Book - Human Embryology (1893) 1
| Embryology - 20 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Bandler SW. Uterine and Tubal Gestation (1893) William Wood & Company, New York.
| Uterine and Tubal Gestation 1893: 1 Uterine Gestation | 2 Tubal Gestation | 3 Ovarian and Placental Secretion |
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
Part I. The Essentials of Uterine Gestation
Chapter I. The Processes Antedating Uterine Gestation
A. The Trophic Influence of the Ovary
Halban transplanted the ovaries in newly born guinea-pigs to see what effect transplantation and castration would exert upon the development of the genitalia and the breasts. The comparisons with non-castrated animals are very interesting. In the castrated guinea-pig the breasts were later found to be one-fourth the normal size; the genitalia were small, the vulva was one-third smaller than normal ; the uterus was as small as at birth, showing very slight development of muscle and endometrium, and containing no ciliated cells. The breasts showed no glandular tissue, the mammilla? were hypoplastic, the vaginal mucous membrane showed both squamous and cylindrical epithelium — a novel condition. When the ovaries were transplanted under the skin, the uterus was well developed, the tubes were normal, the vulva was large, as were the mammillae likewise. In the transplantation of one ovary a part of the uterus and a piece of the tube had likewise been taken, and these grew in a normal manner, and increased in size. The transplanted piece of uterus contained well-developed muscle and normally secreting glands. The portion of tube showed muscle, epithelium, and ciliated cells. Halban thus showed the influence of the ovary, as a secreting organ, upon the uterus, vagina, vulva, and mamma. He considers it probable that the ovarian secretion acts upon the uterus ; the uterine secretion acting in turn upon the mammary gland.
Ribbert implanted the mamma of a young guinea-pig, with its covering of skin, into a cut near the ear. The wound healed, and five months after the operation, the animal having borne two young, this mamma secreted milk normally, a proof that the connection between the breasts and the ovary and uterus is to be found in no other channels than those of the circulation.
Hegar and Kehrer showed that in newly-born animals, after castration, the uterus does not develop, but remains at the same stage, or even undergoes atrophy, Sokoloff castrated rabbits and dogs and found that, a short time after, they became fat and apathetic, and grew constantly worse. Subsequent examination of the uterus divulged muscular atrophy, especially of the circular layer ; the vessels were fewer, the walls thicker, the lumen was small and even obliterated. The mucosa, however, remained unchanged. When only one ovary had been removed, there ivas no change in the sexual development of these animals, the young ones evidencing a normal and constant development of the genitalia.
Jentzer and Beuttner examined the organs of cows within one year to twenty-two months after castration, and found all the layers of the uterus atrophied and substituted by connective tissue. The stratum vasculare had greatly changed ; the atrophy of the mucosa, while not constant, was in most cases acute. They castrated rabbits, gave subsequently hypodermatic injections of ovarin, and yet the uterus atrophied. The objections to considering this last procedure conclusive are : 1. That the ovarin of cows was used. 2. That it was given hypodermatically. 3. That there was no sufficient increase in the amounts used. The castration of other rabbits showed that the cylindrical epithelium became lower, the protoplasm degenerated, these processes becoming more defined the longer after castration the animals were examined. The muscularis was found to be atrophied ; the larger vessels were gone. Although glands were present, the mucosa showed decided atrophy. In dogs castration produced atrophy of the muscle, but only after three or four months ; the epithelium of the uterus was lower, the protoplasma cloudy, the glands were degenerated, and the vessel walls thickened.
Knauer transplanted the ovaries of rabbits and dogs between the fasciae of the abdominal wall and into the mesometrium, being careful to remove absolutely every bit of ovarian structure. In the mesentery he fastened the ovary with two sutures between two folds of peritoneum, the ovaries being then nourished through endosmosis or through plasmatic circulation. New vessels grew into the ovarian tissue and furnished its subsequent support ; this change began as early as the fourth day. Examination at various periods showed that a small part of each ovary usually degenerated, and new connective tissue appeared in place of the lost cells. In all cases in which a complete degeneration of the ovaries was found, atrophy of the breasts and of the genitalia had occurred. The muscle of the uterus was atrophied, the intermuscular connective tissue was increased, the mucous membrane was atrophied — changes like those which occurred after double castration. Retention of function on the part of the transplanted ovaries was always evidenced by the growth of follicles in a normal manner, by the ripening of the follicles, and by the discharge of the ova. In all such cases the normal character of the breasts, of the uterus, and of the genitalia ivas preserved, and in the younger animals all these organs underwent a natural development. In one dog with well-developed breasts, thirteen months after transplantation an opening of the abdomen showed the right ovary to be of normal size and to contain three follicles. The left ovary was small. Two months later coitus took place, and after two more months two well-developed young were born. Three years after transplantation had been done, this animal on examination showed externally a normal condition of development of the breasts and the genitalia. The right ovary was the size of a pea and contained follicles ; the left ovary was larger than on the previous examination. The right ovary was covered with germinal epithelium; many follicles but no primary follicles being present. A like condition was found in the left ovary. The uterus was normal in every way ; the mucous lining contained many glands and ciliated epithelium. The breasts were of normal character, with normal secretion and glands. Knauer's results proved that the preservation to the organism of the functionating ovaries preserves the breasts, the genital organs, and the sexual instinct, a result possible only through the absorption into the circulation of ovarian secretion, and that the function which the ovary exerts upon the body stands in closest relation to its ability to form ripe ova. Ovarian tissue which has ceased to develop ova has lost its other function, that is, secretion. Therefore the numerous nerves of the ovary are in all probability only vessel nerves. Knauer transplanted in sixteen cases the ovaries of animals into each other, obtaining the above good results in only two cases, since in the others the ovaries degenerated. This shows that a certain relation exists between the cells of one and the same body. Although difficult, transplantation of ovaries from one animal to another is possible.
Morris removed the adnexa in a human patient and sewed a piece of one ovary into the stump of the right tube. One month later the patient became gravid, aborting in the third month. Into a twenty-year-old girl with uterus infantilis and rudimentary adnexa, with suppressio mensium, he transplanted a piece of the ovary of a thirty-year-old patient, fixing it in the fundus of the uterus. Eight weeks later a profuse menstruation, lasting ten days, occurred. ; after six weeks a normal one lasting five days ; the third one five days later. The fourth and fifth menstruations were normal, at intervals of four weeks.
Glass transplanted an ovary of a seventeen-year-old girl into a twenty-nine-year-old patient from whom both ovaries had been removed two years before. The ovary was fixed in its normal situation through an opening in the sac of Douglas, per vaginam. Sixteen days later occurred a bleeding lasting two days ; six months afterward a menstruation of three days ; eight months after operation the patient showed good color, was of good appearance, with a return to' former mental and body conditions, after two years of artificial climax.
Dudley implanted an ovary into the fundus of the uterus after removal of a pyosalpinx duplex, and regular menstruation continued.
An examination of the uterus after castration in women shows an atrophy of the cervix, an immediate atrophy of the corpus, a sclerosis of the vessels which show a growth of the intima, and an endarteritis obliterans, especially in the larger vessels. Few glands are present, and the connective tissue is increased.
Gottschalk found an exceptional condition in one case, in which the muscularis was well preserved, although the mucous lining had almost entirely disappeared.
Cholmogoroff found the uteri at climacterium to contain 9 large amount of connective tissue, the vessels being greatly sclerosed. I have found the same condition in a high degree in two cases of my own.
Normal menstruation is absolute evidence of the presence of a normally functionating ovary. The absence of ovaries, a poor development of these glands, an insufficient secretion of ovarian substance, or a diversion of ovarian secretion to other organs of the body, always causes a failure of uterine development or uterine atrophy. It is possible that, with partial or total absence or atrophy of the uterus or other genital organs, normal ovaries may be present. It is likewise possible for poorly developed ovaries to be the result of a failure of development of the body in general or to be simply a failure of development of the ovary itself, through embryonal disturbances.
Winckel has shown that, in the development of the uterus and tubes, the situation of the Wolffian Body close to the ducts of Muller may influence, to a very great degree, their growth and is a frequent cause of malformation. The early completion of the Wolffian bodies, their opening into the sinus urogenitalis, the growth of the Muller 's ducts along the Wolffian, and their crossing at that spot where the union of Muller 's ducts finds its upper limit, are anatomical embryological factors easily recognized as causes of uterine maldevelopment and hypoplasia. Further, the origin of the ligamentum ileo-genitale rotundum at this upper limit, its close union with the ducts of Muller, the fact that its line of development in a measure opposes the union of the ducts, in addition to tension, pressure, and torsion exerted by the neighboring organs, such as the Wolffian bodies, the bladder, the ureters, the vessels and nerves of the uterus and rectum, are important factors influencing the development of the uterus. In addition, Winckel recognizes the occurrence of abnormal cells in the septum between the ducts of Muller, and general hypoplasia of the vessel system, as additional causes of maldevelopment. Aside from secondary atrophy, the result of constitutional diseases, the embryological cause here mentioned, and the forms associated with general hypoplasia, we recognize in the ovary and its secretion the factor which governs the development of the uterus, the genitalia, and the breasts, and the factor which is concerned in the preservation of these organs and the regulation of menstruation.
Eberlin 1 describes a patient with vaginal defects, who, in her eighteenth year, had vicarious menstruation from the nose at regular intervals for six months, after which no recurrence was noted. Her mammae and external genitalia were small. She suffered from molimina menstrualia every three weeks, at first for periods of three to four days. Eventually severe pain was experienced constantly, associated with sickness at the stomach and vomiting. Laparatomy divulged a uterus rudimentarius, with absence of the adnexa of the left side. The right tube and ovary were almost normal. The uterus was 3.5 centimetres in length, differing microscopically in nowise from the normal as regards muscle, but possessing no cavity. The ovary showed a thickening and a hyaline degeneration of the vessel walls. In addition to the corpus luteum, very few follicles but no Graafian follicles were present. After castration all the annoying symptoms disappeared.
Fritsch operated in a like case in which severe molimina men^ineberg, Am. Jour, of Obstet., No. 4, 1898.
strualia, sickness at the stomach, and rectal bleedings were the indications.
In all, Eberlin finds twenty-one cases of this sort associated with vagina] defect to have been operated upon. The ovary in the above-cited case of Eberlin, though containing few follicles, nevertheless secreted sufficiently to cause the severe symptoms. Since no endometrium was present, and no excretion by that channel took place, the ovarian secretion, through cumulative action, was responsible for the severity of the pain. Whatever part the uterus took in these attacks must have deen the result of uterine contraction, since congestion alone is not responsible for so much pain, as is evidenced by the absence of such suffering in pure congestions of the uterus, associated with metritis, etc.
B. Constitutional Changes Dependent on the Ovary
Were we to consider the relation between the ovary and the uterus, and between the genitalia and other organs to exist through the medium of the cerebro-spinal or sympathetic systems, why should we find the walls of the tubes thin and containing more connective tissue in cases of poorly developed ovaries and at the menopause, when no primary follicles and no Graafian follicles are present in the ovaries? The uterus then shrinks, the walls become thin and flabby, the mucous membrane atrophies, the connective-tissue elements are more prominent, and the ciliated epithelium disappears. Is it not extraordinary to make the occurrence of these decided changes dependent upon a cessation of ovarian congestion? That these differences are not due to the lack simply of reflex stimulation on the part of the ovary is sufficiently evidenced by the constitutional changes occurring at puberty, at menstruation, during pregnancy, and at the menopause. The relation between the changes occurring at puberty and at the menopause, before menstruation and after menstruation, during pregnancy and after pregnancy, show a decided resemblance. Until shortly before each menstrual period, temperature, pulse, muscular activity, lung capacity, and the excretion of urea increase, and reach their maximum two to three days before the appearance of blood. During this period we find hyperemia, edema, increased activity of the ovary, changes in all the mucous membranes, and increased function of the glandular apparatus. The occurrence of swelling of the breasts, tenderness of the abdomen, even pain and the passage from the vagina of increased mucus, sometimes mixed with blood, prove at the beginning of each menstrual period a wave movement and an increased blood tension by no possibility due to reflex causes. During and after menstruation regressive changes are evident, and the excretion of nitrogenous elements is diminished.
During pregnancy we have an increased amount of the watery elements of the blood, an increased proportion of fibrin, a diminished amount of albumin, an increase in the white blood cells, a genuine increase in the number of red blood cells and in the amount of hemoglobin.
Before labor the temperature is highest in the last three months of pregnancy, and there is an increase in the elements of the body, equal to one-thirteenth of the body weight. This increase is due to serous infiltration, and to the increased ability of the body to form organized tissue. Post partum, after a temporarily short rise, the temperature is lower, the blood pressure sinks, and becomes normal on the ninth day. The loss in body weight is equal to one-ninth of the weight of the pregnant person. For labor and post partum together, there is a loss of weight nearly equal to one-fifth of the body weight at full term. After labor there is a diminution of tissue change and a diminution in the amount of urine.
Therefore as regards temperature, blood pressure, body weight, the amount of urine secreted, etc., there is always a similar increase before menstruation, and a like decrease in intensity during and after menstruation, as during and after parturition, so that Virchow has well characterized menstruation as being a labor en miniature.
According to Loewenthal, who believes that every ovum is embedded in the mucous membrane of the uterus, we may say that labor is a menstruation in which a fully developed ovum is expelled. The coincidence of labor with a menstrual period seems therefore natural. The resemblance of the mechanical processes concerned in menstruation and in labor is remarkable, and these changes can be due only to the stimulative effect of the ovarian secretion, acting not alone upon the uterus and the genital organs, but likewise upon the breasts, upon the blood elements, and upon blood tension. This secretion is a stimulus likewise to uterine contractions, and is the probable cause of the contractions normally occurring during pregnancy. The action of this accumulated secretion upon the uterus at the end of pregnancy is probably the cause of labor pains.
The action of the ovarian secretion upon pulse tension, and its effect upon the mucous membranes of the body generally, are likewise evidenced by the congestion of the vocal cords during menstruation, so that during this time the singing voice is poor. The secretion of intestinal mucus is also greater, there is increased perspiration, the lower turbinated bones are swollen, and the eye suffers limitations in power. The best evidence of the constitutional elements involved in the process of menstruation is the occurrence of vicarious menstruation. Under this designation ice consider bleedings occurring at regular intervals in a patient suffering from amenorrhea. The most frequent spot for this bleeding is the nose, usually the lower turbinated bones.
Fleiss described a two-year-old child with well-developed pubes and breasts who had periodical bleedings from the nose. In a second case, a girl fourteen years old, well developed, suffered from regular bleedings from the nose, which stopped, however, Avhen real menstruation began. In another case the regular nose bleedings at intervals of twenty-nine days stopped during pregnancy, only to begin afterward, and after a continuation of eight months ceased again on the occurrence of a second pregnancy. Bleedings of the same kind have been described as occurring regularly from other mucous membranes, the trachea, the lungs, and the stomach. In the latter instance the bleedings were not always associated with vomiting, the blood being usually found in the feces. In other cases there were bleedings into the thyroid gland. In cases with poorly-developed uteri, these bleedings disappeared only when the uterus began to functionate properly.
The secretion of the ovary exerts through the medium of the blood a stimulating effect upon the breasts, noticeable before menstruation, during pregnancy, and during the period of lactation .
(ioltz cut through the cord of a dog at the level of the first lumbar vertebra, and later saw the signs of rut appear. After coitus one dead and two living young were born. The breasts were well developed, and lactation and nursing followed the normal course. Since these changes, the sexual tendency and the process of labor could not have been excited through the cord, it must be that a certain secretion of the ovary, acting through the medium of the circulation, gives the stimulus for the exercise of those functions.
Ovarian secretion exerts a most decided effect upon the development of the uterus and the genitalia, as well as upon the breasts. It is absolutely necessary for the preservation of the developed uterus, the other genitalia, and the breasts. An overproduction of ovarian secretion or a disturbance in the function of the ovary causes pathological changes ; an under-production of ovarian secretion is likewise the cause of pathological conditions. The production of ovarian secretion and its action for a certain period of time are the probable causes of the pains of labor.
C. Menstruation
Menstruation is the periodical loss of blood from the uterus or from any mucous membrane, occurring for the reason that no fecundated ovum is present in uterus or tube, and may be divided into three periods : the premenstrual, the menstrual, and the postmenstrual. During the premenstrual period, the ten days immediately preceding the appearance of blood, the following changes take place :
The superficial capillaries become greatly dilated, and serous infiltration of the endometrium takes place, which separates the meshes of the stroma, accompanied by a gradual but decided dilatation of all the blood vessels and lymph channels. There occur a growth of round cells in the interglandular tissue, and an entrance of leucocytes into the mucous membrane. The glands become larger and wider, being often filled with secretion.
This swelling of the mucous membrane, the dilatation of the blood vessels, the production of round cells, and the growth of the superficial layer of the endometrium produce the so-called decidua menstrualis. Although in the connective tissue large cells, not to be distinguished from young stages of decidua cells, are found, it is to be noted that typical decidua cells do not, as a rule, develop at this time in the superficial layer. The endometrium is at this period from 6 to 7 millimetres in thickness.
The period during which blood is thrown out is the next, or menstrual period. The superficial capillaries are greatly dilate'!, and an exit of blood elements, not dependent on a bursting of the capillaries, goes on for several days. The bleeding occurs partly through diapedesis, and, in strong bleedings, through rhexis. There is little or no destruction of the mucosa, only a very slight fatty degeneration of the epithelium of the uppermost layer, so that in the excreted blood relatively few epithelial cells are found.
After menstruation, the uterus shows an almost continuous covering of epithelium, interrupted in spots, especially if pathological processes be present. Most of the ciliated epithelium is preserved. The first stimulus to bleeding is due to contraction of the uterus, which at the height of congestion is possibly accompanied by contractions of the tube. During menstruation the uterus is larger and in the first few days following likewise soft and flabby. The flabbiness lasts longer than the bleeding. A spontaneous dilatation of the cervix canal takes place, and reaches its height on the third or fourth day. This dilatation takes place without regard to the amount of blood discharged, whether the menstruation be painful or painless. The cervix is hyperemic, the glands showing an increased secretion of mucus. The blood thrown off is mixed with the mucus of the uterus and cervix, and later with the acid secretion of the vagina, for this reason coagulating less easily than other blood.
The secretion from the sebaceous glands of the external genitalia is responsible for the peculiar odor present in some cases, and in nowise differs from that observed in the axilla. On the inverted uterus the blood has been observed to appear in single drops from the region of the openings of the glands. The endometrium is then covered with white and bloody mucus, the openings of the glands being clearly seen. There is no degeneration or destruction of the mucous membrane. The changes in the tubes, if any, are slight (Gusserow).
The next, or postmenstrual period comprises fourteen days, during which the mucous membrane returns to a thickness of 3 millimetres. During this time all cells not capable of further growth are thrown off, and the epithelium, only partially denuded, is regenerated. The epithelial cells found singly or in groups in the lumen of the glands disappear by resorption, and partially by phagocytosis. From the sixth day after the beginning of menstruation, cell division is prominent. It is probable that mitosis takes place, even during the exudation of blood. The presence of mitosis in the leucocytes is an evidence of growth of the interstitial tissue during menstruation.
Regeneration concerns the stroma, the glands, and surface epithelium, reaching its height on the fourteenth or fifteenth day after the beginning of menstruation. The mucous membrane becomes pale, the glands and vessels have returned to their normal state, the lost epithelium has been restored. From the middle of the third week on there is a diminution in mitosis.
Menstruation is not a process by which the mucous lining of the uterus is thrown off, with subsequent regeneration previous to the next menstruation. It is simply the excretion of blood from the decidua menstrualis occurring for the simple and sole reason that there is in the uterus no fecundated ovum.
