SH Lecture - Lymphatic Structure and Organs: Difference between revisions
(→Terms) |
No edit summary |
||
| Line 24: | Line 24: | ||
* '''Janeway’s Immunobiology''' (see in [[SH_Lecture_-_Lymphatic_Structure_and_Organs#Additional_Information|additional information]]) [http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=imm.TOC&depth=2 NCBI Bookshelf] | * '''Janeway’s Immunobiology''' (see in [[SH_Lecture_-_Lymphatic_Structure_and_Organs#Additional_Information|additional information]]) [http://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=imm.TOC&depth=2 NCBI Bookshelf] | ||
* '''Histology and Cell Biology''' - A.L. Kiersenbaum (2001) Chapter 6: Blood, Chapter 10: Immune-Lymphatic | * '''Histology and Cell Biology''' - A.L. Kiersenbaum (2001) Chapter 6: Blood, Chapter 10: Immune-Lymphatic | ||
* Previous Lectures: [http://php.med.unsw.edu.au/cellbiology/index.php?title=2010_Society_and_Health_-_Lymphatic_organs_histology 2010] | [http://cellbiology.med.unsw.edu.au/units/medicine/SHlymph.htm 2008] | * Previous Lectures: [http://php.med.unsw.edu.au/embryology/index.php?title=SH_Lecture_-_Lymphatic_Structure_and_Organs&oldid=115513 2012] | [[SH_Lecture_-_Lymphatic_Structure_and_Organs&oldid=115513|2012]] | [http://php.med.unsw.edu.au/cellbiology/index.php?title=2010_Society_and_Health_-_Lymphatic_organs_histology 2010] | [http://cellbiology.med.unsw.edu.au/units/medicine/SHlymph.htm 2008] | ||
Revision as of 10:32, 3 March 2013
Introduction
While the structure of the lymphatic system (lympha = clear water) is well described, there is much to still learn about the complex development and function of this "system".
- Immune - “monitor” of body surfaces, internal fluids
- Extracellular fluid - returns interstitial fluid to circulation
- Gastrointestinal tract - carries fat and fat-soluble vitamins
Aim
This lecture will provide an overview of the histology of key lymphoid organs, including the lymph nodes, spleen and thymus, as well as extranodal lymphoid tissues including mucosal associated lymphoid tissues (MALT)
Key Concepts
- Lymphatic System
- Organs - Thymus, Spleen
- Lymph Nodes and Nodules
- Bone Marrow
- Extranodal Lymphoid Tissues
- Mucosal Associated Lymphoid Tissues (MALT)
Textbook References
- SH Laboratory Support
- Janeway’s Immunobiology (see in additional information) NCBI Bookshelf
- Histology and Cell Biology - A.L. Kiersenbaum (2001) Chapter 6: Blood, Chapter 10: Immune-Lymphatic
- Previous Lectures: 2012 | 2012 | 2010 | 2008
Two Cellular Systems
- Lymphoid System - three major types of lymphocytes (T, B, and NK), tissues, organs and vessels
