal issues
2010 BGD Practical 12 - Abnormalities
UNSW Embryology - Abnormal Development Tutorial - Applied Embryology and Teratology
- Teratology
Embryonic Week 8
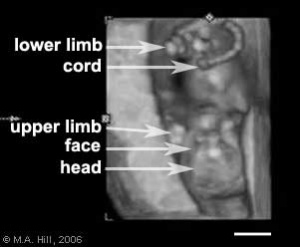
Fetal Week 10
Week 10, 40 mm, female fetus, early fetal stage of development
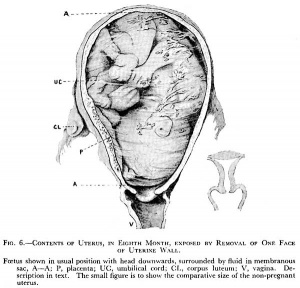
Fetal Week 12
Second Trimester
Third Trimester
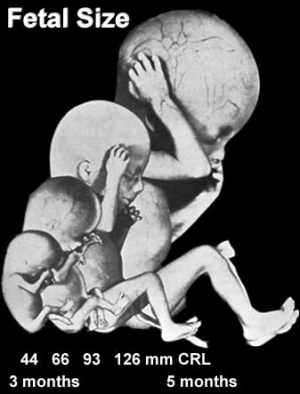
Fetal Size
Fetal length change is greatest in the middle period (second trimester).
Fetal Weight
See also Fetal origins hypothesis and Normal Development - Birth - Low Birth Weight
Fetal Neural
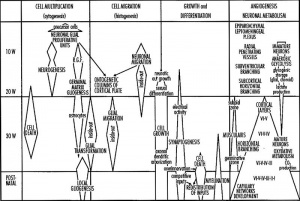
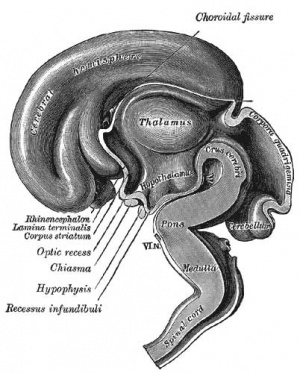
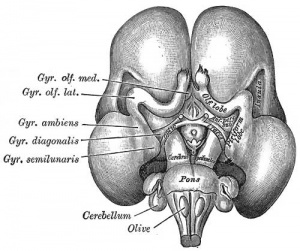
During the fetal period there is ongoing growth in size, weight and surface area of the brain and spinal cord. Microscopically there is ongoing: cell migration, extension of processes, cell death and glial cell development.
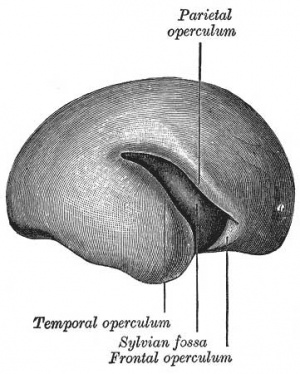
Cortical maturation (sulcation and gyration) and vascularization of the lateral surface of the brain starts with the insular cortex (insula, insulary cortex or insular lobe) region during the fetal period. This cerebral cortex region in the adult brain lies deep within the lateral sulcus between the temporal lobe and the parietal lobe.
- sulcation - The process of brain growth in the second to third trimester which forms sulci, grooves or folds visible on fetal brain surface as gyri grow (gyration). Abnormalities of these processes can lead to a smooth brain (lissencephaly).
- gyration - The development of surface folds on the brain (singular, gyrus)
Insular Gyral and Sulcal Development
- 13-17 gestational weeks - appearance of the first sulcus
- 18-19 gestational weeks - development of the periinsular sulci
- 20-22 gestational weeks - central sulci and opercularization of the insula
- 24-26 gestational weeks - covering of the posterior insula
- 27-28 gestational weeks - closure of the laeteral sulcus (Sylvian fissure or lateral fissure)
(Data from: Afif A, etal., 2007)
Three-dimensional magnetic resonance imaging and image-processing algorithms have been used to quantitate between 29-41 weeks volumes of: total brain, cerebral gray matter, unmyelinated white matter, myelinated, and cerebrospinal fluid (grey matter- mainly neuronal cell bodies; white matter- mainly neural processes and glia). A study of 78 premature and mature newborns showed that total brain tissue volume increased linearly over this period at a rate of 22 ml/week. Total grey matter also showed a linear increase in relative intracranial volume of approximately 1.4% or 15 ml/week. The rapid increase in total grey matter is mainly due to a fourfold increase in cortical grey matter. Quantification of extracerebral and intraventricular CSF was found to change only minimally.
(Text - modified from Huppi etal., (1998) Quantitative magnetic resonance imaging of brain development in premature and mature newborns. Ann Neurol 43(2):224-235.)
Neural development will continue after birth with substantial growth, death and reorganization occuring during the postnatally (MH - postnatal not described in this current lecture)
Neural Development - Fetal | Neuroscience - Regional specification of the developing brain
Fetal Cardiovascular
MH - covered in yesterday's lecture Late Vascular Development.
- fetal neutrophils, monocytes, and macrophages are produced
- mononuclear phagocytes do not mature until after birth
Immune System
- maternal placenta transfer of IgG not other immunoglobulin isotypes.