Ovarian secretion is the direct cause of this periodical swelling of the mucosa, and it continues, if fecundation has taken place, to exert, not alone a local, but likewise a stimulating influence on the general and sexual organs. This stimulation occurs to a heightened degree during pregnancy, and on removal of the uterus, since the secretion is ordinarily excreted during menstruation. On the occurrence of pregnancy, this secretion causes a further development of the uterus and the decidua, and plays an important part in the process of labor; it stimulates the functions of the breasts, exerts a decided constitutional stimulation, and is the cause of many of the pathological conditions occurring before and during labor.
The generally accepted view as to the relation between ovulation and menstruation is that of Pfliiger. The increase of the contents of the Graafian follicle, which results through the secreting activity of the cells of the membrana granulosa, is said to stimulate the nerves running in the stroma and ending in the cells. The increasing tension reflexly irritates the vasomotor centre, with resulting dilatation and congestion of the uterine vessels. At the height of this congestion the follicle is supposed to burst, through pressure. As congestion and tension in the ovary are supposedly the reflex causes of the congestion of the uterus and pelvic organs, menstrual bleeding is considered a result of periodical ovulation. This theory obtained support through the experiments of Strassman, who showed that increased tension in the ovaries of animals, produced by the injection into them of fluid, caused swelling of the mucous membrane of the uterus. In answer it may be asked why the same condition does not result in all cases of ovarian tumors and ovarian cysts, which may develop entirely beneath the albuginea.
This theory of Pfliiger and the experiments of Strassman have been generally quoted to prove the causal relation of ovulation to menstruation. The congestion in the ovary, and the swelling of the Graafian follicle, must then, through the nervous system, stimulate the uterus to congestion, with a resulting periodical bleeding. The cessation of menstruation after castration has likewise been cited as proof of the fact that without ovulation there could be no menstruation, since the periodical hyperemia reflexly caused by ovulation no longer takes place. By others it was considered that the distension of the ovary, occurring periodically, exerted an action upon the vasomotor system, then causing congestion. The atrophy of the uterus after castration was likewise pointed out as a proof of the resulting diminished Mood supply, ordinarily furnished by this reflex action of the ovary. On the other hand, it has been frequently stated that the result of castration was due to the tying off of the arterise spermatica? internas, and that the resulting anemia was the cause of atrophy of the uterus, and of the diminution in the size of the uterine myomata.
Rein cut all the sympathetic and all the spinal nerves running to the uterus in a dog, and yet the animal bore young. Inasmuch as the uterus, freed from the central nervous system, performed its functions as before, he concluded that a regulating nerve centre exists in the ovaries. All this was taken to prove that menstruation was a result of reflex action originating in the ovaries.
D. The Action of Ovarian Secretion on the Endometrium
The periodical swelling of the mucous membrane is due to the secretion given of by the ovary, and the experiment of Strassman proves that the forcing of an additional amount of this secretion into the circulation only enhances this effect. That ovulation and menstruation, or at least the latter, occur with a certain regularity is a fact which we are not able to explain any more than we can say why in malaria the plasmodia are thrown into the circulation at regular intervals, or why the menopause usually occurs at a certain period. At any rate, were menstruation the direct result of periodical ovulation, we should still be in need of a satisfactory explanation for the latter phenomenon. No other theory is satisfactory than that of secretion. Ovulation and menstruation are evidences of the functional capability of the ovary. Since ovulation may occur without menstruation, but the latter never without the former, we have here an evidence that a certain functional activity of the ovary is necessary to stimulate the mucous membrane to its periodical changes. That after double castration regular bleedings may occur for a certain period is proof of the independent role which the endometrium, to a certain degree, plays in the process of menstruation, for sufficient of the secretion of the ovaries may still remain in the circulation to produce the normal processes after removal of the ovaries. The part which the ovaries play in the development of the body, the effect of their presence upon the breasts and the genital tract at puberty, before each menstrual period, at the menopause, and after castration, are sufficient evidence of their secreting power. The experiments of Knauer and others prove that it is simply the presence of the ovaries, and the preservation of their secretion, which are of importance to the body, and that their action upon the uterus is in nowise reflex in character, since when removed and implanted elsewhere, and in this way loosened from their connection with nerve plexuses and the nervous system, every sexual peculiarity is absolutely preserved.
Menstruation is simply an evidence that a fecundated ovum is not present in the tube or in the uterus. Practically no part of the endometrium is thrown off. It seems as if the blood thus lost simply gave an exit to the secretion of the ovary, which, if retained too long in the body, produces in pregnancy certain normal changes, and in a large number of cases abnormal processes. In pregnancy the ovarian secretion stimulates the uterus to enlargement and growth, it stimulates the formation of blood, produces tension and congestion in the vascular system, and stimulates the function of the breasts. After labor, lactation is stimulated by this secretion, so that little or no effect is exerted upon the uterus ; therefore it rarely undergoes the periodical stimulation and has a tendency to atrophy. The changes occurring in the decidua menstrualis and the decidua graviditatis are certainly evidences of the action of a secreted substance. The method in which the ovum is embedded in the decidua, and the processes occurring in its immediate vicinity, as well as the fact that in extrauterine gravidity a decidua graviditatis is formed in the uterus, with decided enlargement of this organ, are likewise proofs of this fact.
E. The Relation of Ovulation and Menstruation
As a matter of fact, ovulation and menstruation are related only in that both are the result of the secreting function of the ovary, and are in nowise connected as regards cause and effect. The ovum is the external secretion, the internal secretion entering the blood through the lymph channels. The ripening and expulsion of an ovum may occur at any time. It is, however, a fact that menstruation occurs only after the ovary is capable of producing ripe ova, and whether the egg be expelled, or occasionally degenerate in the follicle, is immaterial. The independenee of ovulation and menstruation is evidenced by the fact that the former takes place before menstruation has appeared, and likewise after the menopause, as is proven by cases, by no means rare, of pregnancy in girls who have not yet menstruated, as well as by the occurrence of pregnancy at variable periods after the amenorrhea of the climacterium. In children the primary follicles develop fully before puberty, and the same development occurs even in the fetus and in the newly born. Those ova and follicles go through the same stages of development an. I ripening as in the case of adults. That they are not capable of fecundation is shown by the fact that the ova are only one-half as large as in adults. In those cases, however, of young children with well-developed breasts and genitalia, when menstruation begins there is an unusually strong development of the body, and the ova, as well as the follicles, differ in no way from those found in menstruating adults.
Leopold found that in forty-two pairs of ovaries, thirty pairs showed a corpus luteum belonging to the last menstruation. In thirteen pairs no follicles were found which, on account of their size or the swelling of the follicle, justified a belief that a bursting of any follicle would have occurred at the next menstrual period. In twelve cases no corpus luteum was found belonging to the last menstruation. One case showed a follicle which had burst between menstrual epochs.
Arnold found that in fifty-four cases, only thirty-nine showed the presence of fresh corpora lutea after the last menstrual period.
Williams found this to be the case in twelve cases out of sixteen. Therefore, ovulation, although in the majority of cases occurring at or near the menstrual period, is not the cause of the same.
Leopold has shown experimentally that in the inter-menstrual period follicles ready to burst are present, and that through certain causes, such as coitus, the exit of an ovulum may result at any time. That ovulation occurs during pregnancy is proved in the case mentioned by Kroenig, in which conception occurred as a result of coitus four days post partum. The relatively frequent occurrence of pregnancy during the temporary amenorrhea of lactation is a proof of ovulation during this time.
Consentino finds that during pregnancy and lactation ovulation continues. Although the ovum of a menstrual period may be fecundated immediately thereafter, the ovum usually fecundated is the one given off between four and eight days before menstruation, the egg thus belonging to the period, so to say, first omitted. The ovum retains its vitality for an average period of twelve days, and yet out of a collection of two hundred and fourteen pregnant cases, in sixty- five coitus had taken place after the twelfth day following menstruation. Therefore, in these pregnancies at least, the ovum must have belonged to what may be called the next awaited menstrual period. Even if the expulsion of the ovum occur only a few days before that time, its fecundation is not difficult to explain, nor are the cases puzzling in which one coitus directly after menstruation produces pregnancy, as the spermatozoa retain their vitality for a long time, and have been preserved, in proper temperature, for a period of eight days. Duhrssen has found spermatozoa in the tube three and one-half iveeks after the last coitus.
It is therefore evident that ovulation, as a rule, occurs from four to eight days before menstruation, but it may occur at other periods, as ripe ova, practically speaking, may be present at almost any time.
F. Ovulation
The other of the functions of the normal ovary is the production and expulsion of ova capable of being fecundated. It is probable that after birth no new ova are formed from the germinal epithelium. At and after puberty we judge the vitality of the ovary by its ability to bring these ova to a stage which may be called ripe. For the expulsion of an ovum from the Graafian follicle, a gradual increase in size of the follicles takes place, depending partly on an increase in the amount of liquor folliculi. The cells of the follicle epithelium undergo fatty degeneration, and the internal layer, the tunica interna, shows an increase in the size of the cells, and a decided development of the blood vessels. The protoplasm enlarges greatly, begins to take on a yellow color, and these cells, now lutein cells, are arranged in several layers, forming an irregular surface. As a result of the fatty degeneration of the follicle epithelium, the ovum is freed from the cumulus oophorus. The most prominent point of the follicle is poor in blood supply, and furnishes the so-called stigma folliculi. It is here that the opening takes place which serves as an outlet for the ovum. This opening is probably the result of the reaction or chemical effect produced by the ripe ovum, since in the newly born, and in children, follicles of the same size and even larger ones exist without bursting — the so-called atresic follicles. The facts that large follicle cysts occur in the ovary without opening, and also that in women in whom the unopened follicles degenerate, disturbances of menstruation occur — so-called missed ovulation — speak for a chemical reaction as probably one of the functions of the ripe ovum. That the orgasmus venereus does play a part in hastening the expulsion of the ovum is not to be questioned. In most cases the opened follicle is then filled with blood which likewise empties into the peritoneal cavity, and the so-called corpus luteum spurium results. If pregnancy takes place, this body develops decidedly, forming the corpus luteum verum (Nagel).
After ovulation, the ovum is thrown out into the abdominal cavity, and then, influenced by the wave movement of the ciliated epithelium of the tubes, the fimbria? of the ampulla, and the fimbria? ovarica?, finds its way into the uterus. It is not necessary that the tube should grasp or surround the ovary, since it would embrace, even under favorable circumstances, only part of the ovary. This wave movement of the ciliated epithelium causes a current in the peritoneal plasma, which directs the ovum into one or the other of the tubes.
Lode injected, with a needle pointed toward the diaphragm, the eggs of ascarides into the abdominal cavity of rabbits, in the region of the umbilicus. After ten hours, without the excitement of coitus, he found these eggs in the tube. An interesting proof of the existence of this current is given by Knauer, who removed the ovaries of dogs, and sewed them into the mesentery. In one case, on opening the abdomen he saw in one of the ovaries three ripe Graafian follicles. Shortly after, coitus took place, and in due time two young were born. A further proof is found in the experiments of Leopold, who showed that an ovum given off by one ovary may enter the tube of the other side. The cases are not rare in which the tube of one side was closed or absent, and although the corpus luteum verum was found in the ovary of the same side, yet the ovum was found in the uterus. The same is true of those cases in which the corpus luteum verum is on one side, and the ovum develops in the other tube, or in the horn of a uterus unicornis of the opposite side. Therefore it is certain that, normally, a wave current exists on either side of the uterus, and that the ovum is attracted by the stronger current, usually that of the side from which it came, possibly, however, by the current of the other side.
It is therefore evident that an ovum, by natural means, may at any time enter the tubes, and that no congestion of the tube, no erection of the tube, and no reflex spasmodic grasping of the ovary by the tube are necessary.
Lode has shown that an ovum finds its way through the tube into the uterus in thirty hours.
Ohapter II. The Embedding of the Ovum in the Guinea-Pig
A. Uterus of the Guinea-Pig
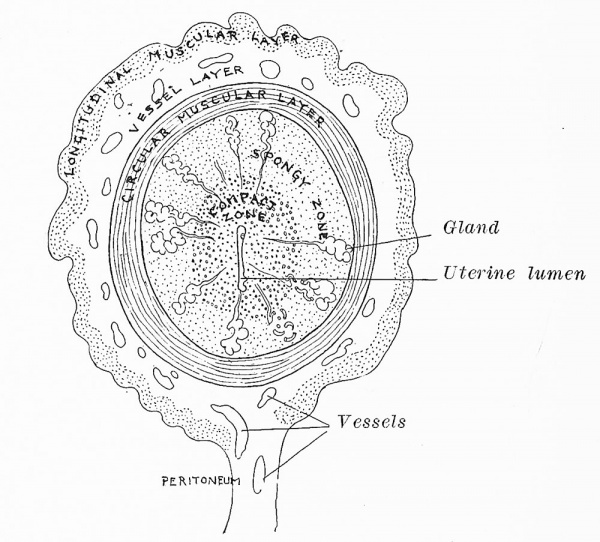
The uterus of the guinea pig is six centimetres long and consists of two muscular layers, an external longitudinal one closely connected with the peritoneum, and an internal circular one. Sometimes, within the latter, are found isolated bands of longitudinal fibres.
Between the two muscular layers is a broad zone of loose connective tissue, and in this are found the continuations of the vessels which enter through the longitudinal layers at the mesometral area. All the larger vessels are in the circular layer. Their walls lose the muscularis and their continuations then enter the specific parenchyma of the uterus, where they appear as capillaries or simple endothelial channels.
Fig. 1. Half-schematic section of the uterine horn of a guinea-pig. (v. Spee.)
The uterine lumen is lined with a single uninterrupted layer of cylindrical epithelial cells ; no cilia are clearly seen. This epithelial layer descends into the connective tissue at numerous places, into glands lined with a low epithelium. The peripheral ends of the glands are twisted and extend up to the circular layer. An active increase of epithelial cells through mitosis takes place only in the end areas of the glands, so that here the regenerative stations for the uterine epithelium are to be sought. In other areas of the uterine lining the epithelial cells have lost the power to produce new cells. This is the case in animals in whom the epithelium plays no part in the formation of the placenta.
The connective tissue consists of two zones separated by a transition zone. (1) A peripheral zone surrounding the twisted gland ends and consisting of spindle or branching cells with intervening spaces, resembling a loose reticular connective tissue. (2) A central compact zone situated between the straight excretory ducts of the glands. In the implantation of the ovum only this area is invaded. Extremely numerous mitoses, and the varying appearance and thickness of their tissue, are proofs of active changes and an increased tissue change. Since at points not important the strongest cell increase may be found, the conclusion is justified that the life of the connective-tissue cells of the uterus is short. There are no spindle-shaped or branching cells here as are found in the peripheral zone.
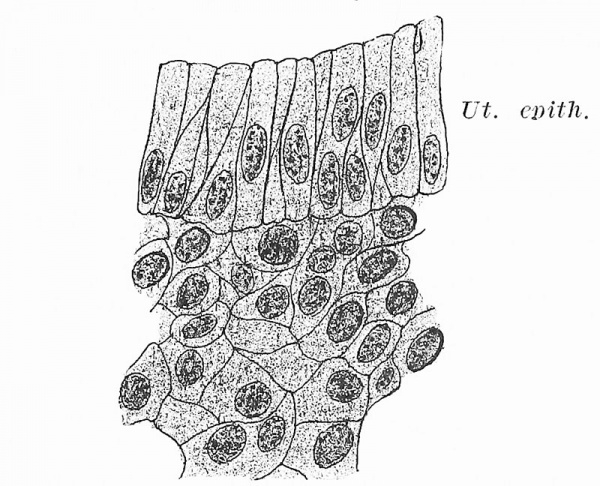
Fig. 2. Cells of the compact zone with the epithelial lining of the uterine lumen of the guinea-pig. (v. Spee.)
The cells of the central zone (Fig. 2) lie like the cells of stratified epithelium. They are polygonal, close together, generally separated by sharp contours, which are probably intercellular spaces. The most firmly uniting basis is furnished by the capillary network, for a real connecting factor among the elements of the connective tissue, especially of the compacta, is not present. The normal relation is preserved by the firmly united epithelium and the circular muscular layer, between which lie the two layers of connective tissue.
B. The Embedding of the Guinea-Pig's Ovum
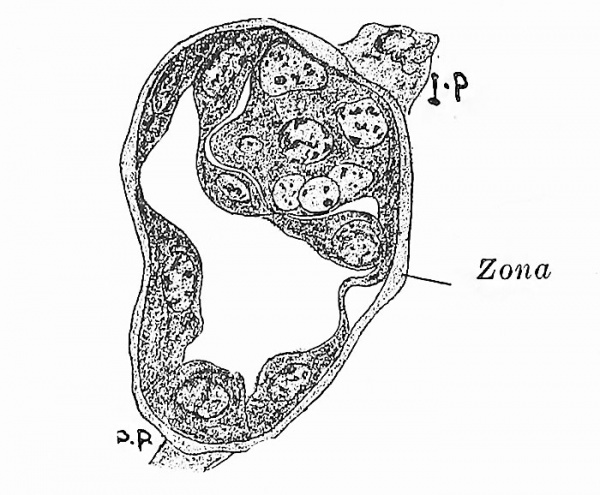
In 1883 Spee stated that on the sixth day post coitus the ovum of the guinea-pig is an oval germinal vesicle one-tenth of a millimetre in diameter, surrounded by a zona pellucida and lying free in the uterine cavity (Fig. 3). The cell wall of the vesicle, the germinal layer, consists, in the region of the ovum's equator, of a single layer of very flat cells. At the two poles the wall seems thicker. At one pole the cell wall of the vesicle is stratified and forms a prominence into the cavity of the vesicle, the Germinal Prominence of Hensen or the Placental Pole (P. P.). At the other pole (the Opposite Pole of Spee) the germinal layer consists of a single layer of cubical cells, constituting the Implantation Pole (LP.). It forms after implantation that summit of the ovum into which the embryonal sphere enters and in which the embryo develops.
Fig. 3. Ovum of guinea-pig free in the uterine cavity. Ovum with zona. Note. — The lettering of Pig. 3 is reversed, (v. Spee.)
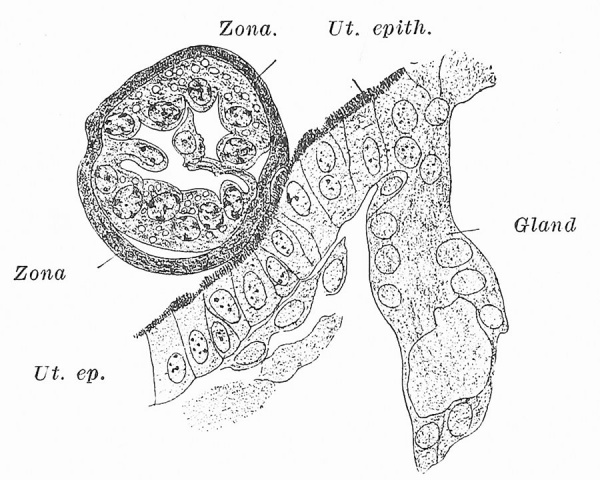
The zona is preserved up to the beginning of the seventh day post coitus and can be readily seen on the free germinal vesicle. The cubical cells of the Implantation Pole send prolongations of their cell bodies through the zona and can enter into direct relation with the epithelial lining of the uterus before the zona is lost finally to the ovum, and may so furnish the first connection ivliich leads to implantation. These prolongations have been seen only in the region of the Implantation Pole. The short period, during which the prolongations of the Implantation Pole hold the ovum fixed to the uterine epithelium, however, has not been observed.
