2010 Group Project 2
Chorionic Villus Sampling (CVS)
Introduction
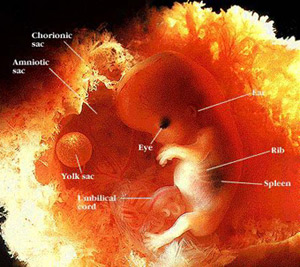
Chorionic villus sampling or CVS is a type of prenatal diagnosis test performed in the first trimester to detect major fetal abnormalities. In the procedure, tissue is withdrawn from the villi of the chorion and tested for chromosomal defects. It is usually done in women over the age of 37 as the chance of chromosomal defects increase with the mothers age. CVS is a specific test for particular abnormalities, such as Down Syndrome or Cystic Fibrosis. It is commonly performed between 10 and 12 weeks of pregnancy.
The advantage of CVS over other procedures is that the result is available approx 6 weeks earlier in the pregnancy, so if a termination is needed, it can be done earlier which is much safer, rather than later in the pregnancy.
Why would you use CVS over other techniques?
ADVANTAGES
- Can be performed earlier in pregnancy than amniocentesis (at around ten weeks).
- Results are available faster
- Cells obtained are mitotically active
- Amount of tissue obtained is preferable for DNA analysis.
- It is almost 100% reliable in detecting chromosomal and genetic defects.
DISADVANTAGES
- It carries a slightly higher risk of miscarriage (1%-2%) than does amniocentesis
- It's less commonly available than amniocentesis, and fewer doctors are experienced in the procedure.
- It entails a greater risk of distorted results than does amniocentesis due to presence of mother's cells in the sample and discrepancies between chorionic villi and fetal genes.
- Metabolic disorders are difficult to diagnose and must be confirmed with amniocentesis.
- Because of the early gestational age at which the test is performed, fetal anatomy cannot be seen as well as it can at the time amniocentesis is performed.
Historic background
Brief timeline of CVS use
- 1968 - Mohr in Scandinavia introduced the concept of prenatal diagnosis using chorionic villi sampling
- 1973 - Kullander and Sandahl and Hahnemann in 1974 showed further study into chromosomal analysis from CVS
- 1975 - from the Department of Obstetrics and Gynaecology at the Tietung Hospital in Anshan, China was successful in using CVS to determine sex of fetuses for sex pre selection.
- 1980 - Kazy et al. were the first to use ultrasound guidance during chorionic villi sampling.
- 1981 - Niazi et al. improved methods for culturing of fibroblasts from trophoblast villi.
- 1983 - Ward performed transcervical CVS with 67% success rate. In the same year, the Brombati group demonstrated and 96% success rate with obtaining villi with the aid of ultrasound guidance
- 1984 - Smidt-Jensen and Hahnemann introduced transabdominal CVS under ultrasound guidance
- 1986 - The Golbus group had a 3.8% miscarriage rate, and subsequently many other clinics started reporting a much lower rate of miscarriage at 1.7% making the procedure safe for routine use
Jan Mohr (1921-2009)
1968 -- Concept of CVS introduced
In 1968 Jan Mohr introduced the concept of prenatal diagnosis using the CVS technique.[1] He used the transcervical method to get a biopsy of the chorion using an endoscope as the source of vision. The current technique differs by using mostly transabdominal access with ultrasound instead of an endoscope. He reported a 96% success rate in obtaining chorionic material but with a high incidence of bleeding and infection. The approach was abandoned as amniocentesis became more popular due to higher safety levels
1973-1975 -- Further study into chromosomal analysis from CVS
Kullander and Sandahl in 1973 and Hahnemann in 1974 further researched fetal chromosome analysis using transcervical biopsy before termination in early pregnancies. [2] In 1975 the first successful diagnostic use of chorionic villi was reported at the Tietung Hospital in China. [3] This is where fetal sex was diagnosed for the purpose of sex pre-selection. They claimed to have 94% diagnosis success and only 4% miscarriage rate. Researchers in the United States were, however unable to duplicate the results and so the idea of CVS diagnosis was again abandoned for some time.
