2017 Group Project 1
Abnormalities associated with Cerebral Cortex Development

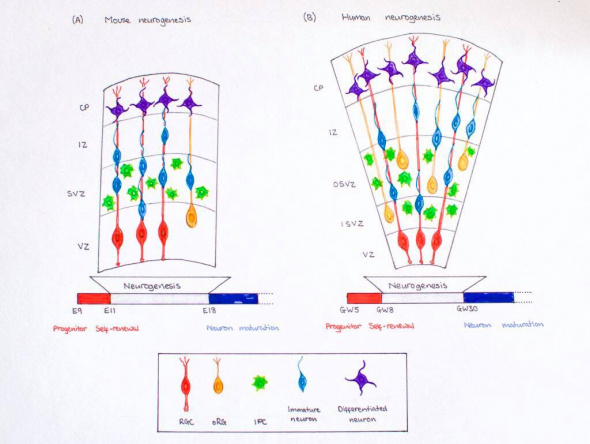
The embryologic development of the cerebral cortex involves highly organised and complex events (as has been seen in the section 'Development of the cerebral cortex').
These events are generally divided by scientists into 3 major stages in cortical formation where crucial changes occur in neuronal cells; these stages include:
1. Proliferation (or Growth),
2. Migration,
3. Organisation (or Maturation or Differentiation).
Disruptions in these stages of cortical development, are the precedent that give rise to malformations or irregularities in the cerebral cortex (Fig. ). This section will explore some abnormalities that are commonly discussed in scientific literature.
Disorders due to the abnormal proliferation, growth or differentiation of neuroblasts
1) Focal cortical dysplasia (FCD)
Focal cortical dysplasia (FCD) is heterogeneous developmental disorder of uncertain etiology. Focal Cortical Dysplasia is characterised by neurons arranged abnormally in the focal areas of the cerebral cortex as well as disorganisation of layers and very large cells called 'balloon' cells.
FCD can affect the areas throughout the brain but occurs dominantly in the frontal and temporal lobes of the cerebral cortex.
In all patients who present with epilepsy, FCD is the cause for about approximately 25% of them. FCD can be of two types: Type I and Type II.

2) Hemimegalencephaly
A rare congenital disorder that also results from the abnormal proliferation of neuroblasts is Hemimegalencephaly.
Hemimegalencephaly is a developmental disorder which consists of a 'hamartomatous' overgrowth (where normal mature cells and tissues normally present in an area of the body, form a tumour-like, benign malformation) on part or all of the cerebral hemisphere.
Hemimegalencephaly accounts for 0.2% of cases of childhood epilepsy. Clinical symptoms of this disease may include developmental delay, paralysis of one side of the body and blindness over half the field of vision; but the most significant symptom is seizures as 90% of patients present with this symptom.
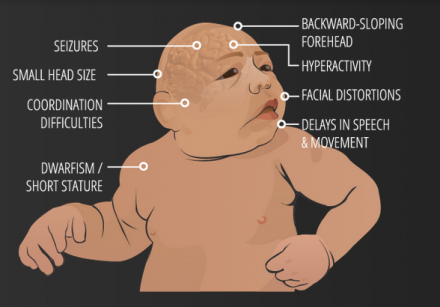
3) Microcephaly Vera
Microcephaly or 'small brain', can be caused by abnormal cell proliferation or cell division along with the involvement of other organs.
Primary Microcephaly or Microcephaly Vera results only due to abnormal cortical development, specifically cell division or proliferation. It is a congenital malformation in which the circumference of the head is quite less than normal and is accompanied by mental retardation and sometimes epilepsy.
References used to write: [1]
[3]
[4]
[5]
4) Tuberous Sclerosis Complex
Tuberous sclerosis complex (TSC) is a multi-organ disease resulting from mutations of certain genes, and is usually classified under defects of early cell proliferation and growth although it is also associated with defects of neuronal migration.
Tuberous sclerosis complex (TSC) is thus called due to lesions seen that resembled potato tubers; and is characterised by benign abnormal mass of cells (tumors, cysts, and other malformations including hamartomas and neoplasms) in the cortex.
" Beneath the cortex, the brain in tuberous sclerosis also shows nodular collections of small cells along the surface of the lateral ventricle that resemble ventricular cells and are called subependymal nodules...or, more descriptively, “candle drippings.” These nodules often contain numerous balloon cells and can in some cases become transformed into glial tumors referred to as subependymal giant cell astrocytomas..."