- Mononuclear Phagocytic System (MPS, also called Lymphoreticular System or Reticuloendothelial System, RES) - circulating monocytes of peripheral blood and non-circulating (fixed) tissue macrophages found throughout the body
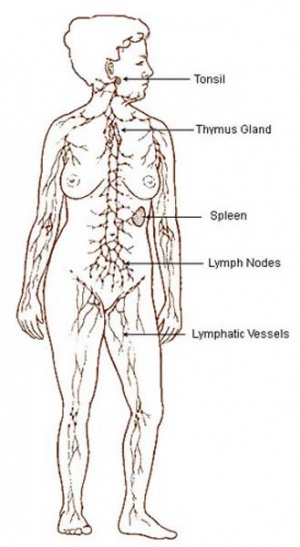
MBoC Figure 24-3 Human lymphoid organs
Lymphatic System
- Connective Tissue Embryonic origin- Mesoderm
- Consists of Cells, tissues and organs
Immune System Note: Immunity is covered in detail elsewhere in the course, current lecture is about Lymphoid Organ structure/location
- Tissues and Organs
- Thymus, spleen, lymph nodes, lymphatic nodules, diffuse lymphatic tissues, bone marrow
- Organs consist also of structural cells and extracellular matrix
- Lymphatic vessels connect system parts
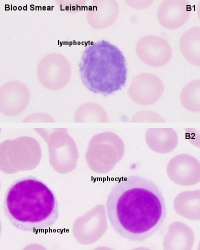
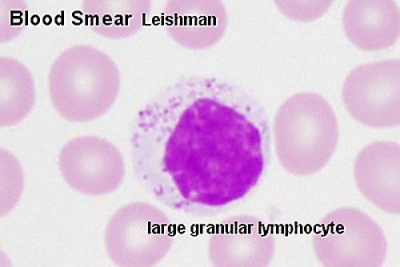
- Cells are Lymphocytes
- B Lymphocytes and T Lymphocytes
- White blood cells, leukocytes
These are blood cells
Blood Cells
Lymphocyte Electron Micrographs
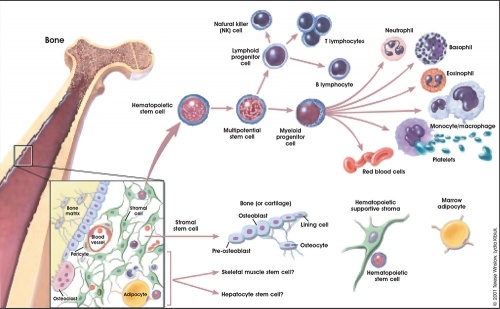
Central/Peripheral Lymphoid Organs
Central lymphoid organs
- Lymphocytes develop from precursor cells (see blood marrow image)
Peripheral lymphoid organs
- Lymphocytes respond to antigen
- lymph nodes or spleen
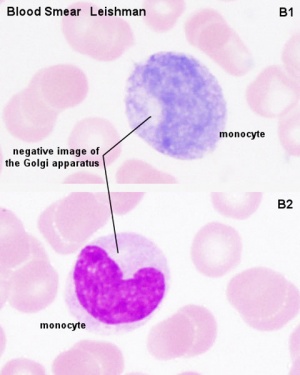
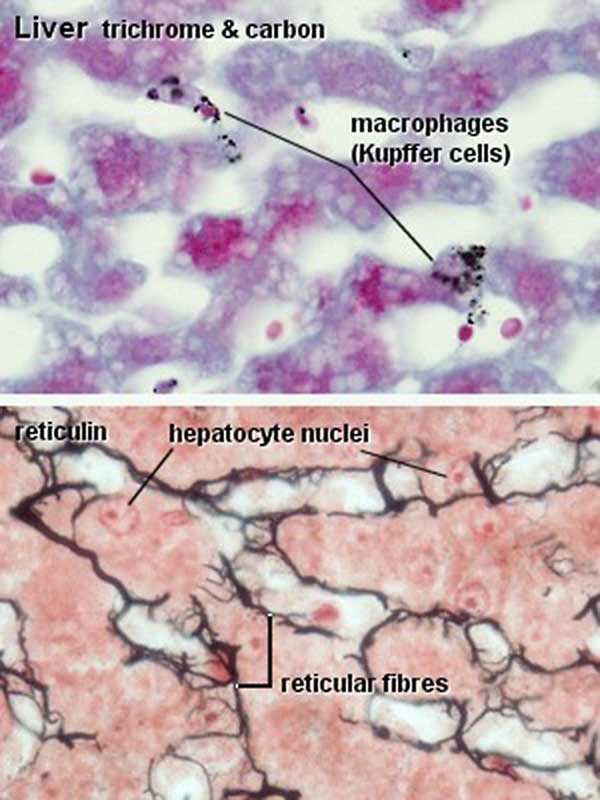
Mononuclear Phagocytic System
(Mononuclear Phagocytic System MPS, also called Lymphoreticular System or Reticuloendothelial System, RES)
Mononuclear Phagocytes 2 types:
- Circulating monocytes of peripheral blood (monocytes entering the connective tissue differentiate into macrophages)
- Non-circulating (fixed) tissue macrophages (MΦ) found throughout the body (Liver (Kuffler cells), spleen and other tissues)
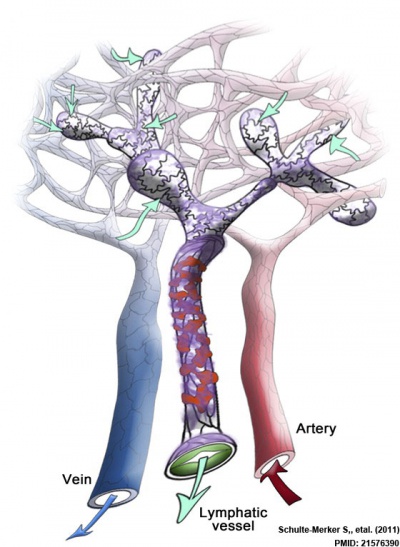
Lymph
- Fluid portion of lymphatic circulation
- blood plasma will leave blood vessels into surrounding tissues
- adds to normal tissue interstitial fluid
- surplus of liquid needs to be returned to circulation
- Lymph vessels provide unidirectional flow of this liquid
Lymph Vessels
Three types based on size and morphology
- Lymph capillaries begin as blind-ending tubes in connective tissue, larger than blood capillaries, very irregularly shaped
- Lymph collecting vessels larger and form valves, morphology similar to lymph capillaries
- Lymph ducts 1 or 2 layers of smooth muscle cells in wall
(Remember anatomy acronym - NAVL = Nerve, Artery, Vein and Lymph)
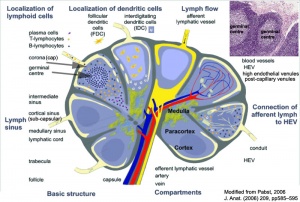
Lymphocyte Circulation
- The circulation through a lymph node is shown.
