SH Lecture - Lymphatic Structure and Organs
Introduction
Start Time/End Time: 10am to 11am Monday 28 February 2011
Campus: Kensington Location: Clancy Auditorium eMed Link to Learning Activity - Lymphatic organs histology
Aim
This lecture will provide an overview of the histology of key lymphoid organs, including the lymph nodes, spleen and thymus, as well as extranodallymphoid tissues including mucosal associated lymphoid tissues (MALT)
Key Concepts: Lymphoid tissue. Mucosal-associated lymphoid tissue, Mononuclear phagocytic system (MPS)
Background
- Lymphatic System
- Organs - Thymus, Spleen
- Lymph Nodes and Nodules
- Bone Marrow
- Extranodal Lymphoid Tissues
- Mucosal Associated Lymphoid Tissues (MALT)
Online - UNSW Cell Biology Lecture 2008
Textbook References
- Histology and Cell Biology - A.L. Kiersenbaum
- Chapter 6: Blood
- Chapter 10: Immune-Lymphatic
- Janeway’s Immunobiology NCBI Bookshelf | Publisher page
- SH Laboratory this week
Two Systems
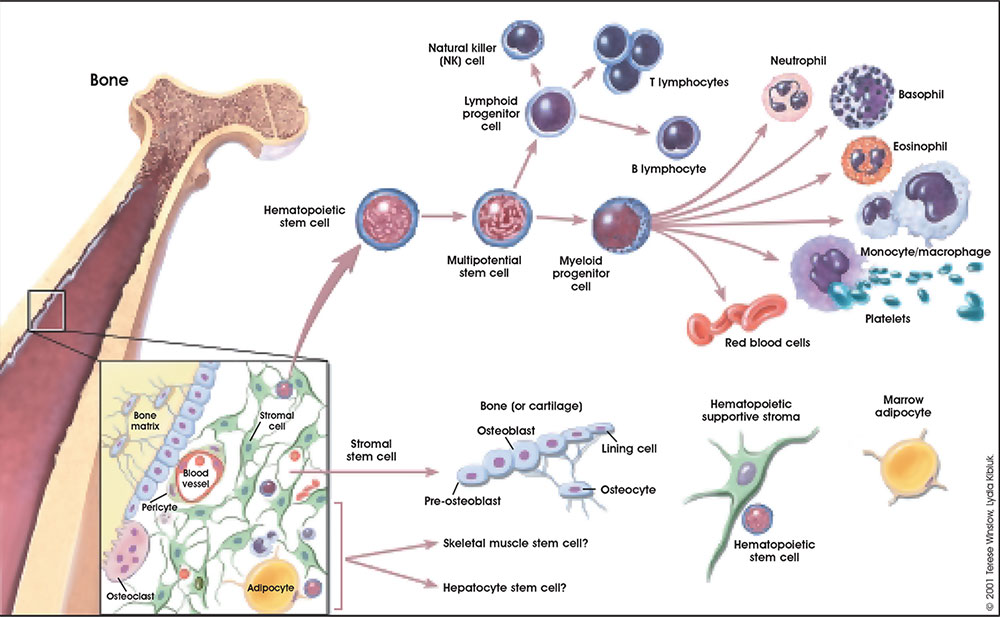
- Lymphoid System - three major types of lymphocytes (T, B, and NK), tissues, organs and vessels
- Mononuclear Phagocytic System (MPS, also called Lymphoreticular System or Reticuloendothelial System, RES) - circulating monocytes of peripheral blood and non-circulating (fixed) tissue macrophages found throughout the body
MBoC Figure 24-3 Human lymphoid organs
Lymphatic System
- Connective Tissue Embryonic origin- Mesoderm
- Consists of Cells, tissues and organs
- Immune “monitor” of body surfaces, internal fluids
Immune System Note: Immunity is covered in detail elsewhere in the course current lecture is about Lymphoid Organ structure/location
- Tissues and Organs
- Thymus, spleen, lymph nodes, lymphatic nodules, diffuse lymphatic tissues, bone marrow
- Organs consist also of structural cells and extracellular matrix
- Lymphatic vessels connect system parts
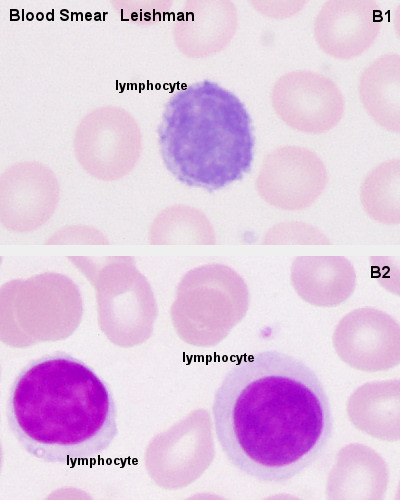
- Cells are Lymphocytes
- B Lymphocytes and T Lymphocytes MBoC Figure 24-7. Electron micrographs of nonactivated and activated lymphocytes
- White blood cells, leukocytes
These are blood cells
Blood Cells
File:Ly106le.jpg large granular lymphocytes - natural killer (Nk-) cells
Central/Peripheral Lymphoid Organs
Central lymphoid organs
- Lymphocytes develop from precursor cells
Peripheral lymphoid organs
- Lymphocytes respond to antigen
- lymph nodes or spleen
Mononuclear Phagocytic System
(Mononuclear Phagocytic System MPS, also called Lymphoreticular System or Reticuloendothelial System, RES)
File:Mono101le.jpg File:Liv41re.jpg
Mononuclear Phagocytes 2 types:
- Circulating monocytes of peripheral blood (monocytes entering the connective tissue differentiate into macrophages)
- Non-circulating (fixed) tissue macrophages found throughout the body (Liver (Kuffler cells), spleen and other tissues)
Lymph
- Fluid portion of lymphatic circulation
- blood plasma will leave blood vessels into surrounding tissues
- adds to normal tissue interstitial fluid
- surplus of liquid needs to be returned to circulation
- Lymph vessels are provide unidirectional flow of this liquid
Lymph Vessels
Three types based on size and morphology
- Lymph capillaries begin as blind-ending tubes in connective tissue, larger than blood capillaries, very irregularly shaped
