User:Z3463890: Difference between revisions
No edit summary |
No edit summary |
||
| Line 152: | Line 152: | ||
'''Omphalocele''' is a rare birth defect that occurs every 1 in 4000 ~ 7000 live births worldwide. Babies with this problem are born with their visceral organs, mainly the liver, and intestine inside a thin membrane sac known as the omphalocele sac external of their abdominal cavity into the base of the umbilical cord. Technically, it is a herniation of the umbilicus. It is an abnormality in the development of the gastrointestinal system at around week 9~12 of fetal development.It occurs when lateral unfolding of the embryo fails for some reason, leading to the formation of an omphalocele. The organs are placed inside the abdominal cavity through surgery, usually within the first half year of the child being born <ref>CDC - Birth Defects, Facts about Omphalocele, [ http://www.cdc.gov/ncbddd/birthdefects/omphalocele.html ], Friday June 8, 2015 </ref> ,<ref> Omphalocele | Birth Anomalies | Prognosis & Treatment, [ http://www.cincinnatichildrens.org/health/o/omphalocele/ ], Friday June 8, 2015 </ref> . | '''Omphalocele''' is a rare birth defect that occurs every 1 in 4000 ~ 7000 live births worldwide. Babies with this problem are born with their visceral organs, mainly the liver, and intestine inside a thin membrane sac known as the omphalocele sac external of their abdominal cavity into the base of the umbilical cord. Technically, it is a herniation of the umbilicus. It is an abnormality in the development of the gastrointestinal system at around week 9~12 of fetal development.It occurs when lateral unfolding of the embryo fails for some reason, leading to the formation of an omphalocele. The organs are placed inside the abdominal cavity through surgery, usually within the first half year of the child being born <ref>CDC - Birth Defects, Facts about Omphalocele, [ http://www.cdc.gov/ncbddd/birthdefects/omphalocele.html ], Friday June 8, 2015 </ref> ,<ref> Omphalocele | Birth Anomalies | Prognosis & Treatment, [ http://www.cincinnatichildrens.org/health/o/omphalocele/ ], Friday June 8, 2015 </ref> . | ||
Children born with this defect often have other abnormalities, often chromosomal such as a | Children born with this defect often have other abnormalities, often chromosomal such as a Trisomy at pair 13, 18 or 21. It is unknown the causes of this birth defect; some investigation have suggested maternal age, multiple pregnancies, and number of births may increase the chance of a child being born with an omphalocele, but there are also many studies that do not agree with this. It is thought that smoking, consumption of alcohol, and not enough dietary foliate in the mother may contribute to this birth defect.The survival rate for children born with just an omphalocele and do not have any other health problems is 90%.A woman carrying a fetus with omphalocele often have high levels of alpha-fetoprotein in her body. Blood testing, detailed fetal ultrasound, ultra-fast fetal MRI and a fetal echocardiogram can lead to early diagnosis of a omphalocele whilst in the fetal stage, and in many cases where it is legal, the pregnancy is terminated <ref><pubmed>13989758</pubmed></ref> , <ref><pubmed>13303095</pubmed></ref>. | ||
BUT '''Gastrochisis''' is a development abnormality of the anterior abdominal wall, where the bowel protrudes without a covering sac between the developing rectus muscles, occurring slightly lateral and towards the right of the fetal umbilicus. Gastrochisis commonly occurs as an isolated malformation, occurring in approximately 2.5 in 10’000 births <ref><pubmed>19419415</pubmed></ref>. | BUT '''Gastrochisis''' is a development abnormality of the anterior abdominal wall, where the bowel protrudes without a covering sac between the developing rectus muscles, occurring slightly lateral and towards the right of the fetal umbilicus. Gastrochisis commonly occurs as an isolated malformation, occurring in approximately 2.5 in 10’000 births <ref><pubmed>19419415</pubmed></ref>. | ||