- Microbial antigens are carried into the lymph node by dendritic cells, which enter via afferent lymphatic vessels draining an infected tissue.
- T and B cells, by contrast, enter the lymph node via an artery and migrate out of the bloodstream through postcapillary venules.
- Unless they encounter their antigen, the T and B cells leave the lymph node via efferent lymphatic vessels, which eventually join the thoracic duct.
- The thoracic duct empties into a large vein carrying blood to the heart.
- A typical circulation cycle takes about 12–24 hours.
Links: MBoC Chapter 24 - The Adaptive Immune System | MBoC Figure 24-14. The path followed by lymphocytes as they continuously circulate between the lymph and blood | Immunobiology
Diffuse Lymphatic Tissue
Alimentary canal, respiratory passage, urogenital tract
- Not enclosed by a connective tissue capsule
- Located in subepithelial tissue - Lamina propria
Lymphocytes
- travel to nodes and back again
- proliferation and differentiation
Effector cells
- B Cell secreting antibody = Plasma Cell
- T Cell = Memory Cell, Cytotoxic T cells, T helper cell
- Diffuse lymphatic tissue + nodules
- Reactive - enlarge when activated (by antigen)
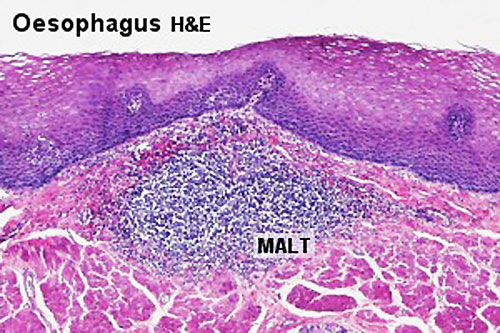
MALT, BALT and GALT
|
Internal epithelia Associated Lymphoid Tissue - naming based upon the anatomical locations
MALT - Mucosa Associated Lymphoid Tissue
|
Immune Responses
Adaptive immunity has 2 main classes
- Antibody-mediated - B Lymphocyte
- Cell-mediated - T Lymphocyte
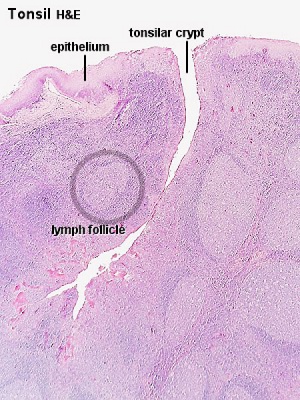
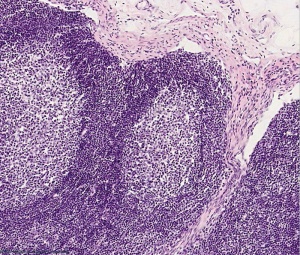
Lymph Nodules
- Organized concentrations of lymphocytes
- No capsule, covered by epithelia
- Nodules are also the unit structure seen in a node
- Oval concentrations in meshwork of reticular cells
Gastrointestinal Tract
- Oropharynx - Tonsils
- Distal small intestine (ilieum) - Peyer’s Patches
- Appendix, cecum
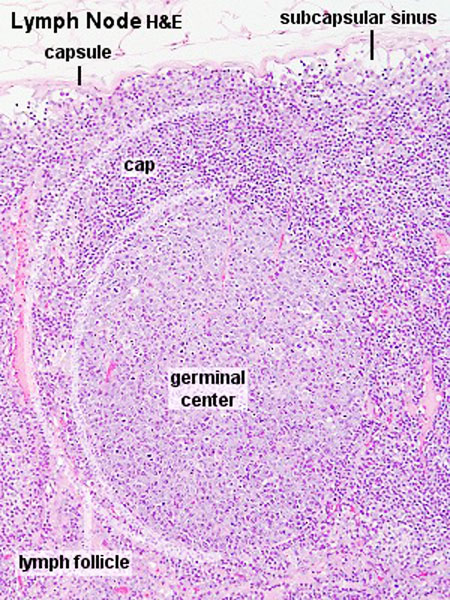
Nodule States
- Primary Nodule - Mainly small lymphocytes
- Secondary Nodule
- Central pale region (germinal centre) - Effector cells and macrophages