Disorders due to abnormal neuronal migration
5) Heterotopia
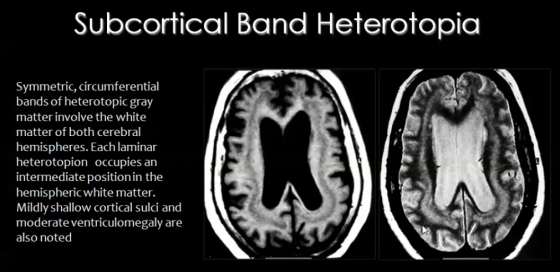
Migration of neurons occurs during the 8th week of development, along radial glial fibers (RGF). RGFs can be damaged due to ischemia, which can be caused by infection resulting from trauma or metabolic errors.
RGF damage leads to the migration process arresting at the wrong time, resulting in abnormal or ectopic locations of neurons of the cortex. This condition is known as Heterotopia.
There are different types of heterotopia:
- Subcortical band heterotopia:
In this type of heterotopia, ectopic locations of neurons, seen as nodules, occur in the sub-cortical regions of the cerebral cortex.
- Periventricular heterotopia/ sub-ependymal heterotopia:
In this type of heterotopia, ectopic locations of neurons, seen as nodules, occur in the sub-ependymal or periventricular area of gray matter of cerebral cortex.
- Focal heterotopia:
In this type of heterotopia, abnormal location of neurons result in focal masses within deep white matter of cerebral cortex.
6) Lissencephaly
Lissencephaly is a congenital cortex malformation, in which gyri (and sulci) of the cerebral cortex are absent (agyria) or largely absent (pachgyria), resulting in a smooth surface of the brain. The normal lamination or layers fail to form and the cerebral cortex usually has only 4 of the typical 6 layers. Like most congenital brain disorders, the etiology of Lissencephaly is uncertain.
Lissencephaly has also been associated with other abnormalities including corpus callosum hypoplasia, small brain stem and gray matter heterotopia.
Lissencephaly is generally characterised by the following features:
- Total agyria (gyri and sulci absent resulting in 'smooth brain')
- Pachygyria (gyri can be seen but are very few compared to normal brain)
- Agyric brain with areas of pachygyria
- Vertically oriented Sylvian fissures of the brain, giving the brain an 'hourglass' configuration
Lissencephaly is of different types; even so common clinical symptoms are 'epilepsy' and 'severe mental retardation'. Types of Lissencephaly are the following:
- Classical (Type I) Lissencephaly- results from neuronal undermigration (failed or incomplete neuronal migration) due to varying causes like mutation; additional clinical features include motor deficits. Patients often also have microcephaly [discussed later in Microlissencephaly].
- Cobblestone (Type II) lissencephaly- results from overmigration, where neurons migrate from the cortex into the overlying leptomeninges, causing diverse disruptions of the basement membrane; the cortex has a 'cobblestone' type of nodular appearance and additional clinical features include various eye abnormalities, congenital muscular dystrophies, hypotonia and generalized weakness in infancy.
Type II Lissencephaly also includes:
- Muscle-Eye-Brain Disease
- Walker-Warburg Syndrome
- Fukuyama Syndrome
- Microlissencephaly
Microlissencephaly occurs when Type I Lissencephaly occurs in combination with congenital Microcephaly, and presents with severe symptoms including seizures, spasticity, severe developmetal delay and short life span.
7) Kallmann Syndrome
The Kallman Syndrome is syndrome which results from the migration of neurons that secrete leuteinizing hormone-releasing hormone (LHRH) from the olfactory placode to the hypothalamus, causing congenital hypogonadism (since LHRH is necessary for normal gonadal function).
Kallman Syndrome is associated with hypoplasia of the olfactory bulbs and olfactory cortex, called arhinencephaly, and lack of the sense of smell. [not yet changed into own words]
Disorders due to abnormal cortical maturation and organization/folding
8) Polymicrogyria
If the neurons of the cerebral cortex successfully complete the proliferation and migration stages, but during the last organisation stage, distribute abnormally then multiple small undulating gyri can result. This condition is called Polymicrogyria (PMG), in which, the gyri become extremely small (hence the term micro) and their number is greater than normal. The cerebral cortex in this condition is flat and thickened, similar to that of pachygyria or agyria, and contains numerous small gyri.
Polymicrogyria is usually focal. It is most commonly 'perisylvian' (around the Sylvian fissure) and can be 'bilateral' or 'unilateral'. The most common sites, in descending order, are the frontal lobe, parietal lobe, temporal lobe and then occipital lobe.
