RG Test01
| 2014 Student Projects | ||||
|---|---|---|---|---|
| 2014 Student Projects: Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | Group 6 | Group 7 | Group 8 | ||||
| The Group assessment for 2014 will be an online project on Fetal Development of a specific System.
This page is an undergraduate science embryology student and may contain inaccuracies in either description or acknowledgements. | ||||
Integumentary
Introduction
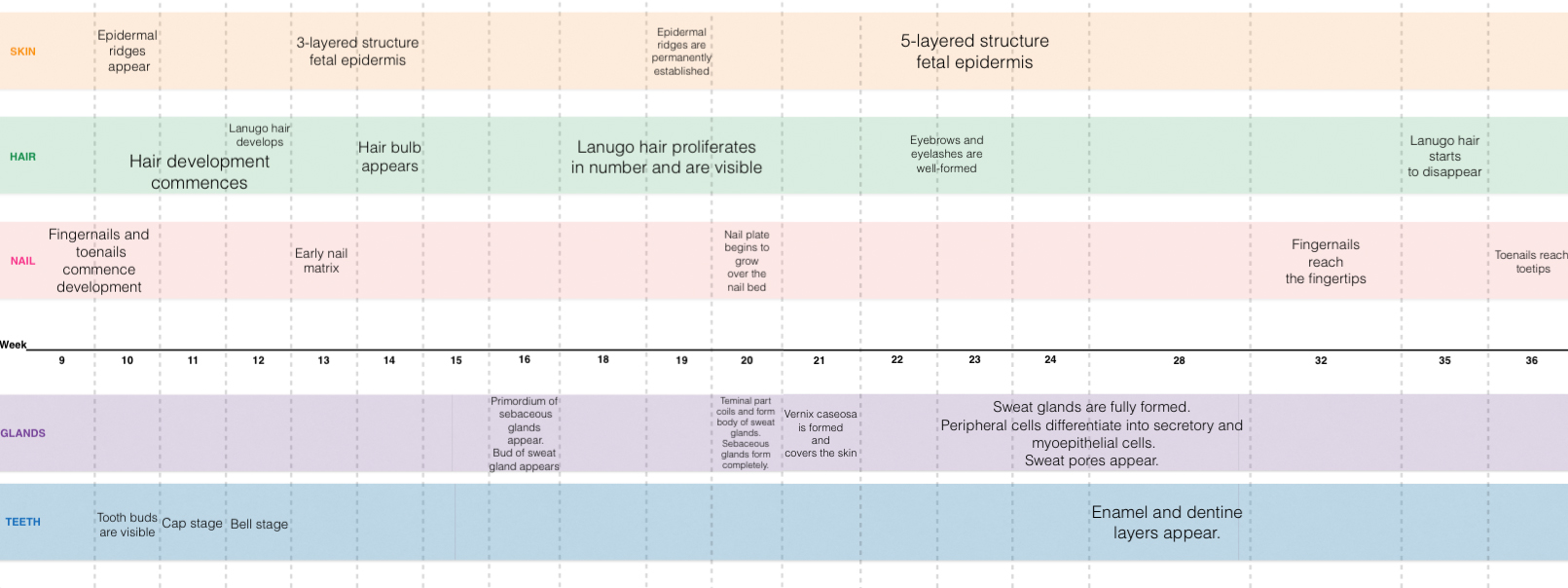
This page concerns the development of the integumentary system in the fetal stage of development, particularly its organs i.e. the skin, glands, hair, teeth, and nails. It explores the mechanism of development as well as the timeline of development. This page also outlines some recent findings on the development of the integumentary system, as well as historic findings. Finally, this page also explores some of the congenital abnormalities of the integumentary system, its mechanism or pathogenesis, clinical manifestations, and how they are treated or managed.
| Objectives |
|---|
|
Development Overview
Skin
The skin consists of 2 layers: the outer layer (epidermis) and a deeper connective tissue layer (dermis)[1].
- The epidermis is derived from the ectoderm. Initially it exists as only a single layer of ectodermal cells at 7-8 days of gestation[2]. However, by about 13-14 weeks after gestation, a 3- layered structure of fetal epidermis exists[3]- consisting of the stratum basale, 1 or 2 intermediate layers and the periderm[4]. The peridermal cells eventually become desquamated and form part of the vernix cervix.
- The somatic mesoderm is the embryonic origin of the dermis. The mesoderm of the dermatones of the body, also contribute to the development of the dermis. Specifically though, in the head and neck region of the body, the dermis is derived from neural crest cells[7].
- The dermis is initially composed of just mesenchymal cells- loosely aggregated mesodermal cells. These mesenchymal cells later develop into fibroblasts- which function to secrete collagen and lay-down elastic fibers into the extracellular matrix[7].
3 other specialised cells of the epidermis also exists[7] - these include melanoblasts, Langherhan cells and Merkel cells.
- Melanoblasts- are derived from neural crest cells that have migrated into the stratum basale. Mid-pregnancy, melanosomes are observed, differentiating the melanoblasts into melanocytes[7].
- Langheran cells- are derived from bone marrow (originally form mesoderm) and migrate into the epidermis[7]. They have the function of antigen presentation.
- Merkel cells- still have an uncertain origin. They have a function related to mechanoreception.
-snip-
Hypohidrotic Ectodermal Dysplasia

Hypohidrotic ectodermal dysplasia (HED) is the most of all ectodermal dysplasias, caused by an abnormality in the development of ectodermal tissues, which inlude skin, hair, teeth, sweat glands, and nails.[9][10] Patients with ectodermal dysplasia often have sparse hair and oligodontia, which is a condition where teeth are missing and are poorly developed.[9][10] Sweating is a very important function in the body in terms of thermoregulation. HED is mainly characterised by hypohidrosis due to the lack of sweat glands in the skin, which could lead to hyperpyrexia and sometimes death. In neonates, the mortality rate of HED reaches up to 30%, with the first year of life having the highest risk. [9] HED is caused by a genetic abnormality of the ectodysplasin A gene (EDA) and passed on by X-linked inheritance. The mutations of this gene results in the poor sweating ability or none at all in a person. The effects of this abnormality is usually more severe in males than in females. [11][10]
There is currently no pharmacological therapies for HED but there are methods applied to prevent the disease from aggravating. Neonates with HED are placed in incubators and monitored to prevent them from overheating. Management of this disease gets easier as the patient ages. Adults with HED can control their thermoregulation by staying in cool environments or drinking cold drinks to lower the body temperature. Currently, there are studies that aim to find a cure for this abnormality, e.g. gene replacement therapy in animal models.[10]
| More Abnormalities |
|---|
References
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedMoore & Persaud - ↑ <pubmed>19701759</pubmed>
- ↑ <pubmed>2413039</pubmed>
- ↑ 4.0 4.1 <pubmed>168272</pubmed>
- ↑ <pubmed>11841536</pubmed>
- ↑ <pubmed>17039717</pubmed>
- ↑ 7.0 7.1 7.2 7.3 7.4 Dudek, R.W. (2011). BRS Embryology (5th ed.). Lippincott Williams & Wilkins
- ↑ <pubmed>21165248 </pubmed>
- ↑ 9.0 9.1 9.2 <pubmed>20682465</pubmed>
- ↑ 10.0 10.1 10.2 10.3 <pubmed>24678015</pubmed>
- ↑ <pubmed>21357618</pubmed>