Vagina Development: Difference between revisions
| Line 9: | Line 9: | ||
Acién's hypothesis - relates to abnormalities and the embryology of the human vagina as deriving from the Wolffian ducts and the Müllerian tubercle. | Acién's hypothesis - relates to abnormalities and the embryology of the human vagina as deriving from the Wolffian ducts and the Müllerian tubercle. | ||
{{Template:Genital Links}} | [[Development_Animation_-_Uterus|Uterus Development Animation]] | [http://embryology.med.unsw.edu.au/Notes/genitalXXuterus.htm original page] | |||
==Background Reading== | ==Background Reading== | ||
Revision as of 20:09, 3 May 2010
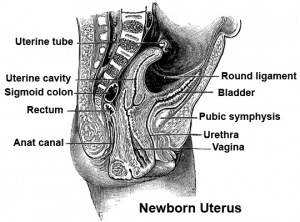
Introduction
The embryonic origin of the vagina has been a historically hotly debated issue with several different contributions and origins described.
One description shows the vagina arising by downward growth of Wolffian and Mullerian ducts. The sinovaginal bulbs are the caudal ends of the Wolffian ducts. Vaginal development is also under negative control of androgens.
An earlier understanding was that the upper part of the vagina derived from Müllerian ducts and the lower part from the sinovaginal bulbs (formed by fusion form the vaginal plate) all derived from the urogenital sinus. The terms sinovaginal bulbs and vaginal plate were first coined by Koff in 1933.[1]
Acién's hypothesis - relates to abnormalities and the embryology of the human vagina as deriving from the Wolffian ducts and the Müllerian tubercle.
| Uterus Development Animation | original page
Background Reading
Search PubMed: Vagina Development | Mullerian ducts
- The development of the human vagina. BULMER D. J Anat. 1957 Oct;91(4):490-509. No abstract available. PMID: 13475148 | PMCID: 1244904
- New concepts on the development of the vagina. Shapiro E, Huang H, Wu XR. Adv Exp Med Biol. 2004;545:173-85. Review. No abstract available. PMID: 15086027
- Revisiting old vaginal topics: conversion of the Müllerian vagina and origin of the "sinus" vagina. Cai Y. Int J Dev Biol. 2009;53(7):925-34. Review. PMID: 19598112 | IJDB
- "Vaginal development has been a longstanding controversy, which hampers studies on vaginal diseases as well as cervical and uterine diseases. Most concerns center on: why is the vaginal epithelium different from the uterine epithelium; and where does the vagina originate from? It is commonly held that the rodent vagina has a dual origin: the cranial part is derived from the Mullerian duct (Mullerian vagina) and the caudal part derived from the urogenital sinus (sinus vagina). This concept was deduced from morphological observations. However, it cannot explain the difference between the Mullerian vagina and the uterus. Moreover, accumulating new data from genetic and molecular studies contradicts the urogenital sinus origin of the sinus vagina. The present review summarizes previous morphological observations and new findings from genetic and molecular studies, and addresses molecular mechanisms underlying the origin and organogenesis of the vagina in rodents. It provides evidence to show that the whole vagina is derived the Mullerian duct. BMP4 reshapes the intermediate mesoderm-derived Mullerian duct into the vaginal primordium. The latter thus exhibits different features from the uterus, including the stratified squamous epithelium and insensitivity to anti-Mullerian hormone. The sinus vagina is formed by extrinsic BMP4-mediated caudal extension of the Mullerian duct. The present review thus shows how a century of controversy over the origin and organogenesis of the vagina has been resolved. This new understanding will provide additional insight into genetic diseases and tumors of the female reproductive tract."
