User:Z3292017: Difference between revisions
| Line 8: | Line 8: | ||
Lab 4 - [[User:Z3292017|Z3292017]] 11:23, 15 August 2012 (EST) | Lab 4 - [[User:Z3292017|Z3292017]] 11:23, 15 August 2012 (EST) | ||
Lab 5 - --[[User:Z3292017|Z3292017]] 10:34, 22 August 2012 (EST) | |||
==Lab 1 - [[User:Z3292017|Z3292017]]== | ==Lab 1 - [[User:Z3292017|Z3292017]]== | ||
Revision as of 10:34, 22 August 2012
Lab Attendance
Lab 1 - Z3292017
Lab 2 - Z3292017
Lab 3 - Z3292017 10:13, 8 August 2012 (EST)
Lab 4 - Z3292017 11:23, 15 August 2012 (EST)
Lab 5 - --Z3292017 10:34, 22 August 2012 (EST)
Lab 1 - Z3292017
Lab 1 Online Assessment
Question 1: Identify the origin of In Vitro Fertilization and the 2010 nobel prize winner associated with this technique:
The origin of IVF can be dated from the late 19th Century where embryo transplantation in rabbits was discovered by Walter Heape. The development of IVF was due to a cascade of events during the 20th century. Pincus and Enzmann from Harvard University suggested the possibility that mammalian eggs are able to develop normally in vitro in 1934. In 1948 Menken and Rock exposed 138 oocytes to spermatozoa in vitro. In 1959, Change was able to provide evidence for IVF by fertilising rabbit eggs with capicated sperm and thus achieve birth. From 1965 Robert Edwards attempted to fertilise human oocytes in vitro. In 1968 Edwards successfully fertilised a human egg using a human culture media he developed. Finally after years of research and failed attempts, the first test tube baby was born in 1978. Robert Edwards was awarded the Nobel Prize in Physiology and Medicine in 2010 due to his immense development and contribution of IVF.
References
- http://www.ivf-worldwide.com/ivf-history.html
- http://en.wikipedia.org/wiki/In_vitro_fertilisation
- http://www.nobelprize.org/nobel_prizes/medicine/laureates/2010/
Question 2: Identify and add a PubMed reference link to a recent paper on fertilisation and describe its key findings:
Cleavage speed and implantation potential of early cleavage embryos in IVF or ICSI cycles by Lee, Lin and Hwu (July, 2012) attempted to determine the correlation of early embryo cleavage, its speed and the potential implantation rates for IVF. Their definition of early cleavage was embryonic mitosis occurring 25-27 hours after insemination. The embryos’ (day 3) cleavage speed was assessed and rated into 3 groups: rapid (more than 9 cells), normal (7-8 cells) and slow (less than 7 cells) along with their morphological quality being either good or poor. Normal fertilisation was determined by the presence of 2 nuclei and 2 polar bodies. 25-27 hours after IVF an early cleavage examination took place to determine which embryos had already cleaved. They embryos were then examined for their quality from 66-68 hours after IVF.
Early cleavage emrbyos developed normally in comparison to non early cleavage embryos. Notably, the early cleavage embryos produced a greater amount of “good quality” embryos and subsequently the implantation rate was sufficiently greater with early cleavage embryos. This finding is of great importance as embryo morphology is the most important tool to select the best embryo to transfer andthus increase the rates of implantation, pregnancy and live birth.