During the | During the 4th week of normal fetal development, the lateral body of the fetus folds, moving ventrally and fusing in the midline to form the anterior body wall. It has been suggested that the incomplete fusion of the midline results in this abnormality, resulting in the abdominal viscera to protrude through the abdominal wall, herniating through the rectus muscle. This is one of the many theories related to Gastrochisis as the cause is still unclear. Other theories include, the failure of mesoderm to form in the body wall, rupture of the amnion around the umbilical ring with subsequent herniation of the bowel, abnormal involution of the right umbilical vein resulting in a weakening of the body wall and thus resulting in herniation of the bowel, and disruption of the right vitelline (yolk sac) artery with consequent body wall damage and gut herniation <ref><pubmed>25059025</pubmed></ref> , <ref><pubmed>17230493</pubmed></ref> . | ||
Revision as of 14:57, 6 September 2015
Lab Attendance
--Z3463890 (talk) 13:46, 7 August 2015 (AEST)
--Z3463890 (talk) 12:51, 14 August 2015 (AEST)
--Z3463890 (talk) 12:04, 21 August 2015 (AEST)
--Z3463890 (talk) 12:05, 28 August 2015 (AEST)
--Z3463890 (talk) 12:44, 4 September 2015 (AEST)
Lab Assessment 1
Article 1
"Effect of vitamin D status on clinical pregnancy rates following in vitro fertilization" [1] PMID 25077107
Summary
According to this study, vitamin D may play a role in human reproduction. Therefore, the aim of this study was to find out whether there is a correlation between vitamin D levels and implantation and clinical pregnancy rates in infertile women following IVF.
Method
• Total of 173 infertile women participated in the study that met the following criteria: aged 18-41 years, follicle stimulating hormone level 12 IU/L or lower and able to provide informed consent.
• 25(OH)D samples were collected within 1 week before oocyte retrieval from those infertile women.
• Vitamin D status was evaluated and determined by serum 25-hydroxy-vitamin D (25[OH]D) levels.
• Patients were classified in two different groups; having sufficient (≥ 75 nmol/L) or insufficient (or deficient; hereafter referred to as “insufficient”; < 75 nmol/L) serum levels of 25(OH)D.
• Patient demographics and IVF cycle parameters between two groups were compared.
• Clinical pregnancy, as identified by ultrasound following 4-5 weeks after embryo transfer; was the primary outcome measurement.
Findings
According to the outcome of this study, the women with sufficient levels of 25(OH)D had significantly higher rates of clinical pregnancy (52.5%) per IVF cycle started than that with insufficient levels (34.7%). Therefore, Vitamin D supplementation can potentially provide an easy and cost-effective way of improving pregnancy rates but requires further investigations as the results are not statistically significant in the sufficient 25(OH)D group.
Article 2
"Examining the temperature of embryo culture in in vitro fertilization: a randomized controlled trial comparing traditional core temperature (37°C) to a more physiologic, cooler temperature (36°C)." [2] PMID 25044079
The aim of this study was to illustrate the better clinical outcome of blastulation and pregnancy rates in human clinical IVF in a more physiologically cooler temperature i.e. 36°C, compare to the traditional core temperature of 37 degrees Celsius.
Method
• 52 Infertile couples with a female partner less than 42 years old were selected for this study.
• 8 or more oocytes from a female of 42 years of age, with infertile couples (n=52) were retrieved.
• Mature oocytes obtained from a single cohort of oocytes were randomly divided into two groups. One group was cultured at 37°C and the other at 36°C. These conditions kept as it is from the time of intracytoplasmic sperm injection (ICSI) until the time of verification (embryo transfer).
• Paired embryo transfers were done by transferring an euploid embryo from both group.
• DNA fingerprinting was used to determine the outcome for each embryo.
It is important to note that, some factors were measured throughout the study to measure the main outcomes and highlight which of these conditions clinically improved the embryonic development. These factors are: rate of development of expanded blastocysts, fertilization, aneuploidy, and sustained implantation.