- Fetal development of the female external urinary sphincter complex: an anatomical and histological study. Sebe P, Fritsch H, Oswald J, Schwentner C, Lunacek A, Bartsch G, Radmayr C. J Urol. 2005 May;173(5):1738-42; discussion 1742. PMID: 15821572
- Helper function of the Wolffian ducts and role of androgens in the development of the vagina. Drews U. Sex Dev. 2007;1(2):100-10. PMID: 18391520
- "Here experiments with the complete androgen receptor defect in the testicular feminisation (Tfm) mouse are reported which show that the vagina is formed by caudal migration of Wolffian and Müllerian ducts. The cranial ends of the Wolffian ducts successively regress while the Müllerian ducts fuse to form the vagina. Immunohistochemistry of the androgen receptor reveals that the caudal ends of the Wolffian ducts remain in the indifferent stage and therefore have been mistaken as sinuvaginal bulbs. The Wolffian ducts do not contribute to the vagina itself but have a helper function during downward movement of the vaginal bud in the female. In the male the caudal ends serve as androgen operated switch for the negative control of vaginal development. The results indicate that the rudimentary vagina in the complete androgen insensitivity syndrome (CAIS) corresponds to non obliterated caudal ends of the Müllerian ducts. Selective atresia of the vagina in the MRKH (Mayer-Rokitansky-Kuster-Hauser) syndrome may be explained by the failure of Wolffian and Müllerian ducts to descend caudally"
- Lifetime changes in the vulva and vagina. Farage M, Maibach H. Arch Gynecol Obstet. 2006 Jan;273(4):195-202. Epub 2005 Oct 6. Review. PMID: 16208476
- "The morphology and physiology of the vulva and vagina change over a lifetime. The most salient changes are linked to puberty, the menstrual cycle, pregnancy, and menopause. The cutaneous epithelia of the mons pubis, labia, and clitoris originate from the embryonic ectoderm and exhibit a keratinized, stratified structure similar to the skin at other sites. The mucosa of the vulvar vestibule, which originates from the embryonic endoderm, is non-keratinized. The vagina, derived from the embryonic mesoderm, is responsive to estrogen cycling. At birth, the vulva and vagina exhibit the effects of residual maternal estrogens. During puberty, the vulva and vagina acquire mature characteristics in a sequential fashion in response to adrenal and gonadal maturation. A trend to earlier pubertal onset has been observed in Western developed countries. In women of reproductive age, the vaginal mucosa responds to steroid hormone cycling, exhibiting maximal thickness and intracellular glycogen content at mid-cycle. Vulvar skin thickness remains unchanged but menstrual cycle-associated changes in ortho- and parakeratosis occur at the cytological level. The vulva and vagina further adapt to the needs of pregnancy and delivery. After menopause, tissue atrophy ensues. Post-menopausal changes in skin barrier function, skin hydration, and irritant susceptibility have been observed on exposed skin but not on the vulva. Nevertheless, older women with incontinence are at increased risk for developing incontinence dermatitis. A combination of factors, such as tissue atrophy, slower dissipation of excess skin hydration, shear forces associated with limited mobility, and lower tissue regeneration capacity increase the risk of morbidity from incontinence dermatitis in older women."
Adult Dimensions
A recent study using magnetic resonance imaging (MRI) has accurately measured the dimensions of the adult vagina.[2]
- "Seventy-seven MRI scans were performed on 28 women before gel application to establish baseline vaginal measurements. Average dimensions were calculated for each woman and for the population. The influence of potential covariates (age, height, weight and parity) on these dimensions was assessed. ...Mean vaginal length from cervix to introitus was 62.7 mm. Vaginal width was largest in the proximal vagina (32.5 mm), decreased as it passed through the pelvic diaphragm (27.8 mm) and smallest at the introitus (26.2 mm)."
References
- ↑ Development of the vagina in the human fetus. Koff AK. Contrib Embryol. 1933 Sep;24(140):59-91. PMID: 12332362
- ↑ Baseline dimensions of the human vagina. Barnhart KT, Izquierdo A, Pretorius ES, Shera DM, Shabbout M, Shaunik A. Hum Reprod. 2006 Jun;21(6):1618-22. Epub 2006 Feb 14. PMID: 16478763
Reviews
- Lifetime changes in the vulva and vagina. Farage M, Maibach H. Arch Gynecol Obstet. 2006 Jan;273(4):195-202. PMID: 16208476
Kavlock R, Cummings A [See Related Articles] Function of sexual glands and mechanism of sex differentiation. J Toxicol Sci. 2004 Aug;29(3):167-78. Review.
Articles
- Essential roles of mesenchyme-derived beta-catenin in mouse Mullerian duct morphogenesis. Deutscher E, Hung-Chang Yao H. Dev Biol. 2007 May 3; PMID: 17532316
- Guioli S, Sekido R, Lovell-Badge R. The origin of the Mullerian duct in chick and mouse. Dev Biol. 2007 Feb 15;302(2):389-98.
- Hashimoto R. Development of the human Mullerian duct in the sexually undifferentiated stage. Anat Rec A Discov Mol Cell Evol Biol. 2003 Jun;272(2):514-9.
- The embryologic development of the human vagina. Ulfelder H, Robboy SJ. Am J Obstet Gynecol. 1976 Dec 1;126(7):769-76. PMID: 1033667
Search PubMed
Search Pubmed: Uterus Development
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, June 2) Embryology Vagina Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Vagina_Development
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G