When the ovum is first attached to the uterine epithelium the zona is present (Fig. 3a), but disappears in a very short time, for it is not seen in embedding ova. Probably the Implantation Pole prolongations perforate it and cause its disappearance at these points. The rest is probably rubbed off. In irrigating a uterus for ova, Spee once found the cell body of an ovum and an empty zona with a hole large enough to have permitted the former to slip out. Acids dissolve the zona, and, as these were often used in fixing the specimens, the fact that no zona was found in the youngest ova which had entered the uterine wall does not prove that the ova were embedded after removal of the zona. The ova during implantation, however, are so closely surrounded by uterine tissue that between them there is no room for a zona, and so in all probability the ovum does not take the zona with it into the uterine wall.
Fig. 3a. Ovum of guinea-pig in its first adhesion to the uterine epithelium. Ovum still possesses its zona. (v. Spee.)
The Embedding or Implantation of an Ovum includes the group of processes which result in the ovum entering from the uterine cavity into the connective tissue of the uterine wall. The processes antedate the formation of the placenta and are distinct from the processes of placental formation, hut the first evidences of the latter follow immediately upon implantation. In the guinea-pig, ova are never implanted at a point at which or in whose neighborhood signs of circulatory disturbances (excessive collection of tissue exudation in the interstices of the subepithelial connective tissue, or a grouping of red blood cells in these interstices), or evidences of a throwing off of tissue into the uterine lumen, are noted. Only such areas are selected as are normal and whose tension, dependent on tissue sap, is even, which fact coincides with the observation that the uterine lumen at the selected point always shows a surprisingly smooth epithelial lining without folds.
The ovum is almost always embedded on the anti-mesometral side, corresponding to the fundus uteri in the human being, and beings about 6 days, 8 to 12 hours post coitus, seldom later at the end of the seventh day. The time left for embedding is 4 to 8 hours. Its beginning is known with a possible variation of about 6 hours. The ovum does not increase in size before its embedding, and measures with the zona only 0.1 millimetre, without the zona 0.08 millimetre, while the uterus is 6 centimetres long. As often only one or two ova are present and as their location is not macroscopically evident, only series sections divulge the various points. If the ovum is already through the uterine epithelium, it is seen with difficulty because of its small size. One may readily imagine the labor involved in obtaining the present unbroken series illustrative of the various stages, a work on which Spee has been engaged for the last ten years.
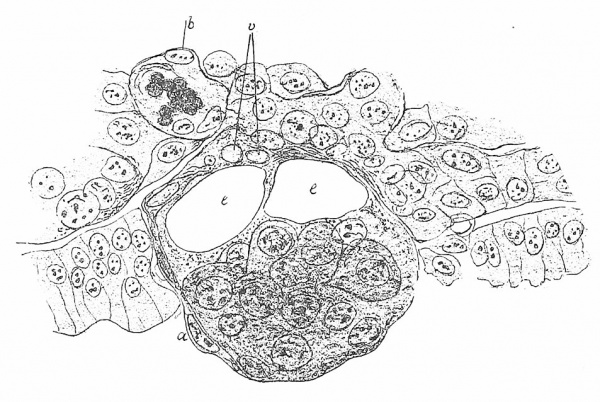
Fig. 4. b, capillary ; v, vacuole ; c, cavity in ovum. Ovum of guinea-pig par tially embedded, showing disappearance of the uterine epithelium, (v. Spee.)
The cells of that pole which leads all other parts in its entrance into the uterus (I. P.) send prolongations through the zona shortly before the implantation period, and render contact and exchange with the uterine epithelial cells possible, even before the zona is gone. These prolongations cause the first adhesion of the ovum to the uterine epithelium (Fig. 3a).
The uterus plays a passive role in implantation of the ovum. The ovum enters the uterine wall and a correspondingly large space of uterine tissue disappears.
The uterine epithelium shows no sign of growth.
The uterine epithelium of just that area in contact with the ovum disappears (Fig. 4).
In Fig. 4 the ovum is 6 days and 10 hours post coitus, and evidences no zona. A thin cell layer (a) surrounds for a distance the cavity (e) of the ovum on one side, but is not distinct on the other side. The solid portion of the ovum consists of large round cells which are not surrounded by a cell covering. Only at a is there a flat cell which stands in continuity with the cell membrane enclosing the cavity of the ovum (e). The membranous portion of the ovum contains two small vacuoles (v).
Fig. 5. Further stage in embedding of ovum, showing changes wrought in the connective tissue compacta. (v. Spee.) x, two cells of the ovum which are embedded on the opposite side.
The central cavity is lined with a non-celled coagulation substance, which has divided the cavity into two parts, probably a postmortem change. The external surface of the solid area is not covered by a specially differentiated layer of flat cells. The solid group of cells represents the placental pole. The cavity e represents the germinal cavity. The part of the ovum near the connective tissue, at the Implantation Pole, is the cell wall of the cavity, the germinal membrane. The space between the cells, and the thin layer near the connective tissue, later becomes filled with cells, forming a solid ovum.
Decided changes occur in the connective tissue which makes room for the ovum. These changes for a long time are such as may be considered a necrosis and a paralysis of the life processes of the connective-tissue cells (Fig. 5).
Fig. 5 shows a double embedding at two points vis-a-vis. The ovum evidences no cavity. The ovum is already deep in the wall and the uterine epithelium is interrupted in the circumference of the ovum. The surrounding connective-tissue cells have changed in that a half -moon arranged row of connective-tissue cells of a stronger stain has been formed. The cells of the ovum are much larger than the connective-tissue cells. To the left at x two cells of the ovum are united to the uterine epithelium, and two others, not distinctly seen, have perforated the uterine epithelium. The single layer about the ovum at I. P. is the germinal layer plus the implantation pole. The cell group at the placental pole has grown into, and filled out, the germinal vesicle, but the ovum is not enlarged. Therefore the ovum now evidences no cavity. The sharp contour at o bounds the connective tissue sharply and is independent of the cell body of the ovum. That the cells of the ovum dissolve the epithelium with which they come in contact, is seen in its early stages at x, where four cells are present. The connective-tissue cells about the ovum are large and polygonal with sharp contours and of epithelioid form. This form also is found in certain areas away from the ovum, and is there dependent on other influences than the ovum. This change in the cells extends, and this area is called the Implantation Area. During this peripheral extension the cells nearest to the ovum show other changes in the nuclei. They stain darker. This is due to a process of dissolution, and as a matter of fact the nuclei nearest to the ovum are already smaller and mitosis ha3 ceased in the immediate circumference of the ovum.
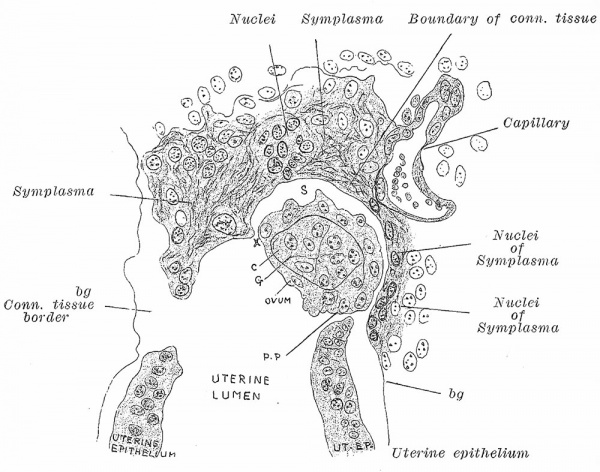
Fig. 6. Further stage of embedding of guinea-pig's ovum, showing the connective tissue compacta about the ovum destroyed by the bio-chemical influence of the ovum. (v. Spee.) c, centre of ovum ; G, embryonal sphere.
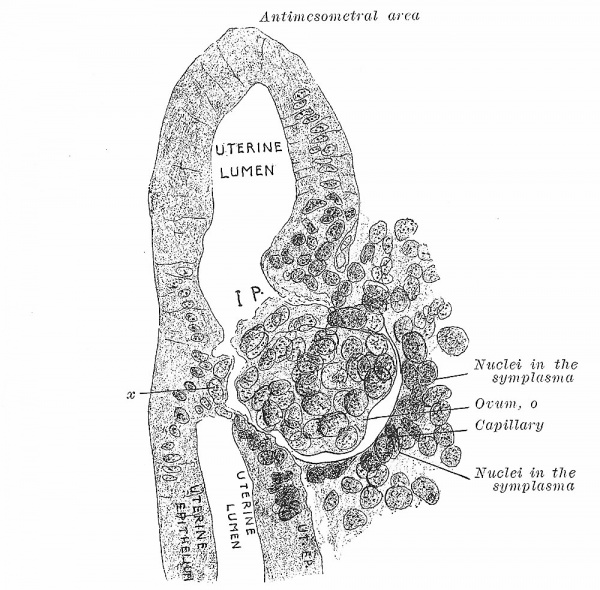
Fig. 7. A stage of embedding one-half hour later than Fig. 6 (v. Spee). more highly magnified. G, embryonal sphere. The ovum is surrounded by a symplasmatic zone.
The connective-tissue cells are fluidified by a form of digestion. The disappearance of mitosis for a considerable distance about the ovum, the dissolving of the connective-tissue cells immediately about the ovum, while at a distance normal cell division takes place, show that the destruction of uterine tissue is due to a biochemical process dependent on the ovum (Fig. 6).
Fig. 6 is still further embedded, and in four-fifths of its circumference is a single layer of cells, the germinal layer. This is connected at the placental pole with a solid mass, the germinal prominence, which fills the space surrounded by the germinal layer. The Implantation Pole is situated on either side of 8.
In Fig. 7 the ovum is situated half in the epithelium and half in the subepithelial connective tissue. The ovum is sharply bounded from the connective tissue. It is surrounded by a symr plasmatic zone in which a histolytic process causes the contours and nuclei of the connective-tissue cells to disappear, as if the ovum were a poison. The ovum consists of a covering layer and a contained mass (G) of large cells containing fat. A small space separates the ovum, in part, from the connective tissue (C. t).
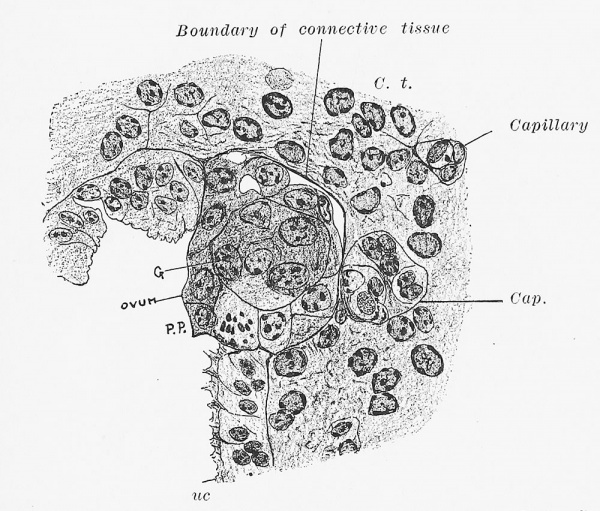
Fig. 8. Almost embedded ovum surrounded by fluid resulting from fluidified connective tissue cells, (v. Spee. )
The ova 6, 7, and 8, though differing only about half an hour in age, produce great changes in the connective tissue. Ovum No. 6 is about three-fourths embedded. Ova 7 and 8 were found in the same uterus. Only in 8 is a growth of the ovum, as compared with 5, evident. Important are the connective-tissue changes, first in the cells of the Implantation Area, and, second, in the boundary line which faces the ovum. Ovum No. 8 is almost embedded and several of its cells are on a line with the uterine epithelium. A comparison of ova 6 and 8 evidences two differences, which show the two varying functions in two different parts of the ovum, (1) the part consisting of the external layer, a derivative of the germinal layer, and the Implantation Pole; (2) the cell mass at the Placental Pole. In the circumference of the Implantation Pole the connective-tissue cells beneath the epithelium disappear or degenerate. The cells at the Placental Pole do not destroy the uterine tissue, therefore the hole in the uterine epithelium at the Placental Pole of ovum 8 is not enlarged.
Fig. 9. Ovum entirely under the uterine epithelium, a.s., assimilation border of the implantation area ; y, embryonal sphere ; H, fluid space about ovum, (v. Spee.)
In the Implantation Area the connective-tissue cells and the nuclei become large. The chromatin of the nuclei becomes grouped on the inner surface of the nuclear membrane, but the nuclear centre is pale. Peripheral to the implantation zone numerous mitoses are observed and are also found in the vessel endothelia. A dense tissue results and the cell interstices disappear, as may be seen in Pig. 9. This very peripheral area has no meaning with regard to implantation or to placental formation.
In Fig. 5 the cells nearest the ovum stain darker and are smaller. In Fig. 6 a contour divides the connective tissue near the ovum from the ovum, but instead of numerous cells and nuclei we see a fibred, granular mass, a group of closely gathered nuclei without cell contours. In Fig. 7 some nuclei are still well stained, but lie in a fibred, granular mass in which no cell contours are evident. A symplasma has been formed through the dissolution of the connective-tissue cells of the implantation zone which is sharply marked off from the ovum.
The ovum is then almost surrounded by fluid residting from these changed cells (Figs. 8, 9, 10).
In Fig. 8 the symplasma is separated from the ovum by the space H, which is wider than in Fig. 7. In the periphery are smaller, darker cells ready to join the symplasma. Here, then, is the assimilation boundary of the symplasma, The space H is filled with a fluid into which the edge of the symplasma passes over gradually. This constitutes the dissolution boundary of the symplasma. The contents of the space H are a thin emulsion which is under pressure, causing the circular contour of the symplasma in Fig. 9.
Fig. 10. A further stage, showing demarkation of the symplasma, thus limiting the assimilation of future areas, n, free nuclei in the symplasma. (v Spee.)
The fluidifying of the symplasma occurs not only at its edge but in its substance, and becomes porous and filled with vacuoles which contain fluid (Figs. 8 and 9). In Fig. 9 the vacuoles are present in large number. At the assimilation boundary at a. s. are seen darker, smaller cells. At / (Fig. 10) is seen a sharp demarkation of the symplasma of the implantation zone which limits the assimilation of future areas. The nuclei of the last assimilated cells lie at this area of separation, in short simple rows. They furnish almost -the same picture as the nuclei in the syncytial or plasmodial formations in the placenta of other animals. The symplasma degenerates and the original boundary of H formed by it disappears.
Fig. 11. Ovum entirely embedded in connective tissue compacta, showing spaces (H) in the fibred tissue about the ovum. The fibred tissue about the ovum contains numerous granules. This is a middle stage between the normal compacta and the final fluid symplasma. (v. Spee.)
Along the epithelial lining the subepithelial cells become smaller, and darker areas of separation appear between them and the epithelium leading up to complete loosening of the latter. The subepithelial cells, fluidifying, form lacunae in the subepithelial connective tissue (Fig. 12).
This fluid, through diffusion or possible absorption by the ovum, makes place for the ovum, which only now begins to grow quickly. Later, at the boundary between necrotic and healthy tissue, a real granulation tissue is formed as an active reaction to the entering ovum (Fig. 12).
In the transition zone appear granular cells, which increase from Fig. 9 on, and eventually forming a characteristic zone in the far periphery, in which the cells also seem clouded. Soon a separation of the implantation area from the connective tissue occurs at the transition zone through great growth of cells in the peripheral areas, and through a stoppage of growth and degeneration in the implantation area. The capillaries pass through this boundary and on their walls are grouped connective-tissue cells. They are numerous at the point of separation, so that the wall looks like a granulating wound surface of endothelial channels. The space about the ovum is gradually rilled with granulation tissue in the next twelve hours. Seven days post coitus the ovum has groAvn considerably (Fig. 12). The Placental Pole evidences a papulation of the germinal layer which gives this end a half-cylindrical groove, due to two lateral folds. The ovum now evidences a cavity, except at the Implantation Pole, where the embryonal sphere is in close contact with the external membrane of the ovum.
Fig. 12. g, embryonal sphere ; n, free nuclei of the syrnplasina ; b.c, capillaries. The ovum has grown. Ovum has a cavity, except at implantation pole, where the embryonal sphere is in contact with the external layer of the ovum, (v. Spee.) Completely embedded, growing ovum.
Seven days thirteen and one-half hours post coitus the ovum has grown large (Fig. 13). The space between the embryonal sphere and the Placental Pole has grown decidedly, so that the ovum is a long, cylindrical vesicle, with its Placental Pole in contact with the uterine epithelium.
The investigations of Spee show that the ovum, of the guineapig, not grown since its fecundation, destroys like an injurious parasite the uterine epithelium and the subepithelial connective tissue to make place for itself in the uterine wall in which it is embedded, and that only after this does it enter into a symbiotic connection with the uterus, which connection finds its expression in the formation of a placenta. The same occurs with the human ovum.
Chapter III. The Embedding of the Human Ovum
A. The Uterus
For many years it had been taught that the human ovum in the uterus developed on the mucosa (decidua serotina) and was enveloped by mucosa growing up about it (decidua reflexa).
Fig. 13. Cavity in ovum between embryonal sphere and placental pole has grown greatly, g, embryonal sphere. (v. Spee.) Rapidly growing, embedded guinea-pig ovum.
In the examination of young human ova Spee was never able to find uterine epithelium lining the bed in which the ovum rested, and he doubted the theory that the uterine mucosa and its epithelium grew up and surrounded the ovum. Hensen had made the observation that the ovum of the guinea-pig, on the seventh day post coitus, was no longer to be found free within the uterus, and that on the eighth day it was located in the uterine wall underneath the epithelial lining (Fig. 13). Selenka, on the other hand, supported the view that the ovum of the guineapig entered into a uterine gland whose epithelium was later destroyed.
The relation between ovum and uterus varies in different animals. There are forms in which the uterine epithelium is preserved at the point at which the ovum is attached. In all those cases in which the ovum grows before its attachment, it remains during its entire development within the lumen of the uterus or in a portion of the same. The closer relation between ovum and uterine wall develops later. In the case of ova which do not grow at that stage, the epithelium disappears. The smaller the ovum, and the smaller the area of uterine wall necessary for its attachment, the more intensely is the uterine tissue affected by the ovum, so that the area affected at this point becomes rapidly very large in proportion to the size of the ovum, and naturally the development of close connection between ovum and uterus occurs earlier than in the first class. Early attachment and small ovum are therefore favorable to the nourishment of the latter. A most favorable feature for the ovum is the form in which the fecundated germinal vesicle, without any increase in growth, is completely embedded in the subepithelial connective tissue of the uterus. Such is the case with ova of the rat, mouse, guinea-pig, and human being.
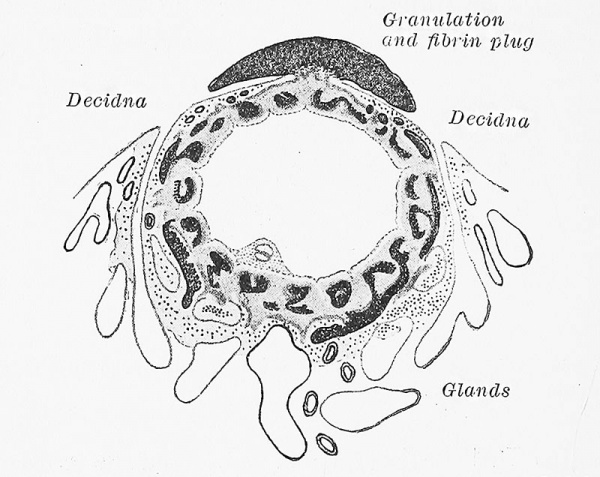
Decidua Menstrualis. — In the menstrual decidua the superficial capillaries become greatly dilated, and serous infiltration of the endometrium takes place, which separates the meshes of the stroma, accompanied by a gradual but decided dilatation of all the blood vessels and lymph channels. There occur a growth of round cells in the inter glandular tissue and an entrance of leucocytes into the mucous membrane. The glands become larger and wider, being often filled with secretion (Fig. 14).
