Endocrine - Thyroid Development
Introduction
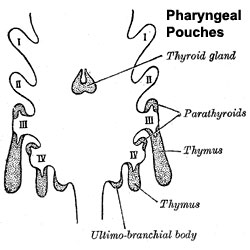
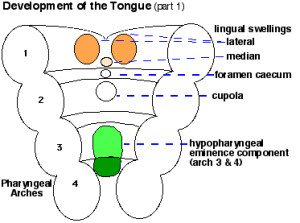
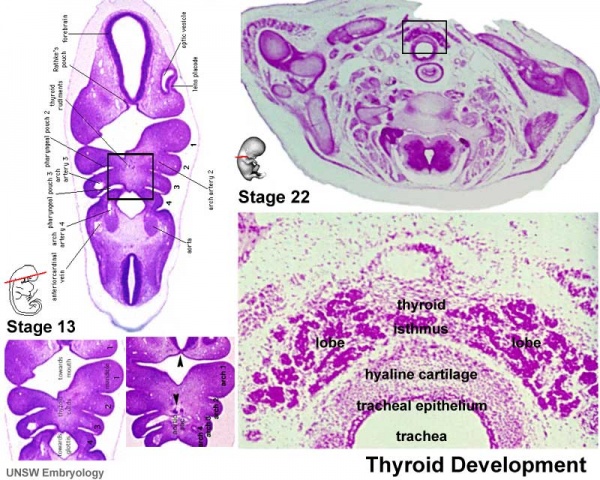
The boundary endoderm in the floor region forms a pocket (marked by the foramen cecum) that separates from the surface and forms the thyroid. Cells originate on the surface of the floor and descend into mesoderm above aortic sac and into the hypopharyngeal eminence as "cords". These cells continue to descend until they reach their final destination in the neck adjacent to the thyroid cartilage.
This pathway forms a temporary duct (thyroglossal duct). There are abnormalities of incomplete or excessive descent of these thyroid precursor cells. The thyroid is one of the earliest endocrine organs to differentiate and has an important hormonal role in embryonic development. The early bundle of cells then forms the thyroid by first dividing to form 2 lobes separated by a narrow connecting isthmus.
- Functions from wk10 - required for neural development, stimulates metabolism (protein, carbohydrate, lipid), reduced/absence = cretinism (see abnormalities)
- Hormones - (amino acid derivatives) Thyroxine (T4), Triiodothyronine (T3)
| Lecture - Head Development | original page
Some Recent Findings
|
Reading
- Human Embryology (2nd ed.) Larson
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Ch10: p230-233, Ch12: p280-282, Ch13: p319-347
- Before We Are Born (5th ed.) Moore and Persaud
- Essentials of Human Embryology Larson
- Human Embryology Fitzgerald and Fitzgerald Ch24: p166-167
Development Overview
|
|
| Foramen Caecum | Stage 13 and Stage 22 thyroid development |
- thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- tongue grows, cells descend in neck
- thyroglossal duct - proximal end at the foramen cecum of tongue thyroglossal duct
- thyroid diverticulum - hollow then solid, right and left lobes, central isthmus
Thyroid Timeline
- 24 days - thyroid median endodermal thickening in the floor of pharynx, outpouch – thyroid diverticulum
- Week 11 - colloid appearance in thyroid follicles, iodine and thyroid hormone (TH) synthesis
growth factors (insulin-like, epidermal) stimulates follicular growth
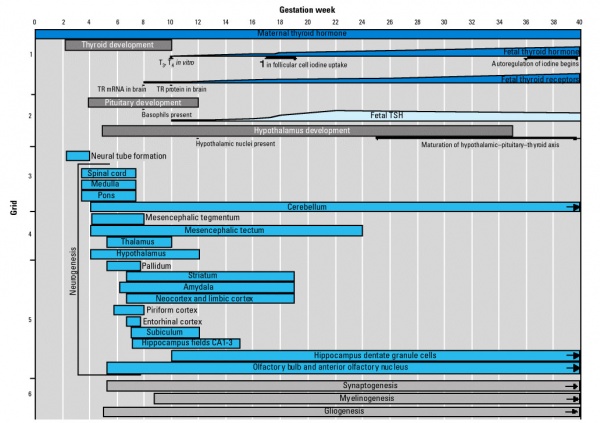
Thyroid System and Neural Development
Fetal Thyroid Hormone
- Initial secreted biologically inactivated by modification, late fetal secretion develops brown fat
- Iodine deficiency- during this period, leads to neurological defects (cretinism)
- Birth - TSH levels increase, thyroxine (T3) and T4 levels increase to 24 h, then 5-7 days postnatal decline to normal levels
Thyroid Hormone
Thyroid hormone is synthesized in the thyroid gland by the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin.