- fetal lymphocytes (mature T and B cells) produced not activated
MH - see Postnatal lecture - maternal milk IgG and IgA antibodies, leukocytes, secretory IgA, lactoferrin, lysozyme, and oligosaccharides and glycoconjugates that are receptor analogs for microbial adhesins and toxins.
Fetal Respiratory
MH - covered in lecture Respiratory Development.
Month 3-6 - lungs appear glandular, end month 6 alveolar cells type 2 appear and begin to secrete surfactant.
Month 7 - respiratory bronchioles proliferate and end in alveolar ducts and sacs.
Lung Stages
- week 4 - 5 embryonic
- week 5 - 17 pseudoglandular
- week 16 - 25 canalicular
- week 24 - 40 terminal sac
- late fetal - 8 years alveolar
Fetal Genital
MH - introduced in the Genital Development lecture.
- ovary and testis development
- external genital development
- testis descent
Fetal Endocrine
Pituitary Hormones
- HPA axis established by week 20
- Pituitary functional throughout fetal development
Thyroid Hormone
- required for metabolic activity, also in the newborn
- important for neural development
Parathyroid Hormone
- newborn has total calcium levels (approx 20 grams) accumulated mainly in the 3rd trimester (weeks 28–40)
- fetal parathyroid hormone (PTH) potentially available from 10–12 weeks and PTH does not cross the placenta
- fetus relatively hypercalcemic, active transplacental transport of Ca2+ to fetus
- maternal serum - calcium ions (Ca2+), inorganic phosphate (Pi) and PTH concentrations are within the non-pregnant normal range throughout pregnancy.
- maternal bone turnover increases in the 3rd trimester.
(Based on Endocrinology - Materno—fetal calcium balance)
Pancreatic Hormones
- maternal diabetes can affect fetal pancreas development (increase in fetal islet beta cells).
Gonadal Hormones
- testosterone - required during fetal development for external genital development and internal genital tract in male.
- estrogens - secreted inactive precursor converted to active form by placenta.
Endocrinology - Control of steroid production in the fetal gonads | Neuroscience - The Effect of Sex Hormones on Neural Circuitry
Abnormalities
UNSW Embryology - Abnormal Development Tutorial - Applied Embryology and Teratology
Teratology
How different environmental effects during the pregnancy may influence outcomes. A teratogen (Greek, teraton = monster) is defined as any agent that causes a structural abnormality (congenital abnormalities) following fetal exposure during pregnancy. The overall effect depends on dosage and time of exposure (see critical periods below).
Absolute risk - the rate of occurrence of an abnormal phenotype among individuals exposed to the agent. (e.g. fetal alcohol syndrome)
Relative risk - the ratio of the rate of the condition among the exposed and the nonexposed. (e.g. smokers risk of having a low birth weight baby compared to non-smokers) A high relative risk may indicate a low absolute risk if the condition is rare.
Mutagen - a chemical or agent that can cause permanent damage to the deoxyribonucleic acid (DNA) in a cell. DNA damage in the human egg or sperm may lead to reduced fertility, spontaneous abortion (miscarriage), birth defects and heritable diseases.
Fetotoxicant - is a chemical that adversely affects the developing fetus, resulting in low birth weight, symptoms of poisoning at birth or stillbirth (fetus dies before it is born).
Synergism - when the combined effect of exposure to more than one chemical at one time, or to a chemical in combination with other hazards (heat, radiation, infection) results in effects of such exposure to be greater than the sum of the individual effects of each hazard by itself.
Toxicogenomics - the interaction between the genome, chemicals in the environment, and disease. Cells exposed to a stress, drug or toxicant respond by altering the pattern of expression of genes within their chromosomes. Based on new genetic and microarray technologies.
Critical Periods
Human Critical Periods of development
Fetal Origins Hypothesis
Maternal derived abnormalities relate to lifestyle, environment and nutrition and while some of these directly effect embryonic development. There is also growing evidence that some effects are more subtle and relate to later life health events. This theory is based on the early statistical analysis carried out by Barker of low birth weight data collected in the early 1900's in the south east of England which he then compared with these same babies later health outcomes. The theory was therefore originally called the "Barker Hypothesis" and has recently been renamed as "fetal origins" or "programming".
Reading
- Human Embryology (3rd ed.) Larson Ch15: Fetal development and the Fetus as Patient p481-499
- Color Atlas of Clinical Embryology (2nd ed.) Moore, Persaud and Shiota Ch3: 9th to 38th weeks of human development p50-68
Second Trimester
- Second Trimester
- Week 12 - CRL 85 mm, femur length 15 mm, biparietal diameter 25 mm.
Third Trimester
- Third Trimester
- Vibration acoustically of maternal abdominal wall induces startle respone in fetus.
- Month 7 - respiratory bronchioles proliferate and end in alveolar ducts and sacs.
- Week 37 to 38 Birth.
References
Reviews
- Fetal assessment during pregnancy. Farley D, Dudley DJ. Pediatr Clin North Am. 2009 Jun;56(3):489-504, Table of Contents. Review. PMID: 19501688
- Regimens of fetal surveillance for impaired fetal growth. Grivell RM, Wong L, Bhatia V. Cochrane Database Syst Rev. 2009 Jan 21;(1):CD007113. Review. PMID: 19160321
Articles
Search PubMed
Search Pubmed: fetal+development | Second Trimester | Third Trimester