- Dark outer ring (small lymphocytes)
Links: Immnuobiology - Figure 1.10. Organization of typical gut-associated lymphoid tissue
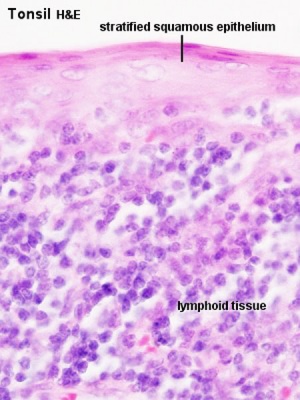
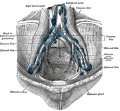
Tonsils
Anatomical location - Palatine (tonsils), Lingual and Pharyngeal ( adenoids )
Palatine Tonsils
- the "tonsils", lateral wall of oropharynx
- covered by stratified squamous epithelium
- numerous crypts (10-20) infolds of surface epithelium
- Afferent lymph vessels absent
- Efferent lymph vessels are present
Lingual Tonsils
- lamina propria root of tongue
- covered by stratified squamous epithelium
- salivary glands and skeletal muscle are directly adjacent
Pharyngeal Tonsils
- adenoids or nasopharyngeal tonsils, upper posterior part of throat
- covered by a pseudostratified ciliated epithelium with goblet cells
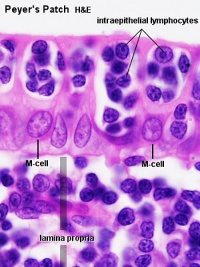
Peyer's Patch
Peyer's Patch, Ileum
microfold cells or M-cells
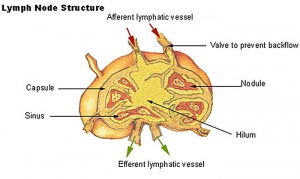
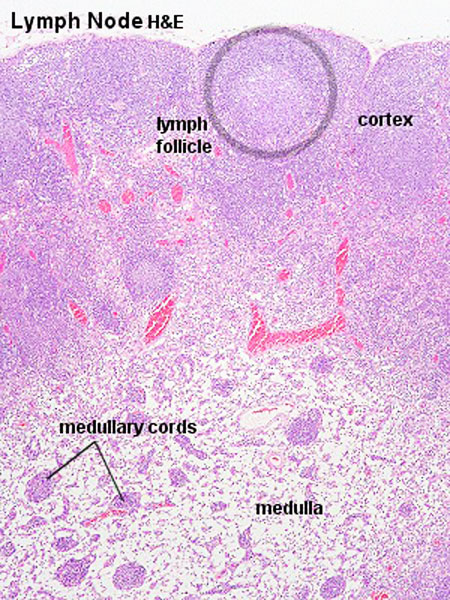
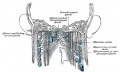
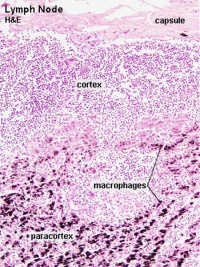
Lymph Nodes
Quicktime Movie - Mouse Lymph Node 7 | more lymph node movies
Immunobiology - Figure 1.8. Organization of a lymph node
MBoC Figure 24-16. A simplified drawing of a human lymph node
* Encapsulated organ (1 mm - 2 cm)
|
|
Lymph Node Structure
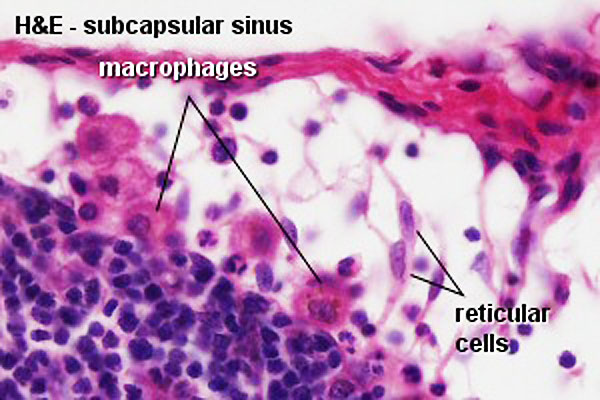
Connective Tissue
- Capsule - dense connective tissue (irregular CT, some adipocytes))
- Trabeculae - dense connective tissue
- Reticular Tissue - Reticular cells and fibers, supporting meshwork (collagen type III)
- Reticular cell produces reticular fibers (collagen type III) and surrounds the fibers with its cytoplasm
- reticular fibbers can also be produced by fibroblasts
Lymph
- enters the node through afferent vessels
- filters through the sinuses
- leaves through efferent vessels
Subcapsular sinus = marginal sinus
Continuation of trabecular sinus
Lymphocyte (T and B) Traffic
- Enter from high endothelial venules (HEVs also called post-capillary venules)
- Spend 8 to 24 h in the lymph node interstitium.