Findings
According to this investigation, paired analysis shows a slightly higher usable rate of blastocyst formation per zygote at the 37°C environment (48.4%), compare to the other group at the 36°C culture (41.2%). Rates of fertilization, aneuploidy, and sustained implantation were equivalent. In conclusion, IVF culture at 36 degrees does not improve the conditions for blastulation and pregnancy rates in human in IVF. Thus, keeping the traditional temperature or decreasing it to 36 degrees does not have any advantages to embryo development .
References
Lab 2 - Images
| Uploading Images in 5 Easy Steps | ||
|---|---|---|
First Read the help page Images and Copyright Tutorial.
Students cannot delete images once uploaded. You will need to email me with the full image name and request deletion, that I am happy to do with no penalty if done before I assess. Non-Table version of this page
|
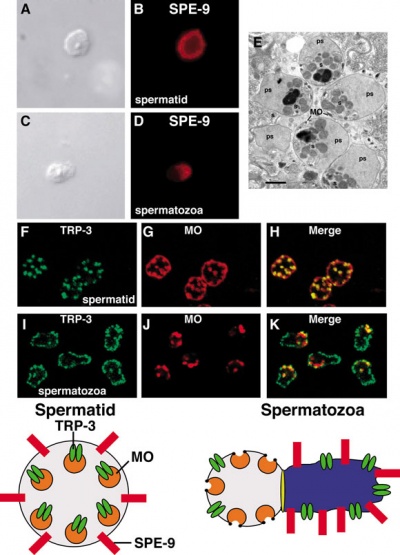
Image showing Dynamic Localization of Two Membrane Proteins Required for Fertilization[1]
- ↑ <pubmed>18050412</pubmed>
Lab 3-research/review articles
[Oncofertility and breast cancer: Where have we come from, where are we going?].
<pubmed>25991386</pubmed>
This article focuses on the current context of national and international recommendations, techniques development to evaluate and preserve fertility and patients' claims, this study aims to make a survey about the management of patients' breast cancer regarding oncofertility. This article concludes that , in order to satisfy patients' requests, several improvements have to be made regarding the patients' information, the health professionals' awareness and care coordination.I don't go through it now but very interesting article to read and useful for our group project.
Emergency fertility preservation for female patients with cancer: clinical perspectives.
<pubmed>26026071</pubmed>
This article explains about clinical perspectives to explore the new as well as the currently available options and strategies that can be used for emergency fertility preservation of female cancer patients.Such options include emergency ovarian stimulation, embryo freezing, egg freezing, ovarian tissue freezing and autotransplantation, in vitro maturation, and ovarian protection techniques. This article also mentions the advantages and disadvantages of each option as well as a new comprehensive multi-step strategy for these situations.
Sexual dysfunction and infertility as late effects of cancer treatment
<pubmed>26217165</pubmed>
As all we know, Sexual dysfunction is the main consequence of cancer treatment. Problems are usually linked to damage to nerves, blood vessels, and hormones that underlie normal sexual function. This article emphasizes on these sexual dysfunction and does in depth. It addresses that innovations in cancer treatment such as robotic surgery or more targeted radiation therapy have not had the anticipated result of reducing sexual dysfunction. Therefore, advances in both technologies and in knowledge about how cancer treatments can damage fertility, offer hope to patients who want children.
Impact of fertility preservation counseling and treatment on psychological outcomes among women with cancer: A systematic review
<pubmed>26264701</pubmed>
This article explains about psychological outcomes in female cancer patients who undergo fertility preservation counseling/consultation (FPC), with or without fertility preservation (FP).I read through the whole article as I found it really interesting and relevant to our group project. This is another subheadings we can add to those.
Lab 4 Assessment-Quiz
Mesoderm Development & Placenta Development
Lab 5 Assessment
What is the difference between gastroschisis and omphalocele?