- Lymph collecting vessels larger and form valves, morphology similar to lymph capillaries
- Lymph ducts 1 or 2 layers of smooth muscle cells in wall
(Remember anatomy NAVL = Nerve, Artery, Vein and Lymph)
Lymphocyte Circulation
- The circulation through a lymph node is shown.
- Microbial antigens are carried into the lymph node by dendritic cells, which enter via afferent lymphatic vessels draining an infected tissue.
- T and B cells, by contrast, enter the lymph node via an artery and migrate out of the bloodstream through postcapillary venules.
- Unless they encounter their antigen, the T and B cells leave the lymph node via efferent lymphatic vessels, which eventually join the thoracic duct.
- The thoracic duct empties into a large vein carrying blood to the heart.
- A typical circulation cycle takes about 12–24 hours.
Links: MBoC Chapter 24 - The Adaptive Immune System | MBoC Figure 24-14. The path followed by lymphocytes as they continuously circulate between the lymph and blood | Immunobiology
MALT, BALT & GALT
Internal epithelia Associated Lymphoid Tissue - naming based upon the anatomical locations
- Mucosa Associated Lymphoid Tissue (MALT)
- Bronchus Associated Lymphoid Tissue (BALT)
- Gut Associated Lymphatic Tissue (GALT)
- Diffuse lymphatic tissue + nodules
- Reactive - enlarge when activated (by antigen)
Diffuse Lymphatic Tissue
Alimentary canal, respiratory passage, urogenital tract
- Not enclosed by a capsule
- Located in subepithelial tissue - Lamina propria
Lymphocytes
- travel to nodes and back again
- proliferation and differentiation
Effector cells
- B Cell secreting antibody = Plasma Cell
- T Cell = Memory Cell
Immune Responses
Adaptive immunity has 2 main classes
- Antibody-mediated - B Lymphocyte
- Cell-mediated - T Lymphocyte
Lymph Nodules
(or follicles)
- Organized concentrations of Lymphocytes
- No capsule, covered by epithelia
- Nodules are also unit structure seen in a node
- Oval concentrations in meshwork of reticular cells
Reticular cell
- produces reticular fibers (collagen type III) and surrounds the fibers with its cytoplasm
- reticular fibers are also produced by fibroblasts
Gastrointestinal Tract
- Oropharynx - Tonsils
- Distal small intestine (ilieum) - Peyer’s Patches
Appendix, cecum
Nodule States
- Primary Nodule - Mainly small lymphocytes
- Secondary Nodule
- Central pale region (germinal centre) - Effector cells and macrophages
- Dark outer ring (small lymphocytes)
Links: Immnuobiology - Figure 1.10. Organization of typical gut-associated lymphoid tissue
Tonsils
Anatomical location - Palatine (tonsils), Lingual and Pharyngeal ( adenoids )
Palatine Tonsils
File:Tns02he.jpg File:Tns40he.jpg
- the "tonsils", lateral wall of oropharynx
- covered by stratified squamous epithelium
- numerous crypts (10-20) infolds of surface epithelium
- Afferent lymph vessels absent
- Efferent lymph vessels are present
Lingual Tonsils
- lamina propria root of tongue
- covered by stratified squamous epithelium
- salivary glands and skeletal muscle are directly adjacent
Pharyngeal Tonsils
- adenoids or nasopharyngeal tonsils, upper posterior part of throat
- covered by a pseudostratified ciliated epithelium with goblet cells
Peyer's Patch
File:Pey02he.jpg File:Pey102he.jpg
Peyer's Patch, Ileum