Thyroxine (T4) - (Mr 777) majority of thyroid hormone derived from the thyroid gland. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood.
Triiodothyronine (T3) - synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4), though T3 is mainly used by tissues. Derived mainly from peripheral monodeiodination of T4 (at the 5' position of the outer ring of the iodothyronine nucleus).
(Data: PubChem)
Deiodinases
A group of enzymes that can modify the thyroid prohormone secreted by the thyroid gland either activating (deiodinase 2) or deactivating (deiodinase 3) thyroid hormone. Their role is thought to regulate the amount of active hormone available locally in a tissue.
- Deiodinase 2 (Dio2) A deiodinating enzyme that activates thyroid hormone by clipping the 5'-iodine off of the T4 prohormone to create T3, which is the preferred ligand for thyroid receptors. The enzyme has 5'- outer ring (5'-) catalytic activity.
- Deiodinase 3 (Dio3) A deiodinating enzyme that inactivates thyroid hormone by removing the 5-iodine from either the T4 prohormone or the T3 active hormone. The enzyme has 5- inner ring (5-) catalytic activity.
Links: PubChem - T4 | PubChem - T3 |
Maternal Thyroid
Maternal thyroid related changes during pregnancy[3]:
- stimulation of maternal thyroid gland by elevated levels of human chorionic gonadotropin (hCG)
- occurs mainly near end of first trimester associated with a transient lowering in serum TSH
- increase in serum thyroxine-binding globulin levels
- small decrease in free hormone concentrations (in iodine-sufficient conditions) significantly amplified in iodine restriction or overt iodine deficiency
- trend toward a slight increase in basal thyrotropin (TSH) values between first trimester and term
- modifications of the peripheral metabolism of maternal thyroid hormones
Abnormalities
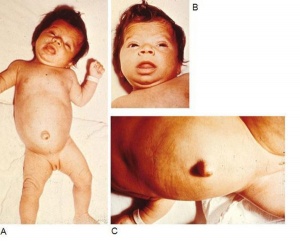
- Congenital hypothyroidism - approximately 1 in 3000 births, associated with neurological abnormalities.
- Lingual thyroid gland - failure of thyroid descent.
- Thyroglossal cyst - persistance of thyroglossal duct.
- Thyroglossal fistula - partial degeneration of the thyroglossal duct.
- Abnormal development of the thyroid - incomplete or excessive descent.
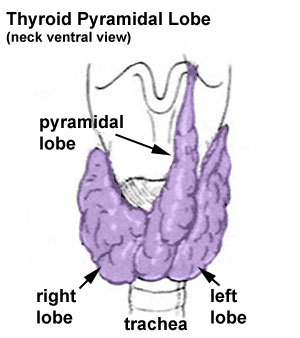
- Pyramidal lobe - from isthmus (50% of people) attached to hyoid bone distal end of thryoglossal duct.
- Childhood hypothyroidism - delays ossification and bone mineralization.
Congenital Hypothyroidism
This abnormality can occur through either dysgenesis or agenesis of the thyroid gland development or abnormal thyroid hormone production. The condition can be classified as a permanent and transient form.