Omphalocele is a rare birth defect that occurs every 1 in 4000 ~ 7000 live births worldwide. Babies with this problem are born with their visceral organs, mainly the liver, and intestine inside a thin membrane sac known as the omphalocele sac external of their abdominal cavity into the base of the umbilical cord. Technically, it is a herniation of the umbilicus. It is an abnormality in the development of the gastrointestinal system at around week 9~12 of fetal development.It occurs when lateral unfolding of the embryo fails for some reason, leading to the formation of an omphalocele. The organs are placed inside the abdominal cavity through surgery, usually within the first half year of the child being born [1] ,[2] .
Children born with this defect often have other abnormalities, often chromosomal such as a Trisomy at pair 13, 18 or 21. It is unknown the causes of this birth defect; some investigation have suggested maternal age, multiple pregnancies, and number of births may increase the chance of a child being born with an omphalocele, but there are also many studies that do not agree with this. It is thought that smoking, consumption of alcohol, and not enough dietary foliate in the mother may contribute to this birth defect.The survival rate for children born with just an omphalocele and do not have any other health problems is 90%.A woman carrying a fetus with omphalocele often have high levels of alpha-fetoprotein in her body. Blood testing, detailed fetal ultrasound, ultra-fast fetal MRI and a fetal echocardiogram can lead to early diagnosis of a omphalocele whilst in the fetal stage, and in many cases where it is legal, the pregnancy is terminated [3] , [4].
BUT Gastrochisis is a development abnormality of the anterior abdominal wall, where the bowel protrudes without a covering sac between the developing rectus muscles, occurring slightly lateral and towards the right of the fetal umbilicus. Gastrochisis commonly occurs as an isolated malformation, occurring in approximately 2.5 in 10’000 births [5].
During the 4th week of normal fetal development, the lateral body of the fetus folds, moving ventrally and fusing in the midline to form the anterior body wall. It has been suggested that the incomplete fusion of the midline results in this abnormality, resulting in the abdominal viscera to protrude through the abdominal wall, herniating through the rectus muscle. This is one of the many theories related to Gastrochisis as the cause is still unclear. Other theories include, the failure of mesoderm to form in the body wall, rupture of the amnion around the umbilical ring with subsequent herniation of the bowel, abnormal involution of the right umbilical vein resulting in a weakening of the body wall and thus resulting in herniation of the bowel, and disruption of the right vitelline (yolk sac) artery with consequent body wall damage and gut herniation [6] , [7] .
References
- ↑ CDC - Birth Defects, Facts about Omphalocele, [ http://www.cdc.gov/ncbddd/birthdefects/omphalocele.html ], Friday June 8, 2015
- ↑ Omphalocele | Birth Anomalies | Prognosis & Treatment, [ http://www.cincinnatichildrens.org/health/o/omphalocele/ ], Friday June 8, 2015
- ↑ <pubmed>13989758</pubmed>
- ↑ <pubmed>13303095</pubmed>
- ↑ <pubmed>19419415</pubmed>
- ↑ <pubmed>25059025</pubmed>
- ↑ <pubmed>17230493</pubmed>
Please do not use your real name on this website, use only your student number.
- 2015 Course: Week 2 Lecture 1 Lecture 2 Lab 1 | Week 3 Lecture 3 Lecture 4 Lab 2 | Week 4 Lecture 5 Lecture 6 Lab 3 | Week 5 Lecture 7 Lecture 8 Lab 4 | Week 6 Lecture 9 Lecture 10 Lab 5 | Week 7 Lecture 11 Lecture 12 Lab 6 | Week 8 Lecture 13 Lecture 14 Lab 7 | Week 9 Lecture 15 Lecture 16 Lab 8 | Week 10 Lecture 17 Lecture 18 Lab 9 | Week 11 Lecture 19 Lecture 20 Lab 10 | Week 12 Lecture 21 Lecture 22 Lab 11 | Week 13 Lecture 23 Lecture 24 Lab 12 | 2015 Projects: Three Person Embryos | Ovarian Hyper-stimulation Syndrome | Polycystic Ovarian Syndrome | Male Infertility | Oncofertility | Preimplantation Genetic Diagnosis | Students | Student Designed Quiz Questions | Moodle page