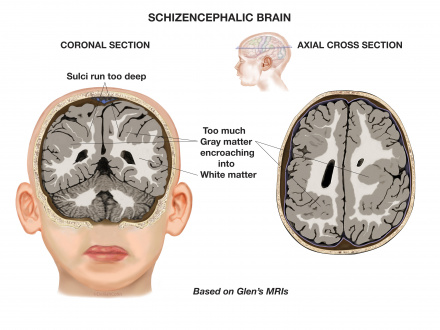
9) Schizencephaly
Schizencephaly is an organisational developmental disorder characterised by a cleft(s) or lesion(s) on the brain surface, which is filled with CSF and lined by gray matter. Schizencephaly can be bilateral or unilateral.
The clefts can be small with closed walls in Type I or Closed lip type schizencephaly; or the clefts can be large with free communication between the ventricle and subarachnoid spaces in Type II or Open lip type schizencephaly.
Schizencephaly commonly involves the parasylvian regions, and severity of the disease correlates with the extent of the clefts.
Other Disorders
12) Fetal Alcohol Spectrum Disorder (FASD)

Fetal Alcohol Spectrum Disorder (FASD) refers collectively to the malformations that occur in children due to maternal alcohol consumption during pregnancy. This results from the effects of ethanol as it crosses the placental barrier. The mechanism for these abnormalities developing is complicated and not entirely clear, but various studies show that ethanol disrupts all major processes of fetal CNS development and causes toxicity of blood (as fetal liver cannot yet detoxify ethanol well).
The three major indications (that also help form the diagnoses) for FASD are facial dysmorphology, growth deficits and central nervous system defects. These conditions result in immense physiological and psychological impacts on the child. Fetal Alcohol Syndrome (FAS) is an acute form of FASD.
On average, FASD is diagnosed in a child between 3-10 years. It is of utmost importance however that the diagnosis is done as early as possible so that timely interventions could be taken in order to lessen the severity of the symptoms that result from this syndrome.
[8]
13) Corpus Callosum Agenesis
<html5media height="320" width="520">https://www.youtube.com/watch?v=7zOa3LLrHKc</html5media>
[9]
- ↑ 1.0 1.1 1.2 1.3 Mahfouz, M. (2015). Imaging of cortical formation disorders - DRE 4 - Prof. Dr Mamdouh Mahfouz. [video] Available at: https://www.youtube.com/watch?v=l_nTggR7LTE [Accessed 23 Sep. 2017].
- ↑ USDA & Felipe Dana/AP and Creative Commons License(CC) (2017). Understanding Zika. [online] Goinvo.com. Available at: http://www.goinvo.com/features/zika/ [Accessed 4 Oct. 2017].
- ↑ Squier, W. and Jansen, A. (2010). Abnormal development of the human cerebral cortex. Journal of Anatomy, [online] 217(4), pp.312-323. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2992410/ [Accessed 23 Sep. 2017].
- ↑ Pang, T., Atefy, R. and Sheen, V. (2008). Malformations of Cortical Development. The Neurologist, [online] 14(3), pp.181-191. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3547618/ [Accessed 23 Sep. 2017].
- ↑ Christopher A, C. (2017). Genetic Malformations of the Human Cerebral Cortex. Neuron, [online] 23(1), pp.19 - 29. Available at: http://www.cell.com/neuron/fulltext/S0896-6273(00)80749-7?_returnURL=http%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0896627300807497%3Fshowall%3Dtrue [Accessed 23 Sep. 2017].
- ↑ PRWeb (2013). Schizencephalic Brain. [image] Available at: http://www.prweb.com/releases/2013/7/prweb3350774.htm [Accessed 5 Oct. 2017].
- ↑ MarkHill,embryology.med.unsw.edu.au (2017). Facial Appearance of Fetal Alcohol Syndrome (FAS). [image] Available at: https://embryology.med.unsw.edu.au/embryology/index.php/File:FASface.jpg [Accessed 5 Oct. 2017].
- ↑ Leigland, L., Ford, M., Lerch, J. and Kroenke, C. (2013). The Influence of Fetal Ethanol Exposure on Subsequent Development of the Cerebral Cortex as Revealed by Magnetic Resonance Imaging. Alcoholism: Clinical and Experimental Research, 37(6), pp.924-932. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3670687/ [Accessed 5 Oct. 2017].
- ↑ Ezzo - Izzo, D. (2007). How the Body Works : The Corpus Callosum. [video] Available at: https://www.youtube.com/watch?v=7zOa3LLrHKc [Accessed 23 Sep. 2017].
- ↑ dimedcom (2013).Corpus callosum agenesis. [video] Available at: https://www.youtube.com/watch?v=M7e9JXGOWD4 [Accessed 6 Oct. 2017].