microfold cells or M-cells
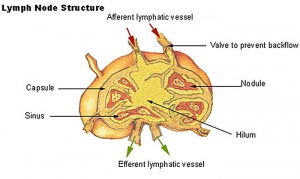
Lymph Nodes
Immunobiology - Figure 1.8. Organization of a lymph node
MBoC Figure 24-16. A simplified drawing of a human lymph node
- Encapsulated organ (1 mm - 2 cm)
- In lymph vessel pathways “filter”
- Afferent- towards node
- Efferent- away from node
- Location throughout the entire body - Concentrated in axilla, groin, mesenteries
- Antigen transformed lymphocytes from the blood
Lymph Node Structure
- Capsule - dense connective tissue
- Trabeculae - dense connective tissue
- Reticular Tissue - Reticular cells and fibers, supporting meshwork
File:Lyn041he.jpg File:Lyn10he.jpg
Lymph
- enters the node through afferent vessels
- filters through the sinuses
- leaves through efferent vessels
Subcapsular sinus = marginal sinus
Continuation of trabecular sinus
Lymph Node Development
Lymph Node Vessels
Lymphocyte Traffic
Links: Immunobiology - Figure 1.8. Organization of a lymph node | Blue Histology - Lymph Nodes
Thymus
MBoC Figure 24-6. The development and activation of T and B cells
Figure 24-7. Electron micrographs of nonactivated and activated lymphocytes
Development Changes
Changes with age Overall Size
- birth 10-15 g
- puberty 30-40 g
- after puberty - involution
- Replaced by adipose tissue
- middle-aged 10 g
Thymus Anatomy
- Superior mediastinum, anterior to heart
- Bilobed lymphoepithelial organ
- Contains reticular cells but no fibers
- Stem lymphocytes
- proliferate and differentiate
- forms long-lived T- lymphocytes
Thymus Cells
- Reticular cells
- Abundant, eosinophilic, large, ovoid and light nucleus 1-2 nucleoli
- sheathe cortical capillaries
- form an epitheloid layer
- maintain microenvironment for development of T-lymphocytes in cortex (thymic epitheliocytes)
- Macrophages
- cortex and medulla
- difficult to distinguish from reticular cells in H&E
- Lymphocytes
- cortex and medulla - more numerous (denser) in cortex
- majority of them developing T-lymphocytes (= thymic lymphocytes or thymocytes)
Fetal/Young Thymus
Thymic corpuscle
Hassall’s corpuscle - Mass of concentric epithelioreticular cells
Adult Thymus
Cortical lymphoid tissue replaced by adipose tissue Increase in size of thymic corpuscles
Links: Blue Histology - Thymus
Spleen
- Like- lymph nodes (filter)
- Unlike- is in blood stream
Structure
- Capsule, trabeculae (dense connective tissue)
- Splenic pulp White pulp, red pulp Based on appearance and cell content
Splenic Pulp
File:Spl041he.jpg File:Spl042he.jpg
White Pulp
- lymphocytes surround central arteries
- as periarterial lymphoid sheath (PALS)
Red Pulp
- Red blood cells
- Splenic sinuses
- Splenic cords
Spleen Structure
Reticular Fibers
File:Spl10re.jpg File:Spl43re.jpg
Spleen Reticular Fibres
Links: Immunobiology - Figure 1.9. Organization of the lymphoid tissues of the spleen
B Cell Development
- Bone marrow
- blood
- Lymph node, nodule
- Lymphatic vessel
- Bone marrow
Germinal Centres
- Bone Marrow
- Medullary cords contain plasma cells
Plasma cells
- secrete antibody directly into blood for distribution to all body
- in local extrafollicular sites are short lived 2–4 days
- longer-lived plasma cells in bone marrow 3 weeks to 3 months+
Additional Information
The following is not part of the lecture and is for reference purposes only.