- Enter a network of medullary sinuses.
- Drain from sinuses into efferent lymphatic vessels.
Links: Immunobiology - Figure 1.8. Organization of a lymph node
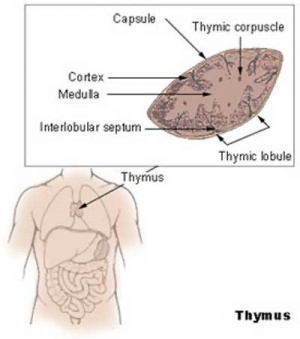
Thymus
|
MBoC Figure 24-6. The development and activation of T and B cells
Figure 24-7. Electron micrographs of nonactivated and activated lymphocytes |
Development Changes
Changes with age Overall Size
- birth 10-15 g
- puberty 30-40 g
- after puberty - involution
- Replaced by adipose tissue
- middle-aged 10 g
Thymus Anatomy
- Superior mediastinum, anterior to heart
- Bilobed lymphoepithelial organ
- Contains reticular cells but no fibers
- Stem lymphocytes
- proliferate and differentiate
- forms long-lived T- lymphocytes
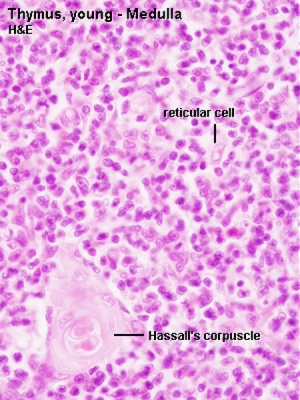
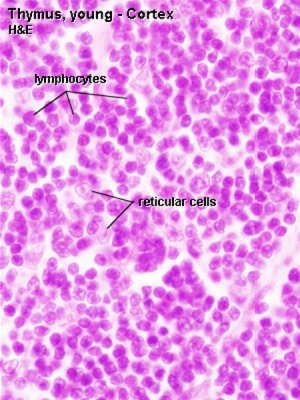
Thymus Cells
- Reticular cells
- Abundant, eosinophilic, large, ovoid and light nucleus 1-2 nucleoli
- sheathe cortical capillaries
- form an epitheloid layer
- maintain microenvironment for development of T-lymphocytes in cortex (thymic epitheliocytes)
- Macrophages
- cortex and medulla
- difficult to distinguish from reticular cells in H&E
- Lymphocytes
- cortex and medulla - more numerous (denser) in cortex
- majority of them developing T-lymphocytes (= thymic lymphocytes or thymocytes)
Fetal/Young Thymus
|
|
| Young medulla | Young cortex |
Thymic corpuscle
Hassall’s corpuscle - Mass of concentric epithelioreticular cells
Adult Thymus
- Cortical lymphoid tissue is replaced by adipose tissue
- Increase in size of thymic corpuscles
- Thymus Histology: Fetal Thymus overview | Fetal Thymus Medulla | Fetal Thymus Cortex | Adult Thymus | unlabeled fetal overview | unlabeled fetal medulla |unlabeled fetal thymic corpuscle |unlabeled fetal cortex | unlabeled adult overview | Category:Thymus | Immune System Development
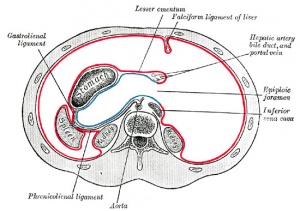
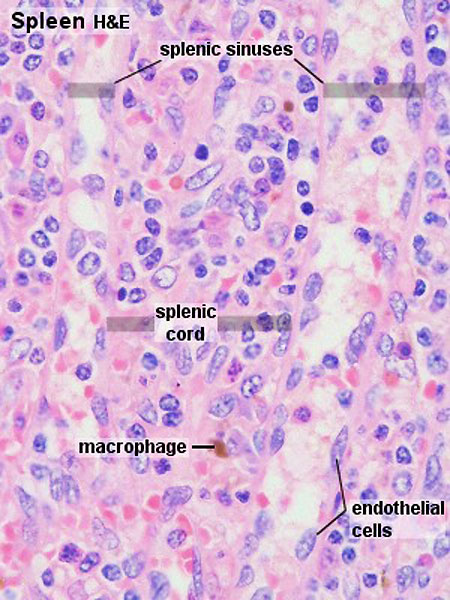
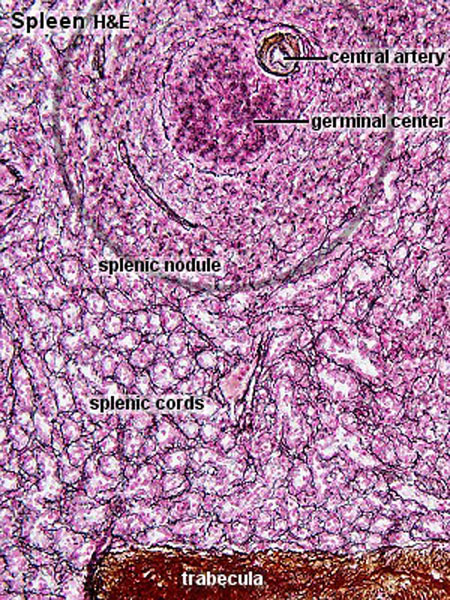
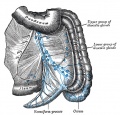
Spleen
Functions
1. Immune
- filters blood in much the way that the lymph nodes filter lymph.