References
Lee MJ, Lee RK, Lin MH, Hwu YM Cleavage speed and implantation potential of early-cleavage embryos in IVF or ICSI cycles. J Assist Reprod Genet. 2012 Jul 25 PMID: 22825967
Lab 2 - Z3292017
Lab 2 Online Assessment
Question 1: Image from journal source
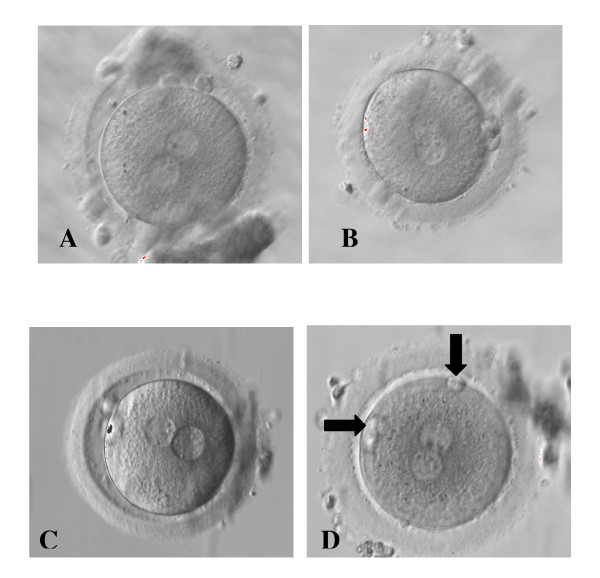
Zygotes showing different distribution of NPB in the 2PN and different PB alignment [1]
Reference
- ↑ Alessia Nicoli, Francesco Capodanno, Lucia Moscato, Ilaria Rondini, Maria T Villani, Antonella Tuzio, and Giovanni B La Sala (2010) Analysis of pronuclear zygote configurations in 459 clinical pregnancies obtained with assisted reproductive technique procedures Department of Obstetrics and Gynecology, Arcispedale Santa Maria Nuova, Reprod Biol Endocrinol. 2010; 8: 77. NCBI
Question 2: Identify a protein associated with the implantation process, including a brief description of the protein's role
Proprotein convertase 6 (PC6) is a necessary regulatory molecule for embryo implantation which generates bioactive proteins such as growth factors, peptide hormones and adhesion molecules. It is produced in the uterine stromal cells in particular at the embryo attachment site throughout early pregnancy in mice. In order for implantation to occur, the uterus ungergoes morphological and physiological changes, one being differentiation of endometrial stromal cells.
Studies have shown that PC6 mRNA is upregulated in particularly at the site of embryo attachment in the mouse uterus, being predominantly at the antimesometrial pole undergoing decidualisation. These results imply that PC6 is associated with decidualisation. From this study, the researchers were able to determine that endometrial PC6 is imperative for maternal stromal decidual response for an implanting embryo during the time of implantation. They discovered that endometrial PC6 is produced explicitly in decidual cells (the vascular and cellular changes in a uterus in preparation for pregnancy) and is not found in other cells as well as the embryo. Similarly, they noted that inhibition of the production of PC6 early on (around day 3.5) using anti-PC6 MO blocked the decidualisation and thus impeded implantation. Notably, PC6 is produced in the late secretory phase of the menstrual cycle in preparation for implantation.
Reference
Guiying Nie, Ying Li, Min Wang, Yi Xun Liu, Jock K. Findlay and Lois A. Salamonsen Inhibiting Uterine PC6 Blocks Embryo Implantation: An Obligatory Role for a Proprotein Convertase in Fertility Biology of Reproduction April 1, 2005 vol. 72 no. 4 1029-1036. Biology of Reproduction
Lab 3 - Z3292017
Lab 3 Online Assessment
Question 1: Difference between post fertilisation age and gestational age
Post fertilisation age (embryonic age) is dated at fertilisation of the egg which is approximately 2 weeks after the gestational age. This however is far less easy to determine than the gestational age as they calculate the time of ovulation as the oocyte is normally fertilised within the 12 hour period after ovulation.
Gestational age is the date of the beginning of the last normal menstrual period and is clinically more commonly used as it is a much easier method to calculate. Notably, the crown-rump length of the fetus along with the head and femur length are later used to confirm the estimated age of the fetus.
Estimation of gestational and embryonic age
Question 2: 3 different types of tissues formed from somites
Ventromedially, the somite differentiates into the sclerotome which forms the vertebrae and the ribs. Studies have shown that Pax-1 is essential for the ventral sclerotome differentiation. The sclerotome differentiates into the vertebrae and ribs through bone formation. Role of Pax-1 in skeleton development. This is primarily initiated with mesenchymal cells which assists the formation of the pre-cartilage mass via chrondrocytes and subsequently cartilage formation. Bone then develops through the replacement of cartilaginous tissue with bone tissue. Development of bone and cartilage
Dorsolaterally, the somite first differentiates into the dermomyotome which then creates 2 regions. The myotome region forms primordial muscle cells (myoblasts) and the dermatome region forms the fibroblasts (dermis). Development of Muscle
Dermatome along with Neurotrophin-3 assists with the early formation of the dermis. Role of Neurotrophin-3 The dermal papillae consist mainly of fibroblasts and is located close to the epidermis. It contains both elastin and collagen fibres (produced by fibroblasts) with the elastin fibres perpendicular to the surface of the skin. The reticular dermis accounts for the majority of the dermis with multidirectional elastin and collagen fibres. Notably, in the dermal papillae, a plexus consisting of numerous blood vessels are found but do not penetrate into the epidermis. Some nerves within this region do penetrate through to the epidermis via free nerve endings which are linked to nerve corpuscles, such as Meissner's plexus. Dermis formation
Myotomes are separated into epaxial muscles and hypaxial muscles via primordial muscle cells . The epaxial muscles form the skeletal muscles dorsal to the vertebral column known as the erector spinae muscles. The hypaxial muscles form the ventral skeletal muscles which contribute to the lung and limb formation. The skeletal muscle fiber is long, cylindrical and multinucleated, with peripherally located nuclei.
