BGDA Practical - Female Reproductive Tract Histology
From Embryology
Introduction
This current page provides background support information for Medicine phase 1 BGD Histology Practical Virtual Slides. Page does not form part of the BGDA practical class virtual slides.
- Virtual Slides: Female Histology
- Draft page (notice removed when completed).
Objectives
- Gain an overview of the microanatomy of the female reproductive system.
- Undertake a microscopical examination of the ovary, oviduct, uterus, cervix, vagina and mammary glands. The functional significance of the various histological structures identified will be discussed.
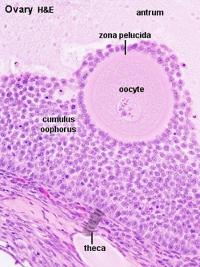
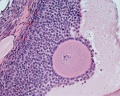
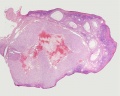
Ovary
Corpus Luteum
Cells work together in the production of ovarian hormones that support the initial pregnancy. Progesterone is synthesized from cholesterol by both the large and small luteal cells upon luteal maturation.
Theca Lutein Cells
Granulosa Lutein Cells
|
|
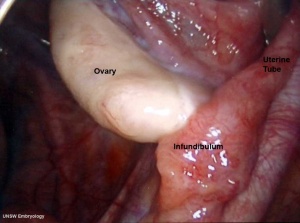
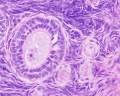
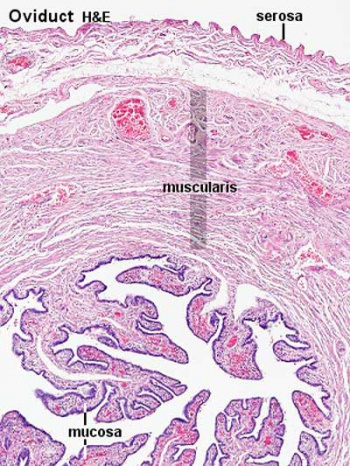
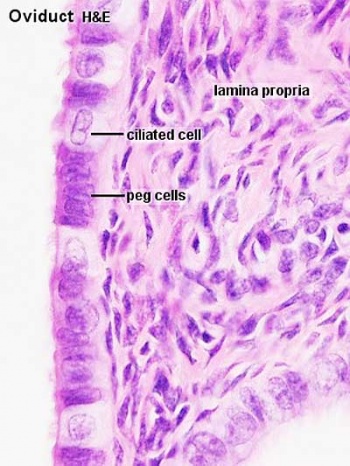
Uterine Tube
(oviduct, Fallopian tube)
- uterine tube acts as a conduit for the oocyte, from the ovaries to the uterus.
- consists of a mucosa and a muscularis.
- peritoneal surface of the oviduct is lined by a serosa and subjacent connective tissue.
Tube Regions
| infundibulum | ampulla | isthmus | intramural |
|---|---|---|---|
| funnel-shaped (up to 10 mm in diameter) end of the oviduct. Finger-like extensions of its margins, the fimbriae, are closely applied to the ovary. Ciliated cells are frequent. | mucosal folds, or plicae, and secondary folds which arise from the plicae divide the lumen of the ampulla into a very complex shape. Fertilization usually takes place in the ampulla. | narrowest portion (2-3 mm in diameter) of the tube located in the peritoneal cavity. Mucosal folds are less complex and the muscularis is thick. An inner, longitudinal layer of muscle is present in the isthmus. | penetrates the wall of the uterus. The mucosa is smooth, and the inner diameter of the duct is very small. |
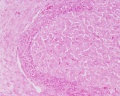
Uterus
- parts - body (upper two-thirds) and cervix.
- walls - mucosal layer, the endometrium, and a fibromuscular layer, the myometrium.
- peritoneal surface of the uterus is covered by a serosa.
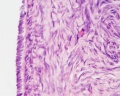
Myometrium
- smooth muscle fibres form several layers with preferred orientations.
- muscular tissue hypertrophies during pregnancy.
- GAP-junctions between cells become more frequent.
Endometrium
- simple columnar epithelium (ciliated cells and secretory cells) and an underlying thick connective tissue stroma.
- mucosa is invaginated to form many simple tubular uterine glands.
- glands extend through the entire thickness of the stroma.
- stromal cells of the endometrium are embedded in a network of reticular fibres.
Menstrual cycle
- hormones alter the endometrium.
- only the uterus body mucosa takes part in the menstrual cycle.
- endometrial layers (based on changes)
- basalis - remains during menstruation, functions as a regenerative zone for the functionalis.
- functionalis - lost during menstruation, functions as the site of cyclic changes in the endometrium.
- Uterus Histology Links: Labeled - proliferative phase | Labeled - gland proliferative phase | Labeled - secretory phase | Unlabeled - secretory phase | Unlabeled - late secretory phase | Labeled - gland secretory phase | Menstrual Cycle | Uterine Gland | Uterus Development
- Links: Menstrual Cycle - Histology