- Lymphocytes in the spleen react to pathogens in the blood and attempt to destroy them.
- Macrophages then engulf the resulting debris, the damaged cells, and the other large particles.
2. Red Blood Cell Removal
- The spleen (and liver) removes old and damaged erythrocytes from the circulating blood.
- Like other lymphatic tissue, it produces lymphocytes, especially in response to invading pathogens.
3. Blood Reservoir
- The sinuses in the spleen also act as a reservoir for blood.
- In emergencies, such as hemorrhage, smooth muscle in the vessel walls and in the capsule of the spleen contracts.
- This squeezes the blood out of the spleen into the general circulation.
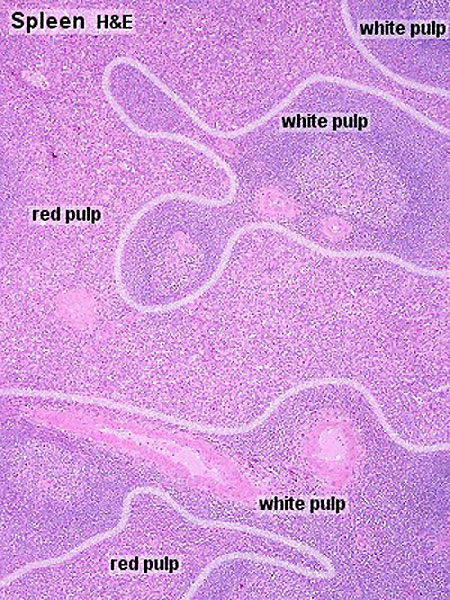
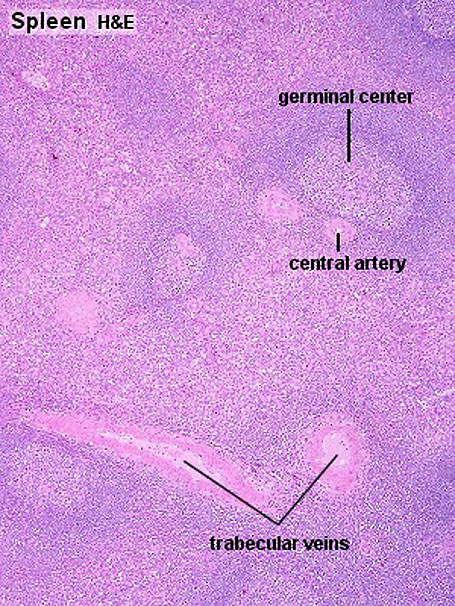
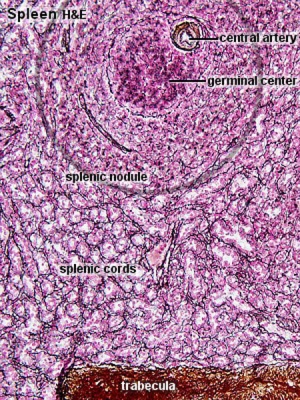
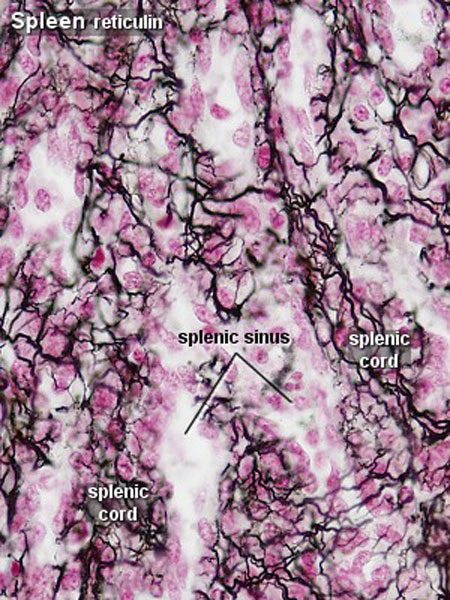
Structure
- Capsule, trabeculae (dense connective tissue)
- Splenic pulp White pulp, red pulp - based on appearance and cell content
White Pulp
- lymphocytes surround central arteries
- as periarterial lymphoid sheath (PALS)
Red Pulp
- Red blood cells
- Splenic sinuses
- Splenic cords
Reticular Fibers
| Spleen Development: SH Lecture Spleen | SH Adult Histology | Overview Red and White Pulp | Overview Red and White Pulp | Cords and Sinuses | Reticular Fibre overview | Reticular Fibre detail | unlabeled red and white pulp | unlabeled red pulp and macrophages | unlabeled white pulp germinal centre | unlabeled reticular fibre | unlabeled white pulp reticular | unlabeled red pulp reticular | Structure cartoon | Cartoon and stain | Category:Spleen | Histology Stains | Immune System Development |
Links: Immunobiology - Figure 1.9. Organization of the lymphoid tissues of the spleen
B Cell Development
- Bone marrow
- blood
- Lymph node, nodule
- Lymphatic vessel
- Bone marrow
Germinal Centres
- Bone Marrow
- Medullary cords contain plasma cells
Plasma cells
- secrete antibody directly into blood for distribution to all body
- in local extrafollicular sites are short lived 2–4 days
- longer-lived plasma cells in bone marrow 3 weeks to 3 months+
Additional Information
The following is not part of the lecture and is for reference purposes only.
| SH Practical - Lymphatic Structure and Organs associated practical support page. Note that virtual slides will be used in the associated practical class and this linked page is provided for student self-directed learning of concepts from the virtual slides. | Additional Images
|
| Janeway’s Immunobiology |
|---|
| A useful resource textbook for further reading on Lymphatic Structure and Organs is Immunobiology 5th edition The Immune System in Health and Disease Charles A Janeway, Jr, Paul Travers, Mark Walport, and Mark J Shlomchik. Open links in a new tab if you wish to refer back to this lecture page.