This swelling of the mucous membrane, the dilatation of the blood vessels, the production of round cells, and the growth of the superficial layer of the endometrium produce the so-called decidua menstrualis. Although in the connective tissue large cells, not to be distinguished from young stages of decidua cells, are found, it is to be noted that typical decidua cells do not, as a rule, develop at this time in the superficial layer. These round cells are the beginnings of the decidua cells. The endometrium is at this period from 6 to 7 millimetres in thickness.
Decidua Graviditatis in the First Week. — On the occurrence of pregnancy, as will be noted below, the superficial portion of the mucosa is later composed mainly of cells and is called the compacta. The deeper layer is composed mainly of glands and is called spongiosa. In the first week, however, as may be seen from the description of Peters, there is a decided division into compacts, and spongiosa only near the ovum. There is at this time no real decidua elsewhere and no difference exists between the connective-tissue cells of the superficial and deep layers. The tissue between the glands, however, is thicker toward the surface. We find spindle-shaped connective-tissue cells mainly. The spaces between the cells are filled with a pale homogeneous plasma, and the tissue looks like reticular embryonal connective tissue. The nuclei in the more superficial cells are somewhat larger, and numerous small round cells are present which represent the early stages of decidua cells. The epithelium of the superficial glands and of the uterine surface is somewhat flattened. An hypertrophy of the glands, especially in the deeper layers, is present, and in transverse section they are lined with papillary projections on which are long, high, cylindrical cells, often looking like beaker cells. Numerous epithelia are found free in the glands. These glandular changes are marked mainly near the ovum.
Fig. 14. Menstrual decidua. a, section through vessels surrounded by groups of round cells ; h. interglandular tissue consisting of normal cells with scattered round cells ; d, section of a gland somewhat dilated — its epithelia are somewhat smaller than normal. (Abel.)
Fig. 14a. Decidua in intrauterine pregnancy (abortion) at the second month {curetting), a, section of a gland with flattened epithelia : b, interstitial tissue consisting of the so-called decidua cells, between which at certain points irregularly-scattered round cells are seen ; c, section of a vessel — in the wall are endothelia. (Abel.)
Decidua Graviditatis. — These typical changes occur, chronologically, at a later period in the entire uterus. Since, however, they are marked in the first two weeks immediately about the ovum, they are mentioned now. It is especially necessary to consider the base in which the ovum develops, as it is difficult at all times, even as early as the first week, to distinguish in many areas between fetal and maternal cells. The mucosa of the pregnant uterus, at its thickest, increases to ten times its original depth by the growth of all its elements. At the end of the first month it is one centimetre thick. Its surface is uneven, deep grooves dividing into irregular fields. These changes are greatest at the fundus. In the region of the internal os the changes are less marked, the lining of the cervix, except for a high degree of hyperemia, having no part in these changes. The increase in the volume of the decidua depends greatly upon the growth of round cells in the endometrium and upon their change into decidua cells. The round cells of the connective tissue, situated in a meshwork of spindle- and star-shaped cells forming the stroma, enlarge. The protoplasm increases greatly in amount and the nucleus becomes larger. The cells are closely grouped, pale and epithelial in appearance (Fig. 14a). They are, like the connective-tissue cells of the normal uterus, infiltrated by capillaries and larger vessels whose endothelium borders immediately on the individual cells. The nuclei are round and long, 8 to 10 pi long and 10 to 12 ju wide. They stain lightly because their chromatin network is very fine. There are nucleoli. Mitosis is rarely observed, but two nuclei may be present. They generally retain their spindle-shaped form or are round polygonal. There is often a fine space between the individual cells, filled with a homogeneous intercellular substance. These cells appear at first in the upper layer, and so prominently that this layer of the gravid decichia is called the compacta. Later, as a result of pressure, the cells resemble squamous epithelium.
Fig. 14b. A gland in the decidua graviditatis, showing the erroneously named "syncytial change" of the lining epithelium. Taken from the curetted mucosa of a uterus two weeks gravid.
The external layer near the muscle contains so many gland lumina that the interglandular tissue is in the background. This interglandular tissue disappears more and more, so that finally a tissue honeycombed by glands results. This layer, in contrast to the superficial, is known as the spongiosa. The compacta is thrown off with the ovum; the spongiosa remains to regenerate the glands.
The gland cells lose their cylindrical form and become cubical and spherical. The protoplasm grows and the nuclei are therefore further apart. Into the gland extend prominences covered with groups of epithelium (Fig. 145). Sometimes the cell boundaries become indistinct, giving the so-called "syncytial change, which has nothing to do, however, with real syncytium.
Fig. 15. Schematic representation of the earliest stage in the embedding of the human ovum. (Peters.)
The epithelium of the surface is subjected to pressure and is flattened, becoming later thin as endothelium.
B. The Embedding of the Human Ovum
Spee and von Herff have shown that in the guinea-pig the ovum forms an opening through the epithelial lining of the uterus, and that, after having passed entirely through the mucous membrane, it develops further in the region of the subepithelial connective tissue. The opening thus formed is closed by lymph exudation, and there results about the ovum a so-called lymph space, showing that an exchange between the ovum and the surrounding tissue exerts upon the latter a certain reaction. That the same process of centrifugal descent of the ovum into its bed occurs in the human being is to be expected, for the following reasons: 1. By analogy with the above process. 2. In human beings there is no epithelium, nor are there any gland openings on the surface of the so-called reflexa, facing the ovum. 3. The youngest human ova found in the uterus show no prominence into the uterine cavity, which would be the case if they developed upon the decidua vera and were surrounded by a decidua reflexa.
Ovum in the Earliest Stages. — Peters examined a growingovum supposedly three clays old. The uterus was slightly enlarged and soft. The decidua at the fundus and on the posterior wall was 8 millimetres thick ; on the anterior, 5 millimetres. The lining of the cervix was hyperemia. On the posterior wall was a slight prominence, which proved to be the ovum, whose largest diameter was found to be 1.6 millimetres. The ovum was embedded in the compact part of the decidua, which portion, as before stated, showed only a slight prominence. The summit of the ovum was not covered by a capsule, but showed a spot of blood granulation.
Fig. 16. Schematic representation of a centrifugally embedded human ovum. (Peters.) The summit of the capsularis is closed by a fibrin plug.
Only in the immediate circumference of the ovum was there a clear division into compacta and spongiosa. The nearer to the ovum, the more frequently were free red and white blood cells found between the cells of the stroma and in the plasma. Nowhere was there an evidence of fatty changes in the superficial layers. The mucosa was everywhere extremely vascular. The venous channels showed, superficially, often only a simple canal of thin endothelium, without adventitia. The arteries preserved their adventitia up to the covering epithelium. The nearer to the ovum, the greater was the vascularization. In this case fecundation took place shortly before the expected menstrual period. The fact that this ovum had made its way into the decidua, wherein it was firmly embedded, proves, analogous to the observation of Spee, that an ovum can develop only on a spot free of epithelium, and that, through reaction upon the surrounding tissue, an ovum sinks into the decidua, and that this reaction causes a dilatation of the surrounding lymph spaces, with a resulting localized edema (Fig. 20).
In the edges of the groove in which the ovum was embedded, and also deeper clown, a more decided hemorrhagic edema took place and minute blood extravasations forced their way up to the epithelium and lifted it off. The resulting coagulation, containing likewise the remains of these cells, serves to close the opening and to cover the ovum (Fig. 16).
Capsularis. — In place of the old view of a reflexa growing up and above the ovum supposedly situated on the epithelium lining the uterus, a centrifugal descent of the ovum must be taken for granted. In v. Spee's young ovum the capsularis had not yet united at the summit. In Leopold's case (ovum seven to eight days) union had already occurred. In Peters' case the summit was closed by fibrin. Leopold and almost all investigators find the structure at this point atypical. The same changes are found as Sanger remarked in the organization of hematocele capsules, i.e., fibrin, connective tissue, and capillaries. Keibel, Kollman, and Reichert say that at the summit of the capsule union results in the formation of what may be called a cicatrix, to which is given the name cicatrix of Reichert.
As proof of the ready and early connection between maternal blood and fetal tissues, it may be mentioned that the tissue which separates the capillaries from the uterine epithelium becomes extremely thin in the decidua menstrualis. The capillaries which run a twisted course between the glands of the spongy layer extend up to the epithelium under the mucosa. In the compacta or superficial layer they often possess only an endothelial wall. When the ovum sinks into the decidua the decidua basalis presents in addition a huge dilatation of the capillaries. The zone which surrounds the ovum is formed by the compacta. As the ovum descends, gradually more compacta surrounds it, forming the so-called enveloping zone.
The Enveloping Zone is the layer of the compacta immediately about the ovum. It furnishes the blood supply to the growing blastocyst. Through its edematous infiltration it renders the centrifugal descent of the ovum easy.
Chapter IV. The Early Development of the Human
OVUM.
The early cell division taking place in an ovum is a more or less even increase, which later gives way to a development along specific lines in certain and well-distinguished areas, so that larger or smaller cell complexes pass through varying phases leading ultimately to the production of embryonal and extraembryonal structures. Preliminary to this stage the cells' of the ovum, which lie loosely together in the earliest period of cell division, become more closely united, so that an epithelium is formed. The epithelial membranes resulting from this early cell division are called germinal layers (Fig. 17). It is in them that the various specific areas of development subsequently appear. On the two germinal layers (ectoderm and entoderm) lining the germinal vesicle or ovum and on the subsequent complexes of these layers, two surfaces are to be distinguished: (1) An inner surface or base facing the cavity of the ovum, and (2) an external or free surface. The various cells of a germinal layer may increase or advance in either direction. If the cells advance from the basal side this constitutes an invagination; if from the free surface, an outgrowth or papulation.
File:Bandler1983 fig17.jpgFile:Bandler1983 fig17a.jpg
Fig. 17. Scheme of ovum at stage of simple chorion ectoderm and entoderm. Fig. 17a. A, amnion. Scheme of ovum with formation of amnion from the ectoderm.
The germinal vesicle increases in size through an increase of fluid in its centre, and is composed of two original boundary layers lying together: an outer, the chorion ectoderm, and an inner, lining the cavity, the entoderm. This combination is called the germinal vesicle and probably represents the stage immediately after embedding. At a certain point is an oval area, the area embryonalis, in which appears an additional very small cavity, the amniotic cavity, in the wall of which the embryo first appears. The exact mode of this production cannot be positively stated, but it follows one or two closely allied forms. It may be formed through an invagination of the ectoderm (Fig. 17a), the folds in the area of invagination lying close together and uniting quickly, thus leaving within the ectoderm a small enclosed cavity. The very smallest amniotic cavities (flying-dog, guinea-pig) are formed by a solid group of cells passing out from the ectoderm and finally becoming separated from it. In the
centre of this solid group the subsequent amniotic cavity develops (Fig. 17b).
File:Bandler1983 fig17b.jpgFile:Bandler1983 fig17c.jpg
Fig. 17b. Ovum with ectodermal amnion separated from the chorion ectoderm. A, amnion.
Fig. 17c. Ovum with ectoderm, entoderm, amnion, germinal plate, but no mesoderm. (Schematic.)
The early amniotic cavity of the human ovum is extremely small. In no animals where an amniotic cavity is formed through the production of reflected and approaching germinal folds does such a small amniotic cavity result. Therefore the amniotic cavity of the human ovum follows either of the two aforementioned processes. By either of these two methods, then, an amniotic cavity passes out from the ectoderm and pushes the entoderm toward the central space of the germinal vesicle. (It is possible that the amnion develops in the embryonal sphere of Fig. 13. We know little about the origin of the entodermal space, and it is described as the lining of the germinal vesicle, although it is possible that it develops in a manner resembling the amniotic cavity.) In the human ovum, in all probability, the early stage consists of small ectodermal amniotic cavity sunk into a depression in the closed yolk vesicle lined with entoderm, these being surrounded by the single layered ectoblast vesicle, the later chorionic ectoderm (Fig. 17c). At this stage no mesoderm is present.
On a portion of the ectodermal lining of the amniotic cavity appears an area, the primitive streak. The cells about it become differentiated into the ectodermal germinal plate (the future embryo). In the primitive streak is a furrow — the primitive furrow — which lies, therefore, in the middle of the later germinal plate. By a growth of cells of the germinal plate on either side and over the primitive furrow (primitive medullary plates) a canal results — the medullary canal (Fig. 30a).
File:Bandler1983 fig18.jpgFile:Bandler1983 fig18a.jpg
Fig. 18. Ovum showing the beginning of a mesodermal growth at the caudal end of the germinal plate. (Schematic.)
Fig. 18a. Ovum with completed growth of mesoderm. (Schematic.)
There begins, with the appearance of the amniotic cavity and the differentiation of a portion of its lining into the ectodermal germinal plate, the development of mesoderm at the caudal end of the latter (Fig. 18). This growth of mesoderm begins close to the inner surface of the chorion ectoderm and forms (1) a thick mesodermal mass, the caudal knot of the primitive streak, extending about the caudal side of the amnion up to the chorion (Fig. 18) ; (2) thin mesodermal layers which grow between the chorion ectoderm and the ectodermal amniotic cavity, and the entodermal yolk vesicle.
In the schematic drawings the entodermal yolk vesicle has been drawn large to make the relations clear. Whatever its size may have been at the beginning, and whether it originates as a very small vesicle in an embryonal nodule or not, it is certain that on growth of the mesoderm the amniotic and yolk cavities are found in the embryonal area of the ovum and take up a relatively small portion of it.
Fig. 19. A part of the periphery of the ovum of Peters, showing actual conditions pictured schematically in Fig. 18a. Yolk sac is very small compared with Fig. 18a,, and naturally the amount of mesoderm below the germinal plate and the yolk sac is much larger than in Fig. 18a. Fig. 19 is the E.F. of Fig. 20.
The ectoderm of the ovum develops hugely, forming the chorionic ectodermal cover or trophoolast.
This stage is well represented in the embryonal formation of Peters (Fig. 19). The ovum is surrounded by chorion ectoblast formation. Cells are more plentiful in the mesoderm near the chorion, but the mesoderm is thick only in the region of the embryonal formation. The internal part of the oval cavity is poor in cells, between which is a weakly staining, fibred, granular mass. The embryonal formation consists of two small epithelial cavities, the ectodermal amniotic and the entoderm yolk vesicle surrounded by mesoderm and embedded in a thickening of the mesoblast near the chorion. The amniotic cavity is entirely closed. Its wall is differentiated into the very thin amniotic membrane and into the germinal plate, composed of high cylindrical cells. Between these and the entoderm cells of the yolk, the future umbilical vesicle, is a layer of mesoderm cells, which are separated from the ectoblast area of the amnion by a membrana prima which always develops at the border between ectoderm and mesoderm.
DIVISION INTO EMBRYONAL AND EXTRA-EMBRYONAL AREAS.
Through the appearance of a slit in the entire circumference of the mesoderm beginning at the caudal end of the germinal plate, but not dividing the dense mass of mesoderm at the caudal end, the amnion with its germinal plate and the future umbilical vesicle are separated from the chorion ectoderm up to the dense mass of mesoderm, which then constitutes the point of union between the embryonal formation and the chorion ectoderm. This point of union contains the adherent band (future abdominal pedicle) and the caudal knot of the primitive streak (Fig. 19a).
Fig. 19a. — Ovum, Fig. 18a, after the development of the mesodermal periembryonal slit. (Schematic.) The adherent band of mesoderm connects the embryonal and extra-embryonal divisions.
The amnion and embryo develop from a small area in the germinal covering, and with the umbilical vesicle are separated from the extra-embryonal area of the ovum, with which they are connected through the adherent band of mesoderm alone. The embryo develops from a portion of the ectodermal lining of the amnion.
The extra-embryonal area of the ovum forms the troplioblast, villi, the chorionic membrane, and the placenta.
Chapter V. The Tbophoblast in the Ova of Animals
THE EARLIEST DEVELOPMENT OF THE ECTODERMAL EXTRA-EMBRYONAL AREA OF ANIMAL OVA.
In discussing the histology of gestation it is important to note that in this field, as well as in that of embryology, many of the most important and valuable points have been learned through the study of like processes in animals. The results obtained in investigations in the latter have been applied more or less closely to the various developmental changes in the human being. Though ofttimes erroneously applied, they have been the source through which many vexed questions have been settled. More recent investigations, however, prove that it is not so much the erroneous applications of the results gained in the study of animals as it is errors made in these observations which have so long delayed a satisfactory conclusion concerning the various processes involved in human placentation. It is necessary, for that reason, to consider first the more recent studies concerning animal placentation, as reviewed by Strahl.
Marchand examined the placentas of rabbits gravid from eight to sixteen days. In the earliest specimens he finds on the ovum a growth of ectoderm elements consisting of two layers: (1) a deeper layer of separated cells and (2) a superficial plasmodial. Since the latter is still covered in part by the zona, it is necessarily of fetal origin. In addition he observes transitions from the cell layer of the ectoderm into the plasmodial. The deeper cells become larger and are arranged in groups. Their cell boundaries disappear, and, through a union of these cells, a plasmodial layer is formed, covering the deeper ectoderm, but, as a rule, distinctly outlined from it. This ectodermal Plasmodium unites with the syncytially-changed uterine epithelium, forming the first connection between the ovum and the uterine wall. In the placenta of nine to ten days Marchand finds blood (1) in the maternal vessels possessing an endothelial lining and (2) in ectodermal spaces in the cell layer. Into these spaces, which possess no endothelium, the blood from the maternal vessels enters.
In the placenta of eleven days few of these unlined ectodermal spaces containing blood remain. Most of them are now lined with a continuous layer of elements rich in protoplasm, which Marchand considers originate from the maternal vessel endothelium ( ?), which has undergone a "syncytial change."
Maximow, in his investigations on rabbit placentae, denies, in contrast to Marchand, the existence of a fetal ectodermal Plasmodium as early as the eighth day. He believes that, when the ovum attaches itself to the uterine wall, the ectoderm consists of only separated cells, which come in contact with the epithelium of the uterus and cause it to degenerate. When the ectoderm, after disappearance of the uterine epithelium, reaches the maternal vessels, the glycogen-containing cells of the uterine connective tissue change to large polynuclear structures. In these cells he finds elements resembling red blood cells in form and color. Only later, when the ectoderm enters into the decidua, does it divide into two layers: (1) one with cell boundaries, the cytoblast, and (2) one without cell boundaries, the plasmodiblast. The latter is found only where the villi come in contact with the glycogen-containing cells, at the ivalls of the maternal vessels. It is not found where the villi grow into the connective tissue between the vessels. From the tenth day on, spaces filled with maternal blood are found in the fetal Plasmodium and there develops an ecto-placenta, into ivhose ectodermal villous formations the mesodermal elements bringing the allantoic vessels enter.
Opitz finds in the rabbit a double ectodermal layer during the process of attachment of the ovum in the uterine wall: (1) an internal layer formed of separated cells, and (2) an external plasmodial layer. The latter causes the uterine syncytium to disappear and aids the attachment of the ovum to the uterine wall freed of epithelium. In the Plasmodium spaces occur into which maternal blood empties from the eroded maternal vessels. From the ovum, ectodermal cell groups enter into this ectodermal Plasmodium, are vascularized, and later become also plasmodial. Those syncytial cells which Marchand considers as resulting from maternal endothelium, Maximow, however, views as ectodermal Plasmodium when found in the fetal portion of the vessels, but considers them in the maternal portion to be endothelial. Opitz considers these cells to be entirely of ectodermal origin. It is to be noted that Maximow and Opitz mention the destruction of the uterine epithelium. Later fetal mesoderm with the allantoic vessels enters into the placenta and on its external surface the remnants of the ectoderm are found as flat covering cells. The epithelium of the uterus plays no part in the development of the placenta, but forms a syncytium which is absorbed by the ectoderm cells.