- Blood Cells
- Florence R. Sabin (1871-1953)
- Online Resources
- Anatomy of the Human Body (Gray)1918
- Immune Links
Blood Cell Numbers
Red cells
- Male: 4.32 - 5.66 x 1012/l
- Female: 3.88 - 4.99 x 1012/l
Leukocytes
- Male: 3.7 - 9.5 x 109/l
- Female: 3.9 - 11.1 x 109/l
Platelets
- 140 - 440 x 109/l
Leukocytes
- Granulocytes: 1.8 - 8.9 x 109/l
- Neutrophils: 1.5 - 7.4 x 109/l
- Eosinophils: 0.02 - 0.67 x 109/l
- Basophils: 0 - 0.13 x 109/l
- Lymphocytes: 1.1 - 3.5 x 109/l
- B-cells: 0.06 - 0.66 x 109/l
- T-cells: 0.77 - 2.68 x 109/l
- CD4+: 0.53 - 1.76 x 109/l
- CD8+: 0.30 - 1.03 x 109/l
- NK cells: 0.20 - 0.40 x 109/l
- Monocytes: 0.21 - 0.92 x 109/l
Online Resources
UWA Blue Histology UWA Blue Histology | Blood | Lymphoid Tissues 1 | Lymphoid Tissues 2
National Institute of Allergy and Infectious Diseases National Institute of Allergy and Infectious Diseases - Immune System | Organs of the Immune System | Lymph Node | Lymphatic Vessel | Understanding the Immune System: How It Works (PDF)
JayDoc Web lymphoid
Textbook
Immunobiology by Janeway, Charles A.; Travers, Paul; Walport, Mark; Shlomchik, Mark New York and London: Garland Science; c2001
- Immunobiology
- Figure 1.7. The distribution of lymphoid tissues in the body
- Figure 10.18. Anatomy of mucosal immune responses
Anatomy of the Human Body (Gray)1918
- Historic anatomy is good, there are there are some functional inaccuracies.
- The Lymphatic System | The Thoracic Duct | The Spleen | The Thymus |
Lymph Node Analysis
- 3D Reconstruction Pelvic Node Anatomy
- Reconstruction of Axillary Node Anatomy
Laboratory
Introduction
This practical class has 2 main parts.
The first part will look at the cellular components of blood and their development.
The second part will look at the organs and tissues associated with lymphoid (lymphatic) immune function.
The Practical involves studying selected slides from the Virtual Slide Box (some text in these practical notes modified from Virtual Slidebox Histology). Additional online self-directed learning resources are shown below. Today's Laboratory will not cover all the immune system associated with the gastrointestinal tract (GIT), just the tonsilal component.
Objectives
1. Understand the major immune cell types of blood as they appear in blood smears
2. Brief understanding of the appearance and function of blood cells
3. Understand the organization of lymphoid tissue
4. Brief understanding of the organization of thymus, spleen and tonsil
Online References
- Dee, F.R., Leaven, T. and Consoer, D. (2005) Virtual Slidebox of Histology - Hematopoietic system. Retrieved April 14, 2005, from http://www.path.uiowa.edu/cgi-bin-pub/vs/fpx_browse.cgi?cat=o_hemato&div=nlm
- UWA Blue Histology UWA Blue Histology | Blood | Lymphoid Tissues 1 | Lymphoid Tissues 2 | | appendix
UNSW Virtual Slidebox
- http://vslide1.med.unsw.edu.au/B-blood-lymphoid.html or http://web.med.unsw.edu.au/vslide/phase1/indexB3.asp
- This new link does not function http://vslide.med.unsw.edu.au/index.jsp
Blood Cell Data
See also section #Blood Cell Numbers
Bone Marrow
Promyelocyte -> Myelocyte -> Metamyelocyte -> White Blood Cell type
Neutrophil "band form" stage before final maturation
Glossary
A few key terms associated with the Lymphoid system.
adenoid - (Greek " +-oeides = in form of) in the form of a gland, glandular; the pharyngeal tonsil.
Afferent lymph - vessel carrying lymph towards a node.
Antibody mediated immunity - the immune function of plasma cells (active B lymphocytes) secreting antibody which binds antigen.
antibodies - mammals have five classes (IgA, IgD, IgE, IgG, and IgM)
antigen - any substance that is recognised by the immune system and stimulates antibody production.
B lymphocyte (cell) - historically named after a structure called the bursa of Fabricius in birds, a source of antibody-producing lymphocytes. These cells develop in the bone marrow. (More? Electron micrographs of nonactivate and activated lymphocytes)
BALT - Bronchus Associated Lymphoid Tissue
band cell - (band neutrophil or stab cell) seen in bone marrow smear, a cell undergoing granulopoiesis, derived from a metamyelocyte, and leading to a mature granulocyte. Also occasionally seen in circulating blood.
cell - has a specific cell biology definition, but is often used instead of "lymphocyte" when describing B and T cells.