I have included some links in this table below to specific notes and there is also available a complete list of contents. External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation. Immunobiology 5th edition The Immune System in Health and Disease Charles A Janeway, Jr, Paul Travers, Mark Walport, and Mark J Shlomchik. Part I. An Introduction to Immunobiology and Innate Immunity Chapter 1. Basic Concepts in Immunology
Part III. The Development of Mature Lymphocyte Receptor Repertoires Chapter 7. The Development and Survival of Lymphocytes
|
| Blood Cells |
|---|
Blood cell information shown in the table below is also additional information for reference purposes.
Blood Cell NumbersThe adult ranges of cells / 1 litre (l), total blood volume is about 4.7 to 5 litres. Blood Development | Blood Histology Red Blood Cells
Leukocytes (white blood cells)
Granulocytes
Non-Granulocytes
Lymphocytes
Platelets
|
| Anatomy of the Human Body (1918) - Lymphatics |
|---|
| Anatomy of the Human Body Gray (1918) Historic anatomy is good, though there are there are some functional inaccuracies.
|
Terms
A few key terms associated with the Lymphoid system.
- adenoid - (Greek " +-oeides = in form of) in the form of a gland, glandular; the pharyngeal tonsil.
- Afferent lymph - vessel carrying lymph towards a node.
- Antibody mediated immunity - the immune function of plasma cells (active B lymphocytes) secreting antibody which binds antigen.
- antibodies - mammals have five classes (IgA, IgD, IgE, IgG, and IgM)
- antigen - any substance that is recognised by the immune system and stimulates antibody production.
- appendix - is a gut-associated lymphoid tissue located at the beginning of the colon. The anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis. Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa.
- B lymphocyte (cell) - historically named after a structure called the bursa of Fabricius in birds, a source of antibody-producing lymphocytes. These cells develop in the bone marrow. (More? Electron micrographs of nonactivate and activated lymphocytes)
- BALT - Bronchus Associated Lymphoid Tissue
- band cell - (band neutrophil or stab cell) seen in bone marrow smear, a cell undergoing granulopoiesis, derived from a metamyelocyte, and leading to a mature granulocyte. Also occasionally seen in circulating blood.
- cecum - (caecum, Latin, caecus = "blind") within the gastrointestinal tract a pouch that connects the ileum with the ascending colon of the large intestine.
- cell - has a specific cell biology definition, but is often used instead of "lymphocyte" when describing B and T cells.