In Tarsius, Hubrecht finds that the uterine wall, through a change of the connective tissue, forms a trophospongia, betiveen ivhich the glands degenerate. On the growth of the embryonal ectoderm or trophoblast, a mixture of trophoblast and trophospongia occurs, with a decided increase in the volume of this early placental formation. Then the development of the mesodermal villous elements takes place, and the mesoderm villi surround themselves with a trophoblast covering. Between the trophoblast cells lacunae form, into which maternal blood passes. Finally, the trophospongia becomes a thin layer which represents the boundary toward the deeper maternal tissue.
In Tupaja, when the ovum rests upon the uterine wall its ectoderm causes the uterine epithelium to disappear. The trophoblast grows decidedly, with the formation of giant cells, and occasionally forms a combined layer with the uterine epithelium in which maternal and embryonal nuclei lie in a common Plasmodium. The maternal portions degenerate, but the ectodermal tissue is divided into ( 1 ) a deeper layer, the cytotrophoblast, and (2) a superficial syncytial layer, the plasmoditrophoblast, which constitutes only a temporary differentiation. In the uterine wall, in the meantime, the connective-tissue trophospongia is formed; the border between ectoderm and maternal connective tissue disappears, for these tissues infiltrate each other. In this resulting union the trophospongia is overcome by the trophoblast and the maternal blood passes from the maternal capillaries into the embryonal trophoblast spaces. The mesodermal fetal cells, then enter with the allantoic vessels and receive on their external surface a covering of trophoblast.
Although various investigations have shown that the variations in the development of the placenta in different animals are quite unexpected, and that among the individual mammalia, even when closely related, decided differences are found, yet the trend is more toward the view that, as a rule, the syncytium originates from fetal ectoderm. According to Strahl and Selenka, in quite a group of placenta? the uterine epithelium plays no unimportant role. On the other hand, Frankel, as a result of extensive investigations, comes to the conclusion that the higher the organization of the placenta and the more firm the connection between maternal and fetal tissues, so much the less is the maternal epithelium preserved.
He finds that in the rodents and in the insectivorae, whose placentae, of all the animals he examined, stand nearest to the human placenta, the uterine epithelium ceases at the border of the placenta. Only in the pig does it remain. In the cow and sheep the epithelium in the cotyledo shows a tendency to degeneration. In the cat, rabbit, squirrel, guinea-pig, rat, mouse, and mole the uterine epithelium takes no part in the formation of the placenta. A so-called syncytial formation, however, he finds to occur in the most varying tissues. The higher in the animal plane the animal stands, the more does the chorionic epithelium groiv into the maternal connective tissue robbed of its epithelium.
Opitz finds that in the guinea-pig the foundation for the placenta is the fetal ectodermal plasmodium vascularized by maternal vessels. The placentae of the rabbit, the guinea-pig, and the human being agree in that earlier or later the ectodermal surface of the ovum comes in contact with the connective tissue of the uterine mucosa. Finally, between maternal blood and the fetal vessels found in the mesoderm of the villi only one layer of the ectodermal syncytium is left. The apparently great differences are to be explained by the fact that in the rabbit and guinea-pig the projections of ectoderm and mesoderm (the villi) come into union with each other, while in the human being they are always separated.
Chapter VI. The Trophoblast of the Human Ovum
THE EARLY DEVELOPMENT OP THE ECTODERMAL EXTRA-EMBRYONAL AREA.
Trophoblast. — The outer layer of the ovum consists of trophoblast. It is a product of the ectoderm and from it develop the future syncytium and, according to most authors, the cells of Langhans. The "trophoblast," according to Hubrecht, "is the epiblast of the blastocyst, as far as it has a direct nutritive significance as indicated by proliferating processes, by immediate contact with maternal tissues, maternal blood, or secreted material." It consists of small and large cells of various forms. Shortly after the ovum descends into the mucosa a connection between the trophoblast and the maternal blood takes place. As all the capillaries near the trophoblast consist of endothelium and evidence many blood sinuses, the trophoblast is infiltrated with blood lacunas which are separated from each other by these trophoblast cell groups. As a result of the growth of these cells, of congestion and of pressure, the blood takes its exit from the capillaries and bathes the cells. The lacunas, then, represent a united system fed by peripheral capillaries and are separated externally from the decidua by a thin layer of ectodermal trophoblast cells, but the trophoblast at various points may extend much further into the compacta.
Fig. 20. Low-power drawing of the trophoblast, enveloping zone, etc., of an ovum three days old. in transverse section. (Peters.) Sy., syncytium; F.P., plug of fibrin at the summit of the capsularis ; Bl.L., blood lacunae; Tr., trophoblast ; M., mesoderm ; Cap., capillaries ; CI., glands ; E.Z., enveloping zone ; E.F., embryo formation ; Comp., compacta ; U.E., uterine epithelium ; GL, gland.
Fig. 21. Section through the central portion of the trophoblast layer. The trophoblast {Tr.) is covered with syncytium {Sy.) at all points in contact ivith the blood lacunae (Bl.L.). Ekt., ectoderm. (Peters.)
The ectoblast cells are of varying form: 1. Cubical, with large, strongly stained round or oval nucleus containing granules and nucleolus. 2. These become changed. The nucleus becomes pale and swollen. Vacuoles appear in the cells and strongly stained fragments of the nucleus are evident. The cells are irregular in form. 3. The nuclei are larger, especially in the external layers, and more swollen. The chromatin network is irregular and dark lumps appear in the nucleus. The nuclei are of various forms, oval, spindle-shaped, and contain vacuoles. 4. Swollen groups of nuclei in degeneration are found. These nuclei contain one or more nucleoli. 5. The protoplasm of these cells unites, forming protoplasmic masses in the shape of bands or irregular groups with extensions.
From the simple cubical cells of the central layer of the trophoblast we find, in going toward the periphery, gradual changes from 1 to 5. The trophoblast cells grow through direct cell division. These changes represent the results of the corrosive action of the Mood on these cells, whereby the future syncytium is formed. The syncytium then lines the lacunas (Fig. 22) . The endothelium of the lacunae and of the capillaries degenerates wherever it is not lined by syncytium. The syncytium is found also under the endothelium of the most peripheral trophoblast masses, and proves that the endothelium plays no part in tlie formation of the syncytium.
Pig. 22. A capillary (Cap.) in the serotinal portion of the trophoblast infiltrated with blood lacunae (Bl.L.). The peripheral wall of the capillary is preserved and forms the serotinal wall of the intervillous space at this point. The capillary at many points communicates with the lacunas (Bl.L.). In the capillary is a large mass of syncytium (Sy.) containing changed trophoblast nuclei (a) and red blood cells (6). At c changes in the trophoblast nuclei are evident. (Peters.) Tr., trophoblast; EM., ectoderm; M., mesoderm; CO., central cavity of ovum ; p. En., peripheral endothelium.
It is to be noted that the opening of the maternal vessels occurs at this early stage, before villi are formed. The endothelium of the capillaries degenerates and the blood makes its exit from the capillaries. It ought to coagulate, but does not. It circulates against the fetal cells, which have the power to prevent coagulation, and yet the blood exerts a deleterious influence on these cells. Thus the resulting syncytium lines the lacunae, prevents coagulation in this primary intervillous space and later about the villi, separating the blood at all times from the cells of the chorionic centre. Free syncytial cells are present, even in the vessels of the periphery in the compacta. At later periods they are found free in the veins and arteries. It is thus seen that the cells of the trophoblast of the ovum enter the veins at an early period.
Fig. 23. Change of trophoblast to syncytium (Sij.) The syncytially changed trophoblast is infiltrated with numerous vacuoles (vac), c, red blood cells of the capillary in which this syncytial mass was floating attached by a pedicle (p). (Peters.)
The Primary Intervillous Space is intravascular and is bounded by maternal and fetal structures. That the developed intervillous space contains free blood has been granted by Virchow, Kolliker, Langhans, Waldeyer, etc. The drawings of Peters indicate a slowing and probable stagnation of the blood current. The maternal endothelium on the side toward the compacta is at first intact and forms the serotinal wall of the space (Fig. 22). In it are found isolated cells and groups of trophoblast. Trophoblast cells are also present on the serotinal wall, so that this wall consists of trophoblast, maternal endothelium, and decidual tissue. Later the endothelium of the serotinal side is found only in the areas corresponding to the openings of the maternal vessels. Where the trophoblast cells extend into the enveloping zone in the form of bands, uniting with each other in a network, it is often difficult to distinguish between maternal and fetal cells. Merttens says the same. Thus the earliest ectoderm cells enter actively into the maternal tissues.
The primary intervillous space is formed through the gradual consumption of the trophoblast. Through its growth more and more layers of the compacta are included in the enveloping zone, until the corrosive action of the blood has furnished the villous mantle of the ovum. 1. The trophoblast is reduced to a single layer. 2. The union of the lacunas at first separated by large trophoblast cell masses takes place. The origin and growth of the intervillous space thus goes hand in hand with the various steps leading to the formation of villi. In the ovum of Peters no villi are yet present. The inner surface of the trophoblast shows irregular, finger-like depressions into which mesoderm is beginning to enter. The lacunas have enlarged and the cell masses between them have become smaller. Through the entrance of the growing mesoderm into these divided cell masses, which are finally reduced by the blood to the syncytial layer, villi are formed and the primary intervillous space becomes larger. The primary enveloping zone becomes the subsequent intervillous space.
Fig. 24. Schematic representation of the earliest stage of the development of the placenta. (Peters.) M., mesoderm; Tr., trophoblast; Bl.L., blood lacunae; Sy., syncytium ; En., endothelium ; Cap., capillary ; E.Z., enveloping zone ; Sp., spongiosa.
The maternal endothelium breaks down and is found floating in the lacunas. It is never seen in a proliferating stage. Syncytium is found under it. It is impossible for the endothelium to fill out all the spaces of the trophoblast, and, if it did do so, we ought to see it somewhere in the process of growth. On the contrary, it is always seen to degenerate. Therefore the syncytium does not originate from maternal endothelium.
The syncytium is found over the surface of the ovum, in the trophoblast, in the lacunae, toward the enveloping zone, and also in the periphery of the ectodermal trophoblast. At the summit of the ovum syncytium is also present. In numerous points the direct transition from trophoblast cells to syncytium is distinctly seen. Therefore it does not originate from the uterine epithelium.
The glands in the decidua about the ovum become filled with blood. They are pushed aside by the growing ovum and are broken into by the trophoblast and syncytium. Their epithelium degenerates and disappears. The uterine epithelium plays no part in the formation of the syncytium.
The syncytium consists of a shining, granular protoplasm containing numerous nuclei. The nuclei are round, oval, or flattened. There are also vacuoles in the protoplasm, which make the latter appear like septa in which are flat and half-moonshaped nuclei (Fig. 23).
Van Siegenbeck finds syncytial giant cells especially near the union between maternal and fetal tissues, in and about the lacuna?, between the ectoblast and the compacta, covering the free compacta, about the maternal capillaries, and even more externally in the vessels. He finds a gradual transition from trophoblast to syncytium. In one place he observed a syncytial giant cell between the mesoblast, and the ectoblast of the fetal sac, which he considers as a proof of the ability of these cells to wander into surrounding tissues.
The processes, so far, are well represented in the schematic drawing, Fig. 24.
Merttens found in the particles obtained by curetting sixteen days after the last menstruation a few sections of an ovum with the enveloping decidua. He describes (1) the chorion and the villi ; on the latter are cell groups, and between them are found spaces constituting the intervillous space; (2) the spongiosa, containing numerous glands, and (3) the compacta, a pale zone lying between 1 and 2, and containing large pale cells between which are numerous darkly-stained nuclei.
In the compacta he finds large cells and large spaces. Between the large cells syncytial masses are irregularly distributed. The cell spaces are round, long, or irregular, and often empty into the intervillous space. They contain blood and are all lined with syncytial masses, which at some points are very thin, and at other points quite thick. Where these spaces empty into the intervillous space the syncytial masses continue into the syncytium of the villi. Merttens does not know whether these spaces are glands, vessels, or lymph spaces. They are possibly, however, the lacunae ~of Hubrecht and Peters.
The epithelia of the glands are like beaker cells, and on their free tips is a half -moon of glycogen. The glands evidence papillary projections (compare Fig. 14ft). Merttens believes that the syncytium results through a change of the surface and gland epithelium ( ?). In his Fig. 8 Merttens represents, in the upper portion, the epithelium of such a gland, and the lower half represents syncytial masses. He believes that the latter results from these epithelial cells, which lose their cylindrical form and unite. From his description and his drawings it is neither clear nor probable that the epithelium goes over into these syncytial masses. Besides, this area is taken from decidua particles not connected with the ovum, and at no point can he find the epithelium of the glands contributing in any way to the syncytium of the chorion.
On the contrary, this ovum is at the stage where the trophoblast is almost consumed by the growth of the intervillous space, and the cell groups at the end of the villi, which Merttens calls points of union between the villi and the decidua, are really the remains of the trophoblast (Fig. 31).
Chapter VII. The Further Development of the Human Ovum
THE EARLY DEVELOPMENT OF THE EMBRYONAL AREA.
1. The ovum v. H., described by Spee, was thrown off after five weeks menopause. The ovum contains an oval germinal plate entirely in the stage of the primitive streak and situated in the wall of the amniotic cavity. The entire embryonal formation is 0.4 millimetre long. The greatest diameter of the ovum including the villi is 5% to 7 millimetres. Under the chorion was found a thin layer of connective tissue poor in cells and bounding directly the mesodermal slit. From this layer the chorion could be lifted off. The inner part of the ovum contained a bubble of air and a non-celled fibred coagulation substance in which, on the serotinal side, was seen the embryonal formation, which included the amniotic cavity with the germinal plate and the umbilical vesicle (Fig. 25).
Fig. 25. — Ovum v.H. (Spee), showing embryonal and extra-embryonal areas. The extra-embryonal villi and membrana chorii are connected with the embryonal formation by the adherent band of mesoderm.
The primitive streak region is small, and yet the development of mesoderm within the chorion, in the abdominal pedicle and about the amniotic cavity and about the umbilical vesicle, is so great that considerable time must have been needed for its development. At the time when the mesoderm began to develop, the ovum was probably of a diameter of 0.5 millimetre. At the first beginning of the mesoderm slit the ovum was probably of a diameter of 1 millimetre.
The embryonal formation is a long, thick projection connected at one end with the inner side of the chorion, but otherwise projecting free into the cavity of the vesicle, that is, the periembryonal mesoderm slit (Fig. 25). A superficial transverse furrow divides it into two elliptical parts. The larger is at the free end and contains the entoderm vesicle. The smaller part contains the amniotic cavity lined with ectoderm and consists, in addition, of the compact band of mesoderm which covers threefourths of the amnion, from the mesodermal covering of the entoderm vesicle up to the chorion (Fig. 26) . This compact band is the adherent pedicle and corresponds to the caudal end of the primitive streak. The entoderm vesicle sends a blind duct, lined with entoderm, into the adherent pedicle. The entoderm vesicle lined with a single row of cubical cells, and covered with mesoderm, is the umbilical vesicle. The amniotic cavity is lined with ectoderm and is likewise covered with mesoderm. The single layer of flat cells lining the amniotic cavity begins to thicken at a certain point ; the cells become high cylindrical and constitute the germinal plate. That part of the ectoderm of the amniotic cavity lying on the umbilical vesicle enters, then, into the formation of this thick germinal plate. The mesoderm which covers the umbilical vesicle and the amnion unites in the narrow zone which separates the two. Here where the walls of the umbilical vesicle and amnion run parallel, the germinal plate is found on the inner surface of the amniotic cavity. From the caudal knot up to the chorion extends the adherent pedicle, the future abdominal pedicle, and here the mesoderm lining the chorion and that found in the embryonal formation unite (Figs. 26, 27).
Fig. 26. Longitudinal section through Pig. 25, ovum v.H. of Spee. V.V., the future umbilical vesicle. The adherent band of mesoderm connects the embryonal formation with the extra-embryonal membrana chorii.
Fig. 27. Fig. 26 enlarged, showing actual conditions in the ovum v.H. pictured schematically in Pig. 19a. U.V., the future umbilical vesicle ; ENT., entoderm ; HES., mesoderm.
Fig. 28. Transverse section through germinal plate of Figs. 26 and 27 (Spee.)
Posterior to the caudal knot of the germinal plate, the umbilical vesicle sends a prolongation, the allantoic duct, into the abdominal pedicle, which duct is separated from the caudal side of the amnion by mesoderm. It is relatively long and probably formed early. It is through the adherent band of mesoderm that the vessels of the fetus pass to the chorionic membrane and into the villi.
The caudal knot of the primitive streak region forms the abdominal pedicle. The germinal plate is only a portion of the completed primitive streak region. There is as yet no differentiation into medullary plates or chorda. The germinal plate has its dorsal surface toward the point of union of the abdominal
Fig. 29. Change from Fig. 27, showing ventral curve due to growth in length of germinal plate. (Schematic.) M, mesoderm.
pedicle to the chorion and its long axis runs radially to the chorion. It is of oval form and has a median furrow on its dorsal surface. Its dorsal surface follows, in addition, the curve of the amniotic cavity and is therefore concave. Its dorsal furrow lies in the same plane as the lumen of the allantoic duct, and its caudal portion is at right angles to the duct. It consists of high cylindrical cells, highest at the middle (Fig. 28). Laterally it extends on into the amniotic lining. Laterally, ectoderm and mesoderm are separated by a membrana prima, which is always present between parallel layers of mesoderm and ectoderm. In the median line, however, is a fibred, granular substance, and here possibly a connection between ectoderm and mesoderm existed. A characteristic connection at the region of the primitive streak is present in mammalia and in older human embryos. There is probably no connection between mesoderm and entoderm, and in the next embryo there is no layer continuity be Vanalis neurenterious between mesoderm and entoderm posterior to the canalis neurentericus.
Fig. 29a. Stage of still further growth of cephalic end of germinal plate. Embryo Gle of Spee.
Fig. 29b. Embryo Glc of Spee. A, amnion cavity. X, between ectoderm and entoderm mesoderm comes. All anterior to the canalis neurentericus is new as compared with embryo v.H., Fig. 27.
It is to be noted that in Fig. 27 the germinal plate has a dorsal curve. The next stage is represented by a ventral curve (Fig. 29). As a result of this (1) the mesoderm between the germinal plate and the entodermal vesicle, and (2) that part of the entodermal vesicle lying parallel to the germinal plate hecome included in the ventrum of the curved germinal plate and form the mesoderm and entoderm of the fetus. The actual change is seen in Fig. 29 a and o.
FURTHER DEVELOPMENT OP THE HUMAN OVUM.