American Academy of Pediatrics 2006 - Update of newborn screening and therapy for congenital hypothyroidism[5] "Unrecognized congenital hypothyroidism leads to mental retardation. Newborn screening and thyroid therapy started within 2 weeks of age can normalize cognitive development. The primary thyroid-stimulating hormone screening has become standard in many parts of the world. However, newborn thyroid screening is not yet universal in some countries. Initial dosage of 10 to 15 microg/kg levothyroxine is recommended. The goals of thyroid hormone therapy should be to maintain frequent evaluations of total thyroxine or free thyroxine in the upper half of the reference range during the first 3 years of life and to normalize the serum thyroid-stimulating hormone concentration to ensure optimal thyroid hormone dosage and compliance. Improvements in screening and therapy have led to improved developmental outcomes in adults with congenital hypothyroidism who are now in their 20s and 30s. Thyroid hormone regimens used today are more aggressive in targeting early correction of thyroid-stimulating hormone than were those used 20 or even 10 years ago. Thus, newborn infants with congenital hypothyroidism today may have an even better intellectual and neurologic prognosis."
Iodine Deficiency
Iodine deficiency disorder (IDD) is the single most common cause of preventable mental retardation and brain damage in the world (More? Abnormal Development - Iodine Deficiency). It is required for synthesis of thyroid hormone, which in turn regulates aspects of neural development.
Worldwide:
1.6 billion people are at risk IDD affects 50 million children 100,000 cretins are born every year It causes goiters and decreases the production of hormones vital to growth and development. Children with IDD can grow up stunted, apathetic, mentally retarded and incapable of normal movement, speech or hearing. IDD in pregnant women cause miscarriage, stillbirth and mentally retarded children.
A teaspoon of iodine is all a person requires in a lifetime, but because iodine cannot be stored for long periods by the body, tiny amounts are needed regularly. In areas of endemic iodine deficiency, where soil and therefore crops and grazing animals do not provide sufficient dietary iodine to the populace, food fortification and supplementation have proven highly successful and sustainable interventions.
Iodized salt programs and iodized oil supplements are the most common tools in the fight against IDD.
(Data: ICCIDD)
Prolonged intake of large amounts (excess) of iodide can increase the incidence of goiter and/or hypothyroidism in humans. African Congo appears to be the only country that appears to have a dietary excess.
Maternal Abnormalities
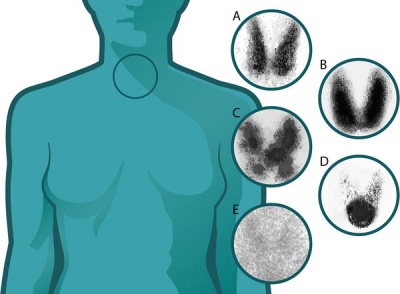
(A) Normal
(B) Graves disease: diffuse increased uptake in both thyroid lobes.
(C) Toxic multinodular goiter (TMNG): "hot" and "cold" areas of uneven uptake.
(D) Toxic adenoma: increased uptake in a single nodule with suppression of the surrounding thyroid.
(E) Thyroiditis: decreased or absent uptake.
Thyroid uptake scans image[6] Maternal Graves Disease - "The dose of anti-thyroid drug usually needs to be decreased during pregnancy, and often Graves disease remits completely and the medication can be withdrawn. This is probably due to the overall immunosuppressive effect of pregnancy."
Graves' disease in mothers can cause thyrotoxic fetus - may have increased fetal motility and develop a range of abnormalities including: goitre, tachycardia, heart failure associated hydrops, growth retardation, craniosynostosis and accelerated bone maturation.
Maternal Hashimoto's Thyroiditis (common autoimmune thyroid disease) usually no consequences on fetal thyroid, even if antibodies (anti-TPO and anti-Tg) found in the newborn due to transplacental passage.
maternal hypothyroxinemia
Links: NIH Genes & Disease - Chapter 41 - Endocrine | EPA (USA) - Radiation Technetium
Environmental Thyroid Disruptors
There are several environmental compounds (chemicals) that are suspected of being thyroid disruptors including:
- halogenated phenolic compounds (3,3',5,5'-tetrabromobisphenol A, 3,3',5,5'-tetrachlorobisphenol A, 4-hydroxy-2',3,4',5,6'-pentachlorobiphenyl)
- phenol compounds (pentachlorophenol, 2,4,6-triiodophenol)
They have been demonstrated to induce partial agonistic and/or complex competitive/uncompetitive antagonistic responces in cell culture.