1980-1983 -- Change from endoscopic examination to ultrasound to guide CVS
With the invention of the ultrasound and advancement in molecular genetics, an earlier prenatal diagnosis was now sought after. So Kazy et al. in 1980, began using both the endoscope and the ultrasound for fetal sexing on chorion biopsies. This was the first report of using ultrasound guidance during chorion sampling. After Kazy et.al. began using the ultrasound for guidance, many others followed. Niazi et al., Ward and the Brombati group all started using ultrasound guided CVS. Techniques quickly improved and success rate of obtaining chorionic material rose from 75% to 96% [4]
1984-1986 -- The introduction of transabdominal CVS
In 1984, Smidt-Jensen and Hahnemann in Copenhagen introduced transabdominal CVS using ultrasound guidance.[5] With less chance of infective complications the procedure has become more popular than the transcervical method in many prenatal diagnostic centers. Other ultrasonic techniques and modifications were explored by the Brambati and Simoni group and the Golbus group in 1985. [6] The Golbus group reported in 1986 a miscarriage rate of 3.8%.[7] Subsequently, many other centres reported a much lower miscarriage rate of 1.5% which made the procedure safe for routine use.
Current associated research
Chorionic Villus Sampling (CVS) is one of many prenatal diagnostic tools for expectant mothers, it is popular since it can be used to identify potential problems with a fetus at a very early stage. However, the procedure does carry some risks, as does any invasive diagnostic procedure. As chorionic villus sampling is a relatively new technique, made available for safe routine use only 20 years ago, the current associated research is mainly associated with risks associated with the procedure, and ways to overcome these risks. The next section in this page will discuss the current research on CVS and the risks involved.
Risks
When Chorionic Villus Sampling is performed, a small sample of the placenta is removed for analysis. The placenta contains fetal material, therefore can reveal genetic defects which may lead to problems or abnormalities. [8] This prenatal test can be performed as early as 11 weeks into the pregnancy, this is earlier than many prenatal diagnosis tests, which is why many parents choose CVS as they can have solid information earlier in the pregnancy. Some common risks which are not under current research include: Cramping, light blood spotting, pain, fever and chills, leakage (which can be a major concern as it can lower amniotic fluid to a dangerous level for the infant), and potential for missing fingers and toes in the newborn. For this reason, the procedure is only recommended for women who are at least 11 weeks pregnant. [9] The other major risks that are currently being researched are outlined below
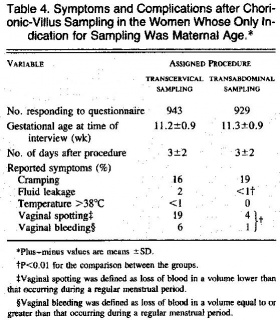
Transabdominal vs Transcervical CVS. Comparison of risks
This table shows the symptoms of women approximately 3 days after sampling. The table shows women who had undergone transcervical sampling had higher frequencies of fluid leakage, vaginal spotting, and bleeding. When a tenaculum is not used, the frequency of vaginal spotting and bleeding persisted in the transcervical-sampling group. Only two women, both in the transcervical-sampling group, had a temperature above 38°C. [10]
Age
Miscarriage
One of the biggest risks of Chorionic Villus Sampling is miscarriage. In one to 100 or 200 cases, the procedure is linked with miscarriage. [11] In an experienced clinic, this rate may go down to one in 300 to 400. To lower the risk of miscarriage with Chorionic Villus Sampling, it is recommended the procedure be performed by an experienced clinician
Hypertensive disorders of pregnancy
Malformations
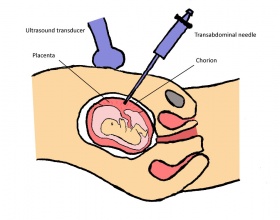
Description of technique
CVS can be performed in two ways, through the cervix (transcervical) or through the abdomen (transabdominal). Both techniques are equally safe when performed by an experienced technician, however miscarriage rates are somewhat higher when done through the cervix. Prior to the procedure, an abdominal ultrasound can be performed to locate the position of the uterus, and the placenta. A full bladder is not required. Depending on the type of method performed, the vulva, vagina, cervix or abdomen are cleaned with antiseptic. The procedure normally takes only 1-2 minutes to perform and the patient is able to leave the clinic within the hour after the fetus is checked.