2. The next older embryo (Gle) shows that the new growth concerns the addition of new elements to the germinal plate, plus an increase in the size of the amniotic cavity and the umbilical vesicle (Fig. 29&). ,The primitive streak region*in v. H. has grown a little, but keeps its position approximately. The mesoderm of the abdominal pedicle, the allantoic duct, and the caudal part of the primitive streak region remain about the same. In their growth a pause ensued, which pause continues until the embryo has seven primary vertebra?. Therefore the added growth concerns the cranial end of the germinal plate, while the caudal end remains a fixed point. The anterior part of the germinal plate has grown to four times the size of that in v. II., with the result that it extends almost at right angles to the original germinal plate, because the caudal end remained a fixed point and thus caused a transposition of the cranial area of the germinal plate. Thus the umbilical vesicle and amniotic cavity are pushed away from their position near the chorion into the deeper part of the mesodermal slit. A continuation of this process causes the embryo eventually to lie with its ventral surface turned toward the point of adhesion of the abdominal pedicle. At the same time the umbilical vesicle has grown, too, so that the embryonal formation of Gle has added a growth almost as large as v. H. itself. In v. H. all those areas of the germinal plate are absent which in Gle turn their dorsal side to the chorion, that is, all cranial to a line drawn transversely through the canalis neurentericus (Fig. 295). The germinal plate, as a result of the rapid growth of the medullary plates, grows at right angles to the long axis of the primitive streak region of v. H. The primitive furrow has an S shape on the dorsal surface. The cranial end of the chorda formation bends ventrically and ends together with the anterior end of the medullary plate. Anterior to the canalis neurentericus the chorda entoderm and the medullary plate lie close together. At the anterior boundary of the canalis neurentericus
Pig. 30. The three layers of a human embryo, still without primary vertebrae. Transverse section. (Keibel.) Showing growth of lateral walls, which thus enclose the entoderm within them.
Fig. 30a. The forming of the intestine. Schematic. (Kollmann.) The mesoderm is divided into a parietal and a visceral layer. The celom, or space between these layers, is the future peritoneum. Intestine and umbilical vesicle are connected by a narrow duct.
the ectoderm bends into the area of the chorda entoderm and the latter possesses elements of the ectoderm.
With the continued growth of the cephalic end and the conse
Fig. 30b. — Human embryo, 2-4 millimetres long, with heart and abdominal vesicle removed and umbilical pedicle cut. (After His.) Showing connection between intestine and umbilical vesicle.
quently decided ventral curve of the embryo, as well as through the growth of the lateral walls, a portion of the entodermal sac lies within the embryo. The ectodermal germinal plate has
on its ventral surface then a strip of mesoderm and upon this mesoderm a part of the very entoderm which lines the entodermal
Fig. 30c. Caudal end of embryo, 3 mm. long. Reconstruction. (Keibel.) CI., cloaca : Md.. medullary canal ; Seine, tail ; Schw. D., caudal intestine. Showing relation of allantoic duct to the cloaca.
abdominal vesicle (Fig. 30). Anterior to the canalis neurentericus is found most of the embryo and the medullary farrow and plates. The embryo consists here of three layers.
Fig. 30d. — Embryo 296, with decided ventral curve, has turned so that the abdominal surface faces the adherent band. X, omphalo-enteric duct. The heavy black line about A, passing off from either end of the embryo, is the amnion. Int., Intestine. Umb. pes., umbilical vesicle. (Schematic.) The embryo now has its ventral surface turned toward the abdominal pedicle.
Posterior to the canalis neurentericus is the original primitive furrow with the primitive lateral plates. The embryo here consists, too, of three layers. The mesoderm of the posterior part goes over into the adherent mesodermal band, the future abdominal pedicle. At the anterior and posterior ends the ectodermal layer of the embryo goes over into the single-layered amnion.
The original cephalic and caudal ends of the embryo (the points where ectodermal germinal plate goes over into singlelayered amnion) develop decided ventral curves. So do the lateral walls or sides of the germinal plate. As a result, the abdominal vesicle becomes constricted more and more, and the wide connection of the abdominal vesicle with the entodermal area of the embryo is narrowed so that a constantly narrower portion connects the abdominal vesicle with the interior of the embryo (Fig. 30a). The portion in the embryo, the entoderm of the embryo, forms the intestine and the cloaca (Fig. 30 a and b. The cloaca is a sac into which intestine and allantoic duct enter (Fig. 30c). As a result the abdominal vesicle is connected with the intestine by what has become a narrow duct, the omphalo-enteric duct, while the allantoic duct situated in the adherent band enters the cloaca (Fig. 30d). It may be said, for the sake of a readier understanding, that the cloacal portion of the entoderm sends a prolongation, the allantoic duct, into the adherent band. (On the umbilical vesicle develop vessels, the omphalo-mesenteric vessels, which enter the mesentery of the intestines, while the omphalo-enteric duct enters the intestine near the future cecum.) Later the cloaca becomes divided into a posterior part continuous with the intestine, the rectum, and an anterior part, or bladder, continuous with the allantoic duct, the future urachus.
Fig. 30e. External scheme of embryonal formation, caudal end, with amnion removed, showing relative situation of parts. A combination of Figs. 29b and 30c. (Waldeyer.)
Chapter Till. The Chorionic Villi
EARLY DEVELOPMENT.
The ectodermal cover of the ovum has the name chorion-ectoderm to distinguish it from the ectoderm in the amniotic cavity, a part of which takes part in the embryonal formation.
This ectodermal cover evidences a great growth of cells in the entire circumference of the ovum, forming what is called the trophoblast. These trophoblast cells invade the decidual compacta. The capillaries of the compacta dilate into lacunae or wide spaces. The blood breaks through the lacuna? and now, at this early time, maternal blood comes in contact with fetal ectodermal trophoblast cells. The maternal blood when it comes into contact with the trophoblast cells changes them to large polynuclear cells, consisting of the protoplasm of several cells in which the trophoblast nuclei of these cells form a polynuclear group. Such groups and likewise large mononuclear cells result from the action of the blood on the trophoblast. Such resulting cells are called syncytial cells, mononuclear or polynuclear. They line, too, the lacuna? in the circumference of the trophoblast.
The trophoblast cells are constantly spreading in the periphery of the ovum, entering further and further into the decidua. They have a destructive action on the decidual cells ; they reach capillaries and vessels and enter the latter. Wherever they open lacuna? or vessels the outpoured blood changes the trophoblast cells with which it comes in contact into syncytium. As a result the trophoblast is divided and subdivided into small islands consisting of groups and masses of trophoblast cells. The cells on the outside of these groups are changed by blood to syncytium. Such groups of trophoblast cells surrounded by syncytium are the future villi. Subsequently mesoderm develops in the interior of these trophoblast islands or ' ' cell groups ' ' and we have young villi (Fig. 31). Later most of the trophoblast cells are displaced and disappear with the exception of a single row situated immediately beneath the syncytium. This single row, composed of large distinct cells with pale protoplasm and large nuclei, is called the cell-layer of Langhans. In the centre of such groups is thy developed mesoderm, and the so-called villi are now formed, but as yet no capillaries are present. Such extensions, composed of a centre of mesoderm and a periphery of Langhans cells, with the latter surrounded by syncytium, are the final villi in whose conuective-tissue centre capillaries finally develop which are connected with the capillaries of the fetus.
When the trophoblast first develops and. extends into the maternal compacta its margin is irregular and. serrated (Fig. 20). As capillaries on the compacta are opened syncytium is formed wherever blood touches the trophoblast cells. The points of trophoblast furthest advanced extend continually into new compacta, destroy it, and open more capillaries. In this way the process is carried on through a constantly increasing periphery. As a result long, irregular, branching, finger-like extensions of trophoblast project out from the trophoblast layers situated immediately on the external layer of mesoderm produced by the mesoderm slit. These layers are, too, changed to syncytium and cell layer of Langhans. Under them the mesoderm also grows and displaces most of the trophoblast cells. The resulting continuous outer wall of the ovum from which the finger-like extensions (villi) project is called the membrana chorii (Figs. 25, 27,29, 296, 3(M).
Fig. 31. — Schematic representation of a later stage of placental development than Fig. 24, showing young villi. (Peters.)
To the inner surface of the membrana chorii is attached the adherent band, or abdominal pedicle. It is a band of mesoderm which has grown continually longer. In it is the allantoic duct. Through it pass the vessels of the fetus to enter the mesoderm of the membrana chorii and the mesoderm of the villi.
The capillaries which develop in the villi unite with the vessels of the fetus in the membrana chorii. Thus, through the medium of the adherent band, fetal blood is brought into the villi. The villi are surrounded by maternal blood and so an exchange between fetal and maternal blood is carried on through the two layers of epithelium covering the villi (Fig. 31).
In the Fourth Week of Uterine Gestation, when the original trophoblast capsule is consumed, the ovum is loosely connected ivith the decidua by only a few adherent villi. The following remarks concern such an ovum, covered with chorionic villi, aborted in the fourth week. Its attachment in the uterus must have been exceedingly loose, for the numerous and countless villi connected with the covering of the ovum carried with them no decidua cells. It was hardened in alcohol, cut in series sections, and stained with hematoxylin and eosin. Examination showed a point of rupture in the wall through which the fetus had been expelled.
Fig. 31a. A well-developed villus showing cell layer of Langlians with "cell group or pillar" at its tip. These cell groups are trophoblast cells. The villus is covered with syncytium which is very thin over the "cell group."
The important points with regard to the villi are as follows: In a well-developed villus (Fig. 31a) we find a connective-tissue centre made up of long, thin, and branching cells situated in a basis composed of a finely granular, frothy, and often red-staining substance like that found in the fetal sac. On this connective-tissue centre is a single layer of large, sharply outlined mononuclear cells forming a continuous covering of the same. This layer frequently forms groups at the tips of the villi (Fig. 31a). This layer, the so-called layer of Langhans, is composed of large round or polygonal cells with a pale, almost waterclear, protoplasm poor in granules. The nucleus is large, round, and homogeneous and generally contains one nucleolus. The
Fig. 316. An outgrowth on the membrana chorii containing trophoblast cells in the lower portion, and showing the various changes to distinct Langhans cells in the centre, and especially to syncytium and syncytial masses on contact with maternal blood in the periphery.
layer of Langhans is separated from the stroma of the villus by a sharp outline. The side away from the mesoderm is smooth ami covered by a distinct structureless membrane. The outer syncytial covering is a thin layer of protoplasm containing a single row of dark nuclei. In the stroma of these villi may be seen round spheroidal trophoblast cells, and their change into nucleated red blood cells can be readily observed.
The younger villi and the large cell groups which represent the early formative stages of villi possess the same structure and cells as the outgrowths found on the external surface of the membrana chorii (Fig. 316). "We find villi composed entirely of spheroidal trophoblast cells surrounded by a covering of syncytium. The gradual transition from these trophoblast cells into syncytium, and the change of the trophoblast nuclei into the nuclei of the syncytium, can be distinctly observed (Figs. 315 and 32). Other villi are composed of trophoblast cells with a distinct protoplasmatic body (Fig. 32a). The trophoblast nuclei preserve their pronounced spheroidal form. The syncytial covering is at numerous points possessed of more than a single layer of nuclei and sends extensions into the trophoblast centre. Other villi composed of trophoblast nuclei possess a beginning centre of mesoderm (Fig. 33). The syncytial covering contains vacuoles in the wall of which are crescent nuclei. A further stage is represented in villi whose mesodermal stroma contains but few trophoblast nuclei and where the syncytium, thin as endothelium, rests on no layer of Langhans (Fig. 34). In numerous villi, at one end is found the typical structure of a complete villus, the syncytial covering evidencing sprouts of a polynuclear character (Fig. 35). The other end of the villus is of a younger stage. The syncytium is there at the period characterized by the frothy, finely granular character of the protoplasm, while the nuclei are irregular in form and do not stain deeply (Fig. 35). Here, too, the change of trophoblast nuclei into syncytial elements is evident. In the cell groups (Fig. 35a) we observe a covering of syncytium which at numerous points extends into the substance of the cell group, forming protoplasmatic masses of a thin endothelial character or of a polynuclear nature, and which divide the cell groups into irregular fields (Fig. 35&) wherein may be recognized the various early stages of subsequent villi (Fig. 35c) . This invasion of syncytial cells is not alone an active growth, but is due to the infiltration of a cell group by blood, which transforms the cells with which it comes into contact into syncytium. Here most distinctly can the gradual transition from trophoblast to syncytium be observed. The large, polynuclear groups and knobs of syncytium, the so-called giant cells, are found at all points in the intervillous space. The nuclei are round, flat, and crescent shape. They are very frequently attached to the villi by larger or thinner pedicles. They are frequently found at the tips of the villi, where they represent the change of the small so-called cell groups, or pillars, to syncytium. The villi are, then, in their various stages simply reproductions of what is found in the membrana chorii.
Fig. 32. Villus composed of trophoblast cells showing transitions to the syncytial covering aDd to syncytial groups on the left.
Fig. 32a. Villus composed of trophoblast cells with distinct large protoplasm.
Fig. 33. Villus with beginning centre of mesoderm. The syncytial covering contains vacuoles and crescent-shaped nuclei.
Fig. 34. Older villus with thin syncytium and no layer of Langhans.
Fig. 35. Villus showing an older stage in the left half and a younger stage in the right half.
Fig. 35a. Cell group with syncytial elements invading it at various points.
Fig. 356. Further stage of Fig. 35a. Cell group divided by syncytial elements, with the formation of fields which represent future villi.
Fig. 35c. A further stage of Fig. 356. Cell group divided into syncytial masses and villi. V 2 , villus in whose stroma are nucleated red blood cells ; 8j a syncytial mass ; T, syncytial nuclei resulting from changes in the trophoblast cells ; Tr., trophoblast cells with beginning change to syncytial nuclei ; V v villus with whose syncytial covering numerous bridges of syncytium are connected.
Chapter IX. The Membrana Chorii
The great growth of the ectodermal cover in the ova of animals has been made known to us by Van Beneden, Duval, Nolf, and especially by Hubrecht, who gave it the name trophoblast.
In 1889 Hubrecht, in examining the placenta of the hedgehog, found a decided resemblance in numerous points to the human placenta. He asked then that the following questions with regard to the human ova should be studied :
- Can, in the earliest stages of human ova, evidences be found of a trophospherical tissue between the villous covered ovum and the inner surface of the decidua reflexa?
- Are there in this tissue blood vessels which receive their supply from those blood vessels which run in the reflexa?
- Can evidences of a trophospherical tissue be found in the serotinal region?
The discussion of the histology of gestation in both uterus and tube shows that the various processes in the development of the human placenta resemble these observed in animal placentation.
It must be noted that these processes follow the steps observed by Hubrecht, Maximow, Opitz, etc. Yet there are still many diverging views as to the origin of the syncytial covering of the villi, as has been also observed in this regard in the investigations in animals.
Selenka and Strahl, in their examination of young human ova, find their views, gained in the examination of animal placentas, sustained— namely, that the syncytial layer originates from the uterine epithelium. "With this view Kossmann and Merttens agree. Eckardt finds that the syncytium originates from the maternal endothelium. Spee states that the syncytium develops from the connective-tissue cells of the decidua. Langhans considers the syncytial layer ectodermal, and the inner layer of Langhans mesodermal. Leopold and Gaisser consider the layer of Langhans to be of mesodermal origin because they find these cells in the mesoderm of the villi. Frankel is uncertain as to the origin of the syncytium in human ova, and finds transitions between the cell of Langhans and cells situated in the mesoderm of the villi. Kastschenko, Minot, Van Heukelom, and Ulesko-Stroganowa consider both layers to be of fetal origin.
Eckardt, who holds that the syncytium originates from the maternal endothelium ( ? ) , states that the capillaries of the decidua which form lacunas under the surface have a varying character. Many possess a distinct growth of the wall elements, which is often so great that he would consider these areas to be sections of glands, were it not for the blood therein contained. We knoAV that, in the decidua menstrualis and graviditatis, blood may enter the glands between the epithelial cells or may break into the glands. The epithelium, which, especially in the neighborhood of the ovum, grows distinctly and shows an enlarged elongated protoplasm, resembles to a certain degree the syncytium. These cells, however, degenerate through the action of the blood and the glands are destroyed or pushed aside. From his description it is quite evident that Eckardt was describing such areas, which he mistook for a growth of maternal endothelium. With these remarks the views of Eckardt may be dismissed.
Merttens found in the particles obtained by curetting sixteen days after the last menstruation a few sections of an ovum with the enveloping decidua. He describes (1) the chorion and the villi. On the latter are cell groups, and between them are found spaces constituting the intervillous space. (2) The spongiosa, containing numerous glands, and (3) the compacta, a pale zone lying between 1 and 2 and containing large pale cells, between which are numerous darkly stained nuclei.
In the compacta he finds large cells and large spaces. Between the large cells syncytial masses are irregularly distributed. The cell spaces are round, long, or irregular, and often empty into the intervillous space. They contain blood and are lined with syncytial masses, which at some points are very thin and at other points quite thick. Where these spaces empty into the intervillous space the syncytial masses continue into the syncytium of the villi. Merttens does not know whether these spaces are glands, vessels, or lymph spaces. They are possibly, however, the lacunae of Hubrecht, Peters, and Opitz.
The epithelia of the glands are like beaker cells, and on their free tips is a half-moon of glycogen. The glands show papillary projections (compare Fig. 145). Merttens believes that the syncytium results through a change of the surface and gland epithelium ( ?). In his Fig. 8 Merttens. represents, in the upper portion, the epithelium of such a gland, and the lower half represents syncytial masses. He believes that the latter result from these epithelial cells, which lose their cylindrical form and unite. From his descriptions and his drawings it is neither clear nor probable that the epithelium changes into final syncytial masses. Besides, this area is taken from decidua particles not connected with the ovum, and at no point can he find the epithelium of the glands contributing in any tvay to the syncytium of th.e chorion.
On the contrary, this ovum is at the stage where the trophoblast is almost consumed by the growth of the intervillous space, and the cell groups at the end of the villi, which Merttens calls points of union between the villi and the decidua, are really the remains of the trophoblast.
In a very early ovum described by Spee the villi are covered with two layers. The inner, the cell layer of Langhans, he attributes to the ectoderm. The outer layer, the syncytium or adventitia of the ovum, he describes as follows : ' ' This layer is often lifted off from the chorion ectoderm. It appears as a continuous thin streak of protoplasm with more or less closely grouped nuclei arranged in a single row. In the layers of the enveloping zone lying near the ovum are found cells which, through a diffuse staining of the nucleus and through the vacuolar character of the protoplasm, resemble the cell elements of the syncytium very much. In the space between the serotina and the ovum (intervillous space) we find them often close together and not distinctly separated, so that here the early stages of the polynuclear protoplasmatic groups are present. Suclt groups are also found united to the membrana chorii. Concerning their origin opinions differ. I have never observed a mitosis or an amitosis in their nuclei. The idea that the chorion ectoderm furnishes these masses may be set aside because of the sharp division between these two layers by a cuticula. These conditions prove that the syncytial formation does not increase through a division of the nucleus or the cell in the intervillous space. Since, however, an increase in the amount of the syncytial substance occurs within the intervillous space, this can only be explained through a ivandering of already finished masses from the connective tissue of the compacta into the ovum. 1 Epithelial cells cannot be considered as the source, since the maternal cavity surrounding the ovum, even in the earliest stages, shows no epithelial lining, although in the later stages closely pressed glands are present all about the ovum and their epithelium is preserved at least up to the end of the first month." It may be seen that Spee left out of consideration any possible action of the blood upon the ectoderm cells as an aid to the formation of syncytium. His decidua cells, resembling syncytium, are possibly changed trophoblast cells 1 . Cells from without probably form the syncytial covering of the villi and of the membrana chorii, in his opinion. We think they are trophoblast cells of fetal ectodermal origin, acted on by the blood — a possibility which he left out of consideration.
Fig. 36. Transverse section through the fetal sac or membrana chorii of a four- to five-weeks ovum.
Fig. 36 represents a transverse section through the greatest diameter of the ovum loosely connected with the decidua in the fourth or fifth week of uterine gestation. The centre is a space lined with a double parallel layer of cells arranged in single file. This also loses its parallel arrangement at certain points, where cells of the same character are found in groups several layers deep.
The resemblance of changed decidua cells to the future syncytium is often striking. See foot note, p. 87.