Lab 4 - Z3292017
Lab 4 Online Assessment
Question 1: 2 invasive prenatal diagnostic techniques related to the placenta:
1. Amniocentesis:
A relatively common yet invasive procedure normally conducted between weeks 15-18 of gestation. A 22 gauge needle is inserted through the anterior abdominal and uterine walls (around the region of the umbilicus) of the mother into the amniotic cavity. Of the approximate 200mL volume that the mother is carrying at this early stage of pregnancy, only 15-20mL can be withdrawn safely. There is usually little risk when performing this procedure as an ultrasonography can be used concurrently to outline the fetal and placental position.
Amniocentesis is a procedure used to determine many genetic disorders such as Down Syndrome and also neural tube defects such as spina bifida cystica. Amniocentesis - The Developing Human
2. Chorionic Villus Sampling:
Trophoblastic tissue biopsies between 5-20 mg can be obtained through inserting a needle through the abdominal and uterine walls of the mother into the uterine cavity. This can also be completed transcervically using a polyethylene catheter through the cervix to obtain a chorionic villus sample. There is a slightly greater risk of miscarriage after this procedure has been performed when compared to amniocentesis (of around 1%).
Chorionic villus sampling is a procedure used to detect chromosomal abnormalities and also X linked disorders. The benefit of CVS over amniocentesis is that it can be performed between the 10th-12th week of gestation and thus giving an earlier diagnosis. Chorionic Villus Sampling - The Developing Human
Question 2: Paper using cord stem cell therapeutically discussion of findings:
Lim JY, Jeong CH, Jun JA, Kim SM, Ryu CH, Hou Y, Oh W, Chang JW, Jeun SS Therapeutic effects of human umbilical cord blood-derived mesenchymal stem cells after intrathecal administration by lumbar puncture in a rat model of cerebral ischemia Stem Cell Res Ther. 2011; 2(5): 38 PMID: 21939558
In this paper, the researchers investigated the effects of therapeutic potential of mesenchymal stem cells after intrathecal administration by lumbar puncture in a rat model of stroke. Following this, the researchers then investigated whether the mesenchymal stem cells could enter and survive in the brain, and their potential to improve post stroke functional recovery. Mesenchymal stem cells (MSC) are a promising therapeutic strategy for the treatment of stroke due to their high proliferative capacity and also that they can be easily obtained.
The mesenchymal stem cells were injected intrathecally in some rats and intravenously in the others three days after Middle Coronary Artery Occlusion (MCAO) using isoflurane anesthesia. A 1cm incision was made over L3-L5 spinous processes and a neonatal lumbar puncture needed (25 gauge) was inserted into the spinal canal. MSCs (1 × 10^6) was diluted with 20 μl PBS being injected into the CSF over 30 seconds. Intravenously, MSCs (1 × 10^6) was diluted with 700 μl PBS were injected slowly for five minutes via an intravenous cannula situated in the tail vein. The presence and survival of the MSCs in the brain tissue was examined by immunohistochemistry. The rats were examined by their recovery of coordination of movement using both the Rotarod test and the adhesive removal test after the 1st, 2nd, 3rd and 4th week of stroke.
The results indicated that the MSC intrathecally receiving rats had an increased level of migrated cells to the ischemic area compared to the intravenous administration of MSCs. Additionally, many of the cells were expressing the mature neural lineage markers. Overall, the intrathecal administration of MSCs were more effective in reducing ischemic damage, yet proved to be similar to intravenous administration in promoting neurological recovery.
This study thus indicated a potential treatment for cerebral ischemia or neurodengerative disorders due to its ability to recover ischemic damaged tissue.