Transabdominal Procedure
- A local anaesthetic is first applied to the abdomen.
- A thin hollow needle is then inserted through the abdomen into the uterus and into the edge of the placenta where the chorion is located. An ultrasound transducer is commonly used to guide the needle during the procedure.
- A finer syringe needle is then passed through the outer needle, and the tissue is then drawn.
- The sample is taken to the laboratory for testing.
Transcervical Procedure
- A speculum is inserted in the vagina and the area is cleaned with antiseptic.
- With the help of ultrasound imaging, a thin cannula is then inserted through the cervix and uterus and into the placenta.
- The tissue sample is then taken up through the cannula.
Abnormalities found by CVS prenatal diagnostic technique
The cells collected by CVS are sent to a cytogenetics laboratory. There the cells are cultured (stimulated to grow and divide) for 10-14 days. After enough cells are obtained, a banded karyotype is performed. This means that the fetal chromosomes in the cultured cells are stained and subsequently photographed. The photographed chromosomes are then ordered by number, counted and checked for structural abnormalities. There should be 46 chromosomes, 23 pairs. A boy's karyotype is described as 46,XY and a girl's karyotype is described as 46,XX.
Useful links
Search Bookshelf Chorionic villus sampling
Search Pubmed Now: Chorionic villus sampling
References
- ↑ <pubmed>5691288</pubmed>
- ↑ <pubmed>4766093</pubmed>
- ↑ <pubmed>811431</pubmed>
- ↑ <pubmed>7208019</pubmed>
- ↑ <pubmed>6463023</pubmed>
- ↑ <pubmed>4088973</pubmed>
- ↑ <pubmed>3717235</pubmed>
- ↑ <pubmed>20664398</pubmed>
- ↑ <pubmed>20051662</pubmed>
- ↑ Jackson, L.G., Zachary, J.M., Fowler, S.E., Desnick, R.J., Golbus, M.S., Ledbetter, D.H., Mahoney, M.J., Pergament, E., Simpson, J.L., Black, S. & Wapner, R.J. 1992, "A Randomized Comparison of Transcervical and Transabdominal Chorionic-Villus Sampling", New England Journal of Medicine, vol. 327, no. 9, pp. 594-598.
- ↑ <pubmed>19155918</pubmed>
Glossary
Amniocentesis - A prenatal diagnostic test involving sampling of amniotic fluid by needle aspiration for genetic analysis.
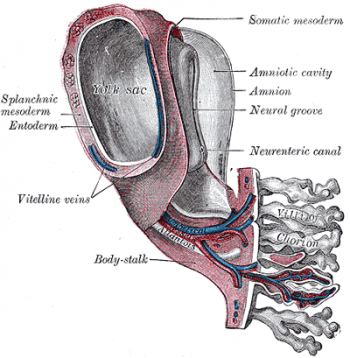
Amnion - An extraembryonic membrane ectoderm and extraembryonic mesoderm in origin and forms the innermost fetal membrane, produces amniotic fluid. This fluid-filled sac initially lies above the trilaminar embryo disc and with embryoic disc folding this sac is drawn ventrally to enclose (cover) the entire embryo, then fetus.