External to these cells, in the entire circumference of the sac, is a substance staining a deeper red and composed of extremely fine, granular, and thin-fibred, cotton-like material. In it, at numerous points, are isolated and grouped cells which look like nucleated red blood cells.
The next stratum is formed of round and oval cells, of the same character as the lining of the central space, but arranged in several somewhat parallel layers. Between these cells is a fine fibre-like substance, like the one just described, but taking a lighter red stain. The outer cells are rounder and more spherical than the inner, and the outermost cells, with a clear protoplasm and distinct nucleus, form a single layer of distinct cells with distinct cell boundaries (36).
The extreme external covering of the membrana chorii is of a plasmodial character, and contains, nuclei of various forms and evidences many vacuoles (Fig. 37). Each vacuole represents the space filled by a trophoblast cell, the nucleus being compressed at one point into a small crescent. At certain points outgrowths are present which contain larger and smaller areas of granular and plasmodial character, the aforementioned distinct cells, blood, and protoplasmatic groups containing small pale cells, small dark nuclei, and nuclei undergoing degeneration. Attached to the membrana chorii and all about it are innumerable villi in all stages of growth, young and old. The older villi present the same structure and possess the same cells, including the nucleated red blood cells, as are found in the chorionic membrane.
Fig. 37. Vacuoles representing body of trophoblast cells, while the nucleus is a crescent in the circumference. From the membrana chorii of Fig. 36.
The conclusion gained from a comparison of this specimen with the structure of the villi is the following: The single layer of cells immediately under the plasmodium of the chorionic membrane, the spheroidal cells under it, the distinct cells found in the outgrowths, the spheroidal cells in the young villi and in the, cell groups which form the new villi, and the cell layer of Langhans, are identical and represent the ectodermal trophoblast cells. The villi are simply excrescences of the membrana chorii.
When the blood comes in contact with the trophoblast cells it does not coagulate. It does, however, exert a decided influence on the nuclei. Strahl found, in examining the placenta of Galago, that the blood extravasated from the vessels of the uterus is made use of by the fetus, in that the degenerating products of the extravasated blood cells are taken up and absorbed. These products are found in the form of larger and smaller yellow granules in the gland epithelium, which the latter uses in furnishing an iron-containing gland secretion. In the placenta of other animals the blood extravasated from the vessels of the uterus is, taken up and absorbed by the ectoderm cells, and in certain animals the fetus obtains its nutrition because the ectoderm, covering the villus, takes up the substance given off by the uterine epithelium. Merttens observes that Lieberkiihn in the placenta of the dog, and Strahl in the placenta of the mole, find ectoderm cells taking up and absorbing red blood cells. Peters states that Tafani, in the placenta of the cat, found chorion ectoderm cells outside of the placenta taking up red blood cells. We find much blood — that is, red blood cells— in the syncytium. It is also found in the vacuoles. Peters believes that the blood takes part in the changes of the trophoblast nuclei and that its elements contribute to the formation of the protoplasmatic masses known as the syncytium. "Not only the blood plasma, but also the nuclei of red and white blood cells, pass into the composition of these masses." It may be seen in Fig. 315 that the red blood cells change into a detritus and combine, so that finally small irregular areas containing small nuclear remnants result. A gradual destruction of red blood cells takes place, and the presence of leucocyte nuclei may be observed. The plasma, when acting suddenly and in large amounts, causes the trophoblast nuclei to shrink and take on a dark stain. When acting slowly it disintegrates them, flattens them, so that in a resulting homogeneous protoplasm nuclei of all forms may be found. It is evident, then, that the protoplasm of the syncytium is the product of the blood cells, the blood plasma, and the protoplasm of the trophoblast cells. The nuclei of the syncytium are the changed trophoblast nuclei.
Wherever blood comes in contact with fetal cells syncytium results, whether in the decidua or in the intervillous space, so that syncytium really plays the part of an endothelium and at all periods, especially in the later stages, resembles endothelium so closely that it was naturally mistaken for it in nearly all the earlier investigations.
Many observers have noted a brush-like covering on the syncytium, though I have never found it. This striated surface on the syncytial covering of the chorion, and often observed on the isolated polynuclear protoplasmatic masses, appears to Spee to be a sort of fibrillation on the cell protoplasm. He believes that it originates through the influence of a sap current toward the ovum, because such a brush-like fibrillation is found in those places where a regulated transit of products through cells occurs, as in parts of the excretory ducts of the salivary glands and the kidneys on the side toward the connective tissue, and also perhaps in the osteoblasts in the Howship lacuna? of bone. 6
Chapter X. The Blood-Forming Function of the Trophoblast
In another particular, as I believe can be shown, the' resemblance between the processes of development in the human being; and those in animals is carried out still further — namely, the formation of blood by the fetal placenta.
In sections through the umbilical vesicle of Tarsius and Tupaja, Hubrecht finds, polynuclear cells which he considers to be mother blood cells. Their nuclei result through fragmentation of a large nucleus. The individual nuclei within the mother cell then become surrounded with a special circle of plasma. When the original mantle of the protoplasm of the large cell is lost, the included cells are freed, forming embryonal nucleated red blood cells. During their circulation in the embryonal fetus the nuclear membrane disappears and the nucleus changes to a drop in which the chromatin diminishes, while the protoplasm begins to resemble the former nucleus. The cells become gradually smaller, and the final forms do not result from the protoplasm but from the nuclei of the cells. The blood cells originate, then, from the original nucleus of a mother blood cell. Hubrecht finds the same steps in the placenta of Tarsius as in the umbilical vesicle. He finds the same to occur in the trophoblast and in the maternal spongia, and even in the vessels which lie between the glands. In the placenta of Tupaja the same steps are noted, but, in addition, the epithelium, as well as the connective tissue of the decidua, is the seat of red blood cells derived from nuclei.
In his ovum v.H. Spee describes the mesoderm layer as follows : He finds two different cell forms occurring side by side and intermingled : (1) Branched cells, extending into fine threads which project in all directions and which may well be considered connective-tissue fibres. Where these cells occur singly — for instance, at certain points in the abdominal pedicle and in the villi— the mesoblast appears exceedingly poor in nuclei. Strongly-stained specimens are necessary to see the numerous fine, wavy, and sharply contoured fibres of the embryonal connective tissue. (2) Between these structures are found larger, strongly prominent spindle cells with oval nuclei, arranged sometimes closely together like bundles, and at other points separated from each other by wide spaces without evident contents. The course of these fibres follows, with noticeable constancy, the curves of the free mesoderm surface — that is, the surface covered with epithelium.
In our opinion many of the second form of cells are possibly ectodermal. In an ovum described by Reichert, on the inner side of the chorion is a substance which he considers to be a mucoid-like deposit and which also extends into the villi. The cavity of the ovum is likewise filled with this substance. Spee considers this to be mesoderm tissue, although Reichert describes the contents of the ovum simply as a mucoid substance without cells: Spee says that the contents of the amnion and of the umbilical vesicle of ova hardened in alcohol never coagulate, but such a condition does take place in the wide mesoderm slit of dead young human ova.
Thus the early embryonal mesoderm tissue of the membrana chorii and of the villi is very poor in cells, and the description of Reichert, characterized by Spee as mesoderm substance, selves to characterize as mesoderm the non-celled material found between the central space and the external layers of cells seen in Fig. 36 and also found in many of the younger villi.
It has been mentioned that Langhans considers the cell layer to •be of mesodermal origin, and that Leopold holds the same view because he finds transitions between the stroma cells and the cell layer. Frankel, who believes that the cell layer and the syncytium are probably identical, finds the question difficult of solution because of the numerous villi whose interior is composed of ectodermal trophoblast cells. We have called attention to this occurrence as a frequent one, and have likewise observed the resemblance between the cell layer of the membrana chorii and the several layers of cells under it which are embedded, however, in mesoderm substance (Fig. 36). The origin of the villi, the fact that they are formed out of solid trophoblast groups, the fact that only later does mesodermal tissue reduce them to the generally single layer of Langhans, the fact that in this reduction to a single layer many trophoblast cells are left embedded in the stroma of the villi and the membrana chorii, and the numerous transitions between these cells and the cells of Langhans, prove that they are ectodermal cells situated in a basis of mesoderm substance in which only later mesoderm nuclei appear.
As the villi grow older, these ectoderm cells are crowded by the growing mesoderm tissue, so that some degenerate, while others take part in the following important changes — that is,
THEY FORM RED BLOOD CELLS.
In the same manner that the external trophoblast cells,, which come in contact with the blood, obtain from it a protoplasmatic envelope, while they themselves form the nuclei, in quite the same manner these cells situated in mesoderm are seen to gradually change their form, become darker, become surrounded by a red-staining granular protoplasm of the same character as the mesodermal tissue. They then represent nucleated red blood cells. They are often seen in stages where the nucleus becomes fragmented or divided into other cells. These larger and smaller nucleated reds are found isolated or in groups, often lying in spaces or slits of the mesoderm of the villi and membrana chorii. These spaces are often surrounded by very long, very dark, and spindle-like cells, evidently forming the endothelium of the future capillaries.
M 1 e have observed the statement that in animals the mesoderm, which enters the trophoblast groups and forms the stroma of the villi, carries with it the branches of the allantoic vessels. Vessels, however, are not present in the villi of the human ovum until the third week, and the villi are then filled with mesoderm or ectoderm cells, and it would be impossible for extensions of the allantoic vessels to enter into the innumerable extensions of the membrana chorii constituting the villi. The process followed, however, is probably the following :
Mesoderm does not enter as a distinct tissue into the trophoblast elements after they have been reduced by the maternal blood to syncytium, but is present between the trophoblast cells from the very earliest period, as may be seen in the description of a tubal ovum. When, therefore, a trophoblast cell group comes in contact with maternal blood, the outer cells are changed to syncytium, underneath which results the cell layer of Langhans, which in the still later periods disappears. The mesoderm substance, when increasing in amount, dilates, the villus and forms the stroma. In the resulting stroma are left the remaining more or less scattered trophoblast cells. From these, nucleated red blood cells are formed, which lie in small slits or spaces, which spaces become lined with endothelium, thus forming capillaries. These capillaries gradually increase and finally become very numerous, having a tendency to lie close under the epithelial covering of the villi. "Whether any of these trophoblast cells take part in the formation of the endothelium, it is impossible to say with certainty. These same processes are observed in the membrana chorii. These capillaries in the villi and in the membrana chorii later unite with the umbilical vessels which make their way through the abdominal pedicle.
Fig. 38. Membrana chorii of tubal ovum.
The nucleated red blood cells, in their subsequent circulation through the fetus, become changed, and from the third month on ordinary red blood cells are found. In the membrana chorii of our uterine ovum the same stages of capillary development may be observed, but to a less extent than in some of the villi which already possess numerous, and distinct capillaries. In the later stages this process is more marked in the membrana chorii than in the villi, as may be seen from the following description of a tubal gestation with well-preserved fetus i 1
J The possibility that these nucleated red blood cells came from the fetus was not left out of consideration.
86 BLOOD-FORMING FUNCTION OF THE TROPHOBLAST.
The fetus was lying in the central cavity of the ovum (Fig. 38) attached by an umbilical pedicle which entered the placenta at the site to be mentioned later. The fetus was one centimetre long; the abdominal wall was not yet closed, and the arm and leg formations were just evident as small pinhead knobs. The cavity of the ovum is lined by a membrane composed of flattened cells with distinct nuclei. At various points in the circumference of the membrana chorii, and especially at the point where the abdominal pedicle is attached, are numerous larger or smaller spaces, separated, sometimes, from the maternal blood by only a single or double layer of cells, which at many points are of a distinctly plasmodial character. The membrana chorii has at various points, and especially at the placental site, numerous villi attached to it and numerous small projections of the same structure as villi. These spaces, or sinuses, contain masses of round, red-staining protoplasmatic masses with dark central nuclei, many of which are undergoing division— nucleated red blood cells. It seems possible that many of these sinuses or spaces represent dilatations of the parallel row of cells observed in Fig. 36, wherein were noted, at various points, groups of cells of a trophoblast character. It is probable that those groups too form the nucleated red blood cells observed in these sinuses.
The largest of these sinuses are present near the insertion of the abdominal pedicle, and all of them are separated from the maternal blood of the intervillous space, often by only a single layer. These sinuses may represent, then, areas in the membrana chorii filled with nucleated red blood cells of placental trophoblast origin, which subsequently enter the fetal circulation.
In the pedicle itself a change to the subsequent non-nucleated red blood cells may be observed, for in its substance are fetal vessels and sinuses filled with cells of a different character. They are small, with a thin circumference of protoplasm and a dark nucleus filling out almost the entire cell body. These represent, then, the later stages of the red blood cells.
The resemblance of this process to the one noted by Hubrecht in Tupaja and Tarsius carries out still further the resemblance of the various processes in the human placenta to those in the placentas of animals. That this theory and explanation, whereby red blood cells are formed of trophoblast ectodermal cells, is a rational one and proven by the examination of our specimens seems to me evident. In addition, it serves to explain the presence of trophoblast cells in the interior of the villi — a fact which has led many, who have considered them mesodermal because situated in the mesodermal stroma, to likewise call the cells of Langhans mesodermal. The formation of nucleated red blood cells from trophoblast cells, on the addition of a protoplasm of mesodermal origin, would serve to make their resemblance to syncytium very great; for the latter is composed of trophoblast nuclei with a protoplasm largely composed of maternal blood plasma. If, as many sections have suggested, the capillaries were lined by endothelium which is also formed of these trophoblast nuclei, the resemblance of this process to the formation of syncytium would be further increased; for the syncytium simply plays the part of endothelium, separating the other fetal cells at all times from the circulating blood.
Uterine (as well as tubal) ova furnish us with the following positive conclusions:
- The human ovum possesses an ectodermal growth of cells, the trophoblast, consisting of closely-grouped cells.
- When vascularized by maternal blood, a second external layer, consisting of plasmodial mononuclear and polynuclear elements, results.
- Elements of the maternal blood circulating in the spaces and lacunas of the trophoblast contribute to the protoplasm of the syncytium. Among other elements, the secretion of the uterine or tubal epithelium may likewise contribute to the formation of the syncytial protoplasm. At any rate, much of the protoplasm (but none of the nuclei) is of maternal origin.
- On the villi and the membrana chorii the plasmodial cells form the outer syncytial layer, ivhile the closely-grouped cells beneath it furnish the single layer of Langhans.
- The stroma of the chorionic villi is formed of mesodermal tissue in which are later found capillaries communicating with the umbilical vessels and containing fetal blood. Clear in almost every detail, then, a trophoblast formation, consisting of an inner layer of separated cells and an outer or plasmodial layer such as is found in the placental development of animals, is present in human placentation.
Note. — It is to be noted that the embedding of the guinea-pig's ovum reveals symplasmatic changes in the decidua which make Spee's theory of the maternal origin of the syncytium very attractive. Certain it is that the decidual cells undergo "syncytial changes." Were we to go but one step further and add to the maternal blood symplasmatic decidual structures as an external factor in the production of syncytium, then the theory of the exclusively fetal trophoblastic origin of this tissue would fall to the ground. The distinction between fetal and maternal cells is often decidedly difficult, and in that fact lies the crux of the problem. If the view we have chosen be correct, it must still be granted that the decidua undergoes primary or secondary changes which make its resemblance to real syncytium striking. Though often and in many specimens led to favor Spee's view by microscopic appearances, yet our choice of views (by no means surely excluding, in whole or in part, the views of Spee) seems well founded.
Structures not wisely called 'syncytial' may be formed from various forms of tissue, as uterine epithelium, uterine connective tissue, fetal ectoblast, etc. Therefore, especially when we consider the variations in placental formation in various species of animals, it is not correct to speak of 'the syncytium' as if all syncytial formations were alike. Therefore, in the guinea-pig, I did not use this word, but chose the term 'symplasma' to designate those structures (developed from connective tissue) comparable to syncytium" (v. Spee). Van Beneden calls this tissue, developed from ectoblast in animals, Plasmodium. Plasmodium is, then, in the human ovum "trophoblast." We believe "syncytium" to be the "Plasmodium" of animals. Decidual and other uterine cells undergo the so-called "syncytial changes." It would be advisable to call these "symplasmatic" cells. The question then is: Is syncytium of symplasmatic or plasmodial origin? "We hold the latter view.
Chapter XI. The Further Development of the Uterine Placenta
Just as during the early weeks the trophoblast invades the trophospongia or decidua, so after the formation of villi is the further course of the ectodermal trophoolast and syncytial cells of a destructive character, so far as the decidua is concerned. Fig. 39 presents a fetal sac in situ in the sixth or seventh week of uterine gestation. The specimen from which the drawing was constructed was unfortunately distorted, yet the important relations are very clear.
Fig. 39. Uterus and fetal sac in situ — 7 weeks — two-thirds the size of the specimen when mounted, and one-half the size of the specimen before hardening. y, decidua vera with numerous glands, i.e., well-marked spongiosa ; x, decidua vera with compacta compressed through pressure of the sac, and evidencing few flattened glands in the spongiosa.
The capsularis, to which villi are attached, is full of darkly-staining trophoblast cells, between which and through which are blood spaces and blood extravasations. Opposite it, but not yet in contact, is the decidua vera, flattened by pressure of the growing sac, and composed of pure decidua divided into a superficial layer, the compacta, and a deeper layer of flattened glands, the spongiosa (Fig. 40). Where the decidua vera is not compressed, as at the areas where decidua vera, reflexa, and serotina join (Fig. 39), the decidua retains in its deeper layer the typical character of the spongiosa, evidencing numerous glands of all sizes and lined by preserved epithelium of a "syncytial" character (Fig. 14&).
Fig. 40. High-power drawing of decidua vera (compressed) of Fig. 39.
The decidua serotina evidences in the deeper layers few flattened glands. The superficial layers are greatly changed. Where the villi come in contact with decidua the syncytium disappears and the cell groups enter the maternal tissue and mingle with it (Fig. 41). This process is carried on, then, by all the attached villi also, so that the resulting "decidua" is of the same character as the cell groups. This resulting tissue resembles the decidua, but its nuclei take a deeper stain and it evidences no small-celled infiltration. In it are found cells composed of a structureless mass enclosing one or more cell nuclei or groups of nuclei. They resemble syncytium and are simply changed fetal cells. Without the aid of these syncytial cells, which infiltrate the maternal tissue very thoroughly and in all directions and quite deeply, it is difficult, with the exception of the darker staining, to mention characteristics which to the beginner would differentiate fetal cells from the decidua. It is this fact which has made the various questions depending on this differentiation difficult of solution.
Fig. 41. Cell groups of villi entering maternal tissue. Taken from the serotinal or placental area of Fig. 39.
Fig. 42. Dark syncytial cells infiltrating decidua serotina of Fig. 39.
The boundary between fetal and decidua cells shows degenerative changes; the superficial glands are pushed aside and destroyed, while the deeper glands grow, their epithelium swells, unites and forms so-called syncytial changes. These masses fall off and finally degenerate. The fetal cells at all periods infiltrate the decidua and bring it to destruction. The advancing ectoblastic and syncytial cells have an erosive action on the vessels which prepares them and the capillaries for bursting. In this way new lacunas and areas of degeneration result, and the blood from these open vessels changes the fetal cells to syncytium and to villi and constantly increases the extent of the intervillous space.
The cell groups of the villi later diminish and disappear. The villi increase in number and are closely grouped. Their stroma consists of star-shaped cells, between which are cells resembling those of Langhans. The rest of the stroma is filled out with numerous capillaries, and finally the syncytium is reduced to a thin substance containing nuclei (Fig. 44).
Chapter XII. The Placenta
That part of the decidua covering the embedded ovum, plus the scar of Reichert, forms the capsularis, or decidua reflexa. That part of the decidua in which the ovum is embedded, and on which the ovum rests in its early stages, is the serotina. Here the main changes between the ovum and villi on the one hand, and the decidua and maternal blood on the other hand, take place. The remainder of the decidua is the vera.