Bisphenol A - monomer used to manufacture polycarbonate plastic, possibly disrupts thyroid hormone function and affects neocortical development (accelerating neuronal differentiation/migration). (More? EHP - Bisphenol A Need for a New Risk Assessment)
Genes
Thyroid Transcriptor Factors (TTF) - TTF-1, TTF-2, PAX-8
Fetal hypothyroidism from low levels of these transcription factors- Pit-1, Prop-1, LHX-3
Thyrotropin-releasing hormone (TRH)
Thyroid-stimulating hormone (TSH)
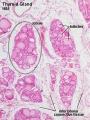
Thyroid Histology
Adult
References
- ↑ <pubmed>19389367</pubmed>
- ↑ <pubmed>19088150</pubmed>
- ↑ What happens to the normal thyroid during pregnancy? Glinoer D. Thyroid. 1999 Jul;9(7):631-5. Review. PMID: 10447005
- ↑ <pubmed>20537182</pubmed>| Orphanet J Rare Dis.
- ↑ <pubmed>16740880</pubmed>
- ↑ <pubmed>16363909</pubmed>
Journals
- Thyroid Thyroid The official journal of the [%20http://www.thyroid.org/ American Thyroid Association].
Online Textbooks
Endocrinology: An Integrated Approach Nussey, S.S. and Whitehead, S.A. Oxford, UK: BIOS Scientific Publishers, Ltd; 2001. table of Contents
- The Thyroid Gland
- Surgical anatomy and embryology of the thyroid gland
- Hypothyroidism in infancy and childhood
NIH Genes & Disease Chapter 41 - Endocrine
Developmental Biology (6th ed) Gilbert, Scott F. Sunderland (MA): Sinauer Associates, Inc.; c2000.
- Is the endostyle the precursor of the thyroid gland?
- Environmental thyroid hormone disruptors
- table 13.1. Some derivatives of the neural crest
Molecular Biology of the Cell (4th Edn) Alberts, Bruce; Johnson, Alexander; Lewis, Julian; Raff, Martin; Roberts, Keith; Walter, Peter. New York: Garland Publishing; 2002.
Health Services/Technology Assessment Text (HSTAT) Bethesda (MD): National Library of Medicine (US), 2003 Oct. Thyroid Gland search Results
Reviews
<pubmed>12432093</pubmed> <pubmed>15863666</pubmed> <pubmed>15231702</pubmed> <pubmed>12566717</pubmed>
Articles
<pubmed>16093324</pubmed> <pubmed>10902817</pubmed>
Search PubMed
Search April 2010
- Endocrine Development - All (14277) Review (4620) Free Full Text (3140)
Search Pubmed: thyroid development
Additional Images
Adult Histology
Terms
External Links
- International Council for the Control of Iodine Deficiency Disorders
- World Health Organization- Micronutrient deficiencies Eliminating iodine deficiency disorders
- British Thyroid Association The official site of the British Thyroid Assocation, a non-profit making Learned Society of professional clinical specialist doctors and scientists in the United Kingdom who manage patients with thyroid disease and/or are researching into the thyroid and its diseases in humans.
- WHO Nutrition Guidelines
- American Thyroid Association American Thyroid Association - Patient Information
- Thyroid Foundation of America
- Endocrine Society (USA)
- European Thyroid Association
- Latin-American Thyroid Association
- [www.aota.or.kr Asia and Oceana Thyroid Association]
- Society for Endocrinology (UK)
- British Association of Endocrine Surgeons
- [www.aace.com American Association of Clinical Endocrinologists]
- Thyroid Disease Manager USA -- this site includes textbook on the Thyroid.
- [www.synthroid.com Knoll Pharmaceuticals]- makers of SYNTHROID
- Gray's Anatomy - The Ductless Glands | The thyroid gland and its relations | Floor of pharynx of human embryo about twenty-six days old. (From model by Peters) | 4b. The Parathyroid Glands
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, June 3) Embryology Endocrine - Thyroid Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Endocrine_-_Thyroid_Development
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G