Amniotic cavity - The fluid-filled (amniotic fluid) extraembryonic coelom (cavity) formed initially by epiblast and then ectoderm and surrounding extraembryonic mesoderm. In humans, it forms the innermost fetal membrane, produces amniotic fluid expanding to fuse with the chorionic membrane during week 8 of development.
Amniotic fluid - The fluid that fills amniotic cavity totally encloses and cushions the embryo.
Chorion - The extraembryonic membrane generated from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange. Chorionic villus sampling (CVS) - The taking a biopsy of the placenta, usually at the end of the second month of pregnancy, to test the fetus for genetic abnormalities.
Chromosome - double stranded DNA coiled around histones. Condenses during mitosis and meiosis.
Ectoderm - One of the initial 3 germ cell layers, which will form the nervous system from the neural tube and neural crest and also generates the entire epithelial layer of the skin covering the embryo.
Endoscope - a long slender medical instrument for examining the interior of a bodily organ or performing minor surgery
Endoderm - One of the initial 3 germ cell layers (ectoderm, mesoderm and endoderm) formed by the process of gastrulation. The endoderm forms as a cuboidal epithelium and contributes not only to the trilaminar embryo, but also lines the yolk sac. It will form the entire epithelial lining of the gastrointestinal tract (GIT), contribute to the accessory organs of GIT and also forms the epithelial lining of the respiratory tract.
Fetus - In mammals, term describes the period of development following the embryonic period. In humans, the development week 9 to 36 is the fetal stage (second and third trimester). (see fetal period above). This term is also used non-scientifically to describe the human conceptus at both embryonic and fetal stages of development.
Gene - A DNA sequence that is transcribed as a single unit and encodes a single polypeptide (protein) or a set of closely related polypeptides. There are approximately 20,000-25,000 protein encoding genes in the human genome. In each cell, DNA is found within the nucleus and also within mitochondria.
Gestation - The period of time from conception to birth. A pregnancy with multiple fetuses is referred to as a multiple gestation.
Mesoderm - The middle layer of the 3 germ cell layers of the trilaminar embryo.
Miscarriage - A general clinical term for the loss of embryo or fetus by spontaneous abortion.
Mitosis - The normal division of all cells, except germ cells, where chromosome number is maintained (diploid).
Prenatal diagnosis - any of the diagnostic procedures used to determine whether a fetus has a genetic abnormality
Tenaculum - instrument used to grasp the cervix and keep the uterus in place during gynecological procedures.
Termination - The spontaneous or artificially induced expulsion of an embryo or fetus. As used in legal context, the term usually refers to induced abortion.
Transabdominal - In the transabdominal CVS technique, the physician inserts a needle through the abdomen into the placenta. This is also done with ultrasound, to guide the physician
Transcervical - In the transcervical CVS technique, the physician inserts a small tube through the cervix into the placenta. This is done while ultrasound guides the physician
Ultrasound - A non-invasive technique for visualizing and prenatal diagnosis of several features of development including: follicles in the ovaries, the gestational sac, fetus in the uterus, fetal parameters, and the placenta. The technique uses high-frequency sound waves that are reflected off internal structures. These reflections can then be analysed and displayed by computer.
Villi - Plural of villus, which is a thin projection from a surface. A term used to describe the many functional units together of the fetal placenta.
Vitelline arteries and veins - The blood vessels which form in the extraembryonic mesoderm of the yolk sac and anastomose are called vitelline arteries (flow away from the embryo) and vitelline veins (flow toward the embryo).
Glossary Links
- A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers
2010 ANAT2341 Group Projects
Project 1 - Ultrasound | Project 2 - Chorionic villus sampling | Project 3 - Amniocentesis | Group Project 4 - Percutaneous Umbilical Cord Blood Sampling | Project 5 - Fetal Fibronectin | Project 6 - Maternal serum alpha-fetoprotein | Students Page
Cite this page: Hill, M.A. (2024, May 1) Embryology 2010 Group Project 2. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_Group_Project_2
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G