The villi in the entire periphery of the ovum depend for their growth and development on connection with the maternal decidua and blood. At the end of the first month the villi are evenly distributed over most of the periphery of the ovum. With the growth of the ovum in the next two months there is a stretching of the capsularis, which, however, grows likewise, so that it is not much thinned except at its summit. There is, however, in these two months a constantly slighter connection of the vessels of the capsularis with the maternal vessels of the vera and serotina. In addition the fetal vessels w T hich enter the membrana chorii through the adherent band establish closer and more immediate relations with the villi at the serotina, for the abdominal pedicle is at this point.
As a result we distinguish two divisions in the chorion: (1) that in which new villi cease to develop and in which formed villi gradually degenerate and atrophy — the chorion Iceve; and (2) that in which the villi increase hugely in number and size, the area, at the serotina — the chorion f rondo sum.
The chorion frondosum forms the placenta. The growth of the uterus in the first three months is independent of the growth of the ovum, and the uterus undergoes eccentric development. Therefore the area of the serotina increases in extent. The ovum grows of its own accord, and as a result the area of the chorion frondosum increases in extent and keeps pace with the growth in extent of the serotina. Septa, of decidua extend between villi and groups of villi, due to the irregular invasion of the serotina. As the ovum grows in the first three months it is covered by capsularis (Fig. 39). Though the capsularis at the end of the third month covers an ovum as large as a goose egg, it is fairly thick except at its summit, and is in contact with the decidua vera in its entire circumference. During the fourth month the capsularis unites at all points to the vera and its nourishment ceases except at its oase. The area where capsularis at its base joins the serotina and vera is known as the Border Zone and constitutes the boundary of the ' ' placental area" in the first three months. The base of the capsularis unites last with the vera. Septa of serotinal decidua extend between villi and groups of villi, especially at the point where capsularis, serotina, and vera join, and there lie close to the membrana chorii, forming a maternal border or margin to the placenta — i.e., at the border zone the decidua is supposed to extend up to and touch the membrana chorii as Winkler 's Plate.
In the early three months, up to the formation of the placenta, even though the uterus grows actively, the growing chorion frondosum and the base of the chorion Jaeve extend into vera and split it into two layers ( ?). The lower layer becomes serotina and the upper layer is added to the capsularis. From the end of the third month on, the uterus enlarges passively through growth of the ovum. It is scarcely possible that the edge of the growing placenta then likewise splits the vera into two layers to any extent, but in its growth it will extend, strictly speaking, not upon vera, but upon the base of the capsularis which has united to vera. The villi do not atrophy on every point of the capsularis. They may persist on the part of the capsularis nearest to the vera and serotina. When capsularis unites to vera these villi may grow through the united capsularis and vera. As a rule the loosest union between capsularis and vera is at this point and so the loosest union of villi and placenta to decidua is at this point.
Three groups are observed in mammalia, as regards the character of the chorion.
(1) The chorion is smooth and is attached to the uterine mucosa, which is rich in vessels. The chorion takes from the large epithelial cells of the uterus nourishment for the embryo.
(2) The chorion has projections or villi. An allantois approaches the chorion, and contained umbilical vessels enter the villi. The chorion and the mucosa are closely connected. In the pig, for instance, numerous projections, rich in vessels, fit into smooth depressions in the mucosa, in which open the uterine glands. In labor the villi and the uterine mucosa are separated without loss of mucosa substance.
(3) At one or more parts of the chorion a placenta develops composed of placenta fetalis and placenta uterina. In the sheep, cow, and ruminants a subdivision exists. Numerous small placentre or cotyledones are present. The villi are covered with flat cells and the depressions of mucosa are lined by cylindrical cells. The latter develop a so-called uterine milk for the nourishment of the fetus. All other mammalia with a placenta evidence a very close connection betiveen the maternal and fetal parts, and in labor a decidua is cast off. Here a syncytium forms the separation between the villi and the maternal blood.
Fig. 43. Low-pressure drawing of uterus and placenta at full term, showing the close but uneven attachment of the placenta, two-thirds of actual thickness. To the right the villi are on the muscularis. To the left (marked Decidua) there is spongiosa. In hardening a separation formed between compacta and spongiosa at this point.
Fig. 44. Utero-placental junction at full term. 8 and the other spaces are maternal vessels. Villi are projecting into maternal sinuses. U.W., uterine wall infiltrated with fetal cells, especially with the very dark giant syncytial masses. Of the four septa between the villi, the two outer are "adherent villi," the two inner are decidual septa. Some of the sinuses are possibly glands with lost epithelium.
Fig. 45. High-power drawing of an area in Fig. 44, showing the invasion of maternal tissue by fetal cells even at full term, and also the entrance of villi into the uterine veins through the blood current.
Fig. 46. — High-power drawing of placental villi of Fig. 44, showing the free syncytial masses and the chorionic syncytium to be identical with the syncytial giant masses of Fig. 45.
The invading trophoblast and syncytial cells have a decided poiver of wandering. These wandering cells are often found singly, entering between the muscle and the connective-tissue bundles, in the lymph spaces and often in the blood vessels.
Through pressure they are often reduced to thin, long, spindleshaped forms, and, when found, the muscle fibres between appear to be changed forms of the latter. In the earlier periods, round or polyhedral cells with very large, round or irregular, long, darkly-staining nuclei are found and have been generally mistaken for decidua cells. Their nuclei are often very large and on degeneration contain vacuoles.
In the specimens (Figs. 43, 44) on page 95 is seen a section through a placenta and the uterine wall at full term. The villi are very closely grouped. The uterine wall evidences large sinuses and is thoroughly infiltrated with fetal cells and many giant syncytial masses 1 of the same character as the syncytial covering of the villi. In the drawing may be seen four extensions between the uterine wall and the main mass of the placenta. Between the extensions loose and attached villi, as well as free syncytial masses, are present. The two middle extensions belong to the uterine wall, but they are thoroughly infiltrated with fetal cells. On their sides and at their tips villi are attached, sending at these points their cells in the uterine wall.
The two outer extensions are the so-called adherent villi firmly embedded in the uterine wall, and their tips are outlined by more closely grouped and more darkly stained ectodermal cells. It is from points like these that the ectodermal cells and the giant cells invade most deeply the uterine wall, as may be seen in Fig. 44. The spaces between these extensions represent the mouths of the maternal sinuses which send their blood into the intervillous space.
In the case of normal uterine gestation villi do not project into the arterial openings of the intervillous space. They do, however, project normally not only at the border sinuses, but at all the serotinal points into the veins alone. The villi are of normal structure and often so numerous that they occlude the vein lumina. They are frequently very long and follow the course of the veins for a considerable distance, so that in the uterus villi may be found in direct contact with the uterine muscle or, better, in the veins of the uterine muscle (Fig. 45).
From the very earliest period of trophoblastic development trophoblast cells may be carried into the maternal circulation through the blood lacuna? and the blood capillaries. In the latter stages the trophoblast cells invading the decidua, eroding the vessels, and destroying the decidua furnish still further opportunities for the entrance of fetal cells into the maternal circulation. When the intervillous space is well defined and is limited in its entire circumference by the point of union of the decidua vera and the capsularis (decidua refiexa), a still further opportunity is furnished to syncytial masses, cell groups, and even villi to be carried through the veins into the maternal circulation. In the still later periods and at full term, villi projecting into the maternal veins may be carried off, and the fetal cells which have invaded the decidua and the uterine Avail, and which even up to the last days of gestation continue to enter the maternal vessels, may readily enter the maternal blood current. In eclampsia such elements have so frequently been found in the cirsulation, and especially in the lungs, that they have been considered the cause of this affection. They have, however, been proved to be rather the result than the cause, for Schmorl and others have found them in these locations in perfectly normal cases.
Many consider these placental giant cells to be of decidual origin So does Spee.
The important fact remains that from the very earliest moment, not only in the primary intervillous space but in the fullyformed intervillous space, as well as through the vessels of the uterine decidua and ivall, fetal cells are continually entering the blood of the mother.
Chapter XIII. The Umbilical Vessels and Cord
A. Umbilical Vessels
The ovum possesses its fluid centre or yolk. It may possess a covering of discus proligerus and albumin. On embedding the trophoblast digests the decidual cells and is surrounded by the so-called symplasmatic fluid. The ovum develops and the trophoblast grows. During this time osmosis and the yolk are sources of nourishment.
As the decidua is invaded capillaries are opened, and in the first few days trophoblast is acted on by blood of the mother. It changes trophoblast cells to syncytium and probably blood elements enter into the composition of the cells. Osmosis again serves to explain the growth of the ovum and its contents. On the interior of the ovum we have the embryo, consisting of ectoderm, mesoderm, and a lining of entoderm, which entodermal lining is a part of the entoderm of the yolk sac and abdominal vesicle. The ectoderm of the embryo, consisting of stratified epithelium, is continued into the single-layered amnion reflected over its dorsal aspect. The contents of the yolk sac thus line the entoderm of the embryo. A branch of the entoderm extends into the abdominal adherent band as the allantoic duct (Figs.30cZ,46&).
As the ventral and caudal ends curve anteriorly, and the lateral walls also, they constrict the abdominal vesicle. The connection between extra-abdominal umbilical vesicle and intra-abdominal is through a resulting narrow canal, the ductus omphalo-entericus (Fig. 46 a and b). The duct is called omphalo-entericus because meanwhile mesoderm and entoderm have formed intestine and the duct enters into intestine instead of into a flat entodermal lining of the embryo. All this while arteries and veins have developed on the abdominal vesicle, the arterise and vena? omphalo-mesentericse. The arteries pass from the aorta to the vesicle, the veins from the vesicle to the venous end of the heart tube. In the first month develop two umbilical arteries and two umbilical veins. The arteries are branches of the aorta. They pass along the future lateral pelvic walls, along the later bladder, along the later anterior abdominal wall to the adherent band of mesoderm. Two umbilical veins develop, one of which atrophies. Their contents at first enter through the duct of Cuvier into the heart.
The two venae omphalo-mesenterica? pass along the intestine and anastomose at the duodenum. They send branches to the budding liver, the future hepatic veins. These pass into the end area of the venae omphalo-mesentericse which empties into the primitive heart. The liver grows and thus needs more blood. Then develop the umbilical veins, which pass through the ducts of Cuvier to the venous sinus of the heart, passing over the liver. The right vein atrophies. Some branches of the left umbilical vein anastomose under the liver with the vena? omphalo-mesenterica;. This anastomosis under the liver soon becomes the important part and finally takes all the placental blood to the liver and through the hepatic veins. Thus the umbilical blood circulates with the yolk blood through the liver and then through the yolk veins to the heart, for the end piece of the yolk veins becomes the cardiac end of the future inferior vena cava. At first the umbilical vessels are small, while the omphalo-mesenteric are large. As the yoke is sucked up the omphalo-mesenteric vessels atrophy and the umbilical grow. The branches of the latter extend on through the abdominal pedicle, through the mesoderm of the membrana chorii into the villi, and join the capillaries there. At the end of the first month the fetal heart begins to beat, and in the first month circulation through the vessels begins, and for the first time there is an exchange between maternal blood and the contents of the chorionic vessels through the syncytium and cells of Langhans. As the liver grows the yolk veins atrophy and the umbilical veins grow larger. "When the liver can no longer take care of all the placental blood the ductus venosus Aurantii is formed, and so part of the blood goes directly into the inferior vena cava. The original yolk veins form the portal circulation, which becomes active in the latter part of the fetal nine months. After birth the portal circulation, carrying blood from the intestines, pancreas, and spleen, supplies the liver. The portal circulation, as said before, develops from the yolk veins. These changes are due to the change in size and importance of the yolk, placenta, and liver. After birth the umbilical vein becomes the ligamentum teres of the liver; the ductus venosus becomes the ligamentum venosum (Hertwig).
B. The Umbilical Cord
The ductus omphalo-entericus enters the future ileum a1 a point lying subsequently near the cecum. It is obliterated in the eighth week and disappears. Sometimes it is retained and is known as the diverticulum of Meckel. It may be simply a diverticulum of the ileum. It may extend up to the umbilicus as a patent canal extending from the ileum. It may remain as a band extending between the ileum and the umbilicus.
The umbilical artery of each side forms from its first part the common iliac. The remainder passing along the pelvic lateral wall to the side of the bladder, along the anterior surface of the abdominal wall to the adherent band and umbilicus, becomes the ligamentum vesico-umbilieale laterale. The intra-abdominal portion of the allantoic duct becomes a part of the bladder and the urachus, which extends from the summit of the bladder along the anterior abdominal wall to the navel.
Fig. 46a. Embryo with abdominal mesodermal pedicle and with umbilical vesicle, showing amnion still close to the embryo, a condition still found in the third week or even later. (Ahlfeld.)
Of the umbilical veins, one atrophies. Early in its career it joins the veme omphalo-mesenterica?, which, in their later stages, are connected with the liver, and thus it enters the liver and subsequently becomes the ligamentum teres. Coming out of the abdomen of the fetus are :
1. The adherent band of mesoderm.
2. In it the allantoic duct.
3. In it the umbilical vein and umbilical arteries.
4. The atrophied umbilical vesicle and its duct, the omphaloenteric duct.
5. On the latter the atrophied omphalo-mesenterie vessels.
C. Amnion
The amnion, even in the third week, may lie close upon the fetus. In it fluid is secreted which constantly distends it. As the cephalic and caudal ends take on a ventral curve, and as the lateral walls of the germinal plate curve upward and gradually approach, and as the points from which amnion begins thus approach, the amnion comes nearer and closer to the abdominal pedicle and the omphalo-enteric duct. "When the amnion is finally distended so that it is in contact with the inner lining of the membrana chorii (6th-10th week), it must envelop the abdominal pedicle and the atrophied umbilical vesicle. The vesicle is longer than the abdominal pedicle, so that its tip lies for a distance on the fetal surface of the membrana chorii. The point of attachment of the original adherent band to the membrana chorii is the point of attachment of the abdominal pedicle to the chorion frondosum and the point of attachment of the umbilical cord to the placenta. At the umbilicus the amnion, which thus covers the cord, goes over into the abdominal epidermis. The main substance of the'cord consists of "Wharton's jelly. A long, thin cord is characteristic of man.
Fig. 466. Ovum (schematic), showing extra-embryonal chorion connected with the embryonal area by the mesoblastic umbilical pedicle. In the umbilical pedicle are the allantoic duct and the umbilical vessels. Passing from the umbilical vesicle to the intestine are the omphalo-enteric duct and its obliterated vessels. When the amnion becomes large enough to line the membrana chorii (sixth weevc or later), it presses these structures together and surrounds the then-formed umbilical cord.
Chapter XIV. Gross Anatomy of the Placenta
The placenta is a thickly spongy, fairly circular mass measuring 15-20 centimetres in diameter and about 3-4 centimetres in thickness. The surface toward the embryo has attached to it the cord and is covered, or rather lined, with the amnion.
Placenta is the finally developed membrana chorii of the chorion frondosum with its myriads of chorionic villi. Instead of each villus being connected with the membrana chorii, we have connected with the latter large stems on which are numberless branches and sub-branches covered with chorionic villi.
The outer surface of the placenta is divided by furrows into areas or islands called cotyledones. A cotyledo consists of a stem passing out from the membrana chorii. From it pass villi and large branches covered with villi, and from these still smaller branches with villi. The uterine placental area has been invaded by trophoblast cells and villi during a period of nine months, so that compacta and almost all of the spongiosa have been "eaten up." If, from a certain area, we remove compacta and spongiosa, we pass from the region of capillaries toward the region of vessels situated in the muscularis. The uterus, however, has grown actively in the first three months. The vessels of such an area have hypertrophied during this time proportionately with the enlargement and hypertrophy of all the uterine structures. In the next six months the uterus enlarges passively and a further influence is exerted on the openings of the vessels on the uterine surface — i.e.] they are stretched and opened in trumpet fashion. As a result, we find on the uterine placental surface larger and smaller sinuses lined more or less with endothelium, which endothelium may extend in trumpet fashion to various degrees.
Except at the margin, practically no glands are found beneath the decidual projections. The remnant of decidua covering the uterine placental area is very thin and is so infiltrated with fetal trophoblast cells as to be practically fetal in character. The same is true of the decidual projections.
The sinuses are situated in hollows or depressions, for the uterine surface is very irregular. As a result of irregular invasion by trophoblast cells and villi, and as a result of the deeper invasion by the "adherent villi," the uterine surface shows irregular decidual projections. Between these projections and at their base are the "sinuses." Numberless individual villi are loosely attached to the tips and sides of the projections. Masses of villi fill up the hollows or bays. To the bottom of these bays are attached the adherent villi — i.e., the large stems which pass off from the membrana chorii.
GROSS ANATOMY OF THE PLACENTA.
Former decidua vet
Glandularis or spongiosa
Compacta
Menibrana cliorii
Amnion
Umbilical vessels
Vessels in
villous branch Vessels in large placental stem
Villi Membrana cliorii
Former de- ( Compacta cidua vera )
Spongiosa
Maternal vessel (capillary)
Maternal vessel (capillary)
Gland or sinus in serotina
Decidual septum
Decidual "bay" filled with villi
The attachment of stems between decidual projections, and the extension of decidual projections between masses of villi, serve to divide off the uterine surface and the placenta into compartments. These compartments are filled solidly with villi. As a result the blood coining from the uterine arteries is limited more or less to the compartment into which it enters. We have the socalled intervillous spaces. The entire placental structure is not washed or infiltrated by all the maternal blood making exit from the uterine placental surface, but by the blood of its compartment.
No space separates external placental surface from uterine surface. The masses of villi composing the placenta have the most external groups close to the openings of the maternal sinuses. Villi and masses of villi extend into the uterine veins. This arrangement, whereby maternal blood passes out between the densely grouped villi and back again through the venous sinuses of compartments, gives the greatest and most plentiful opportunity of surrounding the myriads of villi with maternal blood. The fetal vessels passing through the cord, through the membrana chorii, through the villous stems, through the villous branches into every villus, give a tremendous opportunity for exchange between maternal blood and fetal blood through the syncytium.
The placenta is thus well attached to the uterine wall. In addition the reflexa is attached to the vera at all parts of its periphery. In addition the liquor amnii presses placenta and reflexa closely against serotinal area and vera.
At the edge of the placenta the amnion which lines it passes on and lines the membrana chorii which has not formed placenta, the chorion lasve.
From the edge of the placenta on, the membrana chorii or chorion lgeve is attached by means of the reflexa to the decidua vera.
At the edge of the placenta the attachment of reflexa and vera is not very close. This area represents the point of junction of vera, serotina, and reflexa. After union of base of reflexa to vera at this point, the edge of the placenta may extend on upon the reflexa, now united to vera. Beyond this point the attachment of chorion to vera per the reflexa is the same as at other points. The uterine wall at the edge of the placenta has at all times the best-preserved growth of glands, for here the attachment of reflexa and vera is last completed and the pressure is least.
There remains of the decidua only a thin layer at best. In some areas the villi are practically on the muscularis. At other points spongiosa is preserved, but the glands have lost their epithelia and look like vessel sinuses. At other points compacta and spongiosa are fairly well preserved. The invasion of the decidua is very irregular in character (Fig. 43). Generally speaking, little decidua separates the villi from the muscularis. The layer of Nitabuch said to separate fetal and maternal structures, and probably derived from fetal ectoderm, is varying in amount and regularity.
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
Cite this page: Hill, M.A. (2024, April 20) Embryology Book - Human Embryology (1893) 1. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Book_-_Human_Embryology_(1893)_1
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G