Cell-mediated immunity - the immune function of T lymphocytes.
"clockface" - a term used to describe the appearance of plasma cell nuclei due to the clumping of the chromatin at the nucleus periphery. More clearly seen in tissue plasma cells that the bone marrow smear, where they are sometimes confused with the basophilic erythroblasts.
cords of Billroth - spleen cellular columns located in red pulp. surrounded by splenic sinusoids. Cords contain reticular cells, macrophages, lymphocytes, plasma cells and erythrocytes.
cortex - outer layer, used in association with medulla (innner layer or core) a general description that can be applied to describing an organ with a layered structure.
Effector cells - the immune functioning (active) B and T lymphocytes.
Efferent lymph - vessel carrying lymph away from a node.
GALT - Gut Associated Lymphatic Tissue
haemopoiesis (hemopoiesis) formation of blood cells.
IgA - the main class of antibody in secretions (saliva, tears, milk, and respiratory and intestinal secretions).
IgD - the immunoglobulin B cell starts to produce as a cell-surface molecule after leaving the bone marrow.
IgE - bind Fc receptors (surface of mast cells in tissues and basophils in the blood).
IgG - the major class of immunoglobulin in the blood.
IgM - the first class of antibody made by a developing B cell, which may switch to making other classes of antibody.
immunodeficiency - when one or more components of the immune system is defective. (More? Immunobiology - immunodeficiency)
involution - in the Thymus refers to the replacement, mainly in the cortex, of cells by adipose tissue. (More? PubMed- thymus involution) | Cancer Medicine - Thymomas and Thymic Tumors)
lamina propria - a layer of loose connective tissue found underneath the epithelium of mucosa.
Leukocyte- (Greek, lukos= clear, white) white blood cell.
lingual- related to the tongue.
lymph node - connective tissue encapsulated lymphoid organ (1mm - 2cm in size), positioned in the pathway of lymph vessels.
macrophage - a large highly motile white blood cell which engulfs foreign material (bacteria etc) and both degenerating cells and cell fragments. Found in many different tissues and locations. (More? Immunobiology - Defects in phagocytic cells are associated with persistence of bacterial infection)
MALT - Mucosa Associated Lymphoid Tissue medulla - innner layer, used in association with cortex (outer layer) a general description that can be applied to describing an organ with a layered structure.
medulla - inner layer or core, used in association with cortex (outer layer) a general description that can be applied to describing an organ with a layered structure.
Memory Cell - effector T cell (lymphocyte)
normoblast - seen in bone marrow smear, a developing erythroblast (red blood cell) that still retains a nucleus.
parenchyma - (Greek = enkeim "to pour in") cells forming the functional cells of an organ or tissue. These cells carry out the function of the organ at a cellular level, and are not the structural cells, connective tissue, extracellular matrix (stromal).
periarterial lymphoid sheath - (PALS) in the spleen the white pulp that surrounds the central arteries. (T-lymphocytes,macrophages and plasma cells)
Plasma Cell - active B cell (lymphocyte) which is secreting antibody. Located in either bone marrow or peripheral lymphoid tissues, these cells have and increased cytoplasmic volume (due to increase rough endoplasmic reticulum) in comparison to the inactive (non-secreting) lymphocyte.
splenic sinusoids - enlarged spleen capillary spaces located in red pulp and surrounding cords of Billroth.
stroma - (Greek = "a cover, table-cloth, bedding") tissue forming the framework/support of an organ or tissue. That is the structural cells which form connective tissue and secrete extracellular matrix, rather than the functional cells (parenchymal). All organs can therefore be functionally divided into these 2 components, stromal/parenchymal.
Subcapsular sinus (=marginal sinus) space lying under the connective tissue capsule which receives lymph from afferent lymphatic vessels.
Thymic corpuscle (=Hassall’s corpuscle) a mass of concentric epithelioreticular cells found in the thymus. The number present and size tend to increase with thymus age. (see classical description of Hammar, J. A. 1903 Zur Histogenese und Involution der Thymusdriise. Anat. Anz., 27: 1909 Fiinfzig Jahre Thymusforschung. Ergebn. Anat. Entwickl-gesch. 19: 1-274.)
thymic epitheliocytes - reticular cells located in the thymus cortex that ensheathe the cortical capillaries, creating and maintain the microenvironment necessary for the development of T-lymphocytes in the cortex.
T lymphocyte (cell) - named after thymus, where they develop, the active cell is responsible for cell-mediated immunity. (More? Electron micrographs of nonactivate and activated lymphocytes)
thymus
tonsils