- Cell-mediated immunity - the immune function of T lymphocytes.
- "clockface" - a term used to describe the appearance of plasma cell nuclei due to the clumping of the chromatin at the nucleus periphery. More clearly seen in tissue plasma cells that the bone marrow smear, where they are sometimes confused with the basophilic erythroblasts.
- cords of Billroth - spleen cellular columns located in red pulp. surrounded by splenic sinusoids. Cords contain reticular cells, macrophages, lymphocytes, plasma cells and erythrocytes.
- cortex - outer layer, used in association with medulla (innner layer or core) a general description that can be applied to describing an organ with a layered structure.
- Effector cells - the immune functioning (active) B and T lymphocytes.
- Efferent lymph - vessel carrying lymph away from a node.
- GALT - Gut Associated Lymphatic Tissue
- haemopoiesis (hemopoiesis) formation of blood cells.
- Hassall's corpuscle - thymic corpuscle.
- IgA - the main class of antibody in secretions (saliva, tears, milk, and respiratory and intestinal secretions).
- IgD - the immunoglobulin B cell starts to produce as a cell-surface molecule after leaving the bone marrow.
- IgE - bind Fc receptors (surface of mast cells in tissues and basophils in the blood).
- IgG - the major class of immunoglobulin in the blood.
- IgM - the first class of antibody made by a developing B cell, which may switch to making other classes of antibody.
- immunodeficiency - when one or more components of the immune system is defective. (More? Immunobiology - immunodeficiency)
- involution - in the Thymus refers to the replacement, mainly in the cortex, of cells by adipose tissue. (More? PubMed- thymus involution) | Cancer Medicine - Thymomas and Thymic Tumors)
- lamina propria - a layer of loose connective tissue found underneath the epithelium of mucosa.
- Leukocyte- (Greek, lukos= clear, white) white blood cell.
- lingual- related to the tongue.
- lymph node - connective tissue encapsulated lymphoid organ (1mm - 2cm in size), positioned in the pathway of lymph vessels.
- M cell - (microfold cell) found in the follicle-associated epithelium of the Peyer's patch. Function to transport gut lumen organisms and particles to immune cells across the epithelial barrier.
- macrophage - a large highly motile white blood cell which engulfs foreign material (bacteria etc) and both degenerating cells and cell fragments. Found in many different tissues and locations. (More? Immunobiology - Defects in phagocytic cells are associated with persistence of bacterial infection)
- MALT - Mucosa Associated Lymphoid Tissue
- medulla - inner layer or core, used in association with cortex (outer layer) a general description that can be applied to describing an organ with a layered structure.
- Memory Cell - effector T cell (lymphocyte)
- normoblast - seen in bone marrow smear, a developing erythroblast (red blood cell) that still retains a nucleus.
- parenchyma - (Greek = enkeim "to pour in") cells forming the functional cells of an organ or tissue. These cells carry out the function of the organ at a cellular level, and are not the structural cells, connective tissue, extracellular matrix (stromal).
- periarterial lymphoid sheath - (PALS) in the spleen the white pulp that surrounds the central arteries. (T-lymphocytes,macrophages and plasma cells)
- Plasma Cell - active B cell (lymphocyte) which is secreting antibody. Located in either bone marrow or peripheral lymphoid tissues, these cells have and increased cytoplasmic volume (due to increase rough endoplasmic reticulum) in comparison to the inactive (non-secreting) lymphocyte.
- sentinel lymph node - the hypothetical first lymph node or group of nodes reached by metastasizing cancer cells from a primary tumour.
- splenic sinusoids - enlarged spleen capillary spaces located in red pulp and surrounding cords of Billroth.
- stroma - (Greek = "a cover, table-cloth, bedding") tissue forming the framework/support of an organ or tissue. That is the structural cells which form connective tissue and secrete extracellular matrix, rather than the functional cells (parenchymal). All organs can therefore be functionally divided into these 2 components, stromal/parenchymal.
- Subcapsular sinus (=marginal sinus) space lying under the connective tissue capsule which receives lymph from afferent lymphatic vessels.
- Thymic corpuscle (=Hassall's corpuscle) a mass of concentric epithelioreticular cells found in the thymus. The number present and size tend to increase with thymus age. (see classical description of Hammar, J. A. 1903 Zur Histogenese und Involution der Thymusdriise. Anat. Anz., 27: 1909 Fiinfzig Jahre Thymusforschung. Ergebn. Anat. Entwickl-gesch. 19: 1-274.)
- thymic epitheliocytes - reticular cells located in the thymus cortex that ensheathe the cortical capillaries, creating and maintain the microenvironment necessary for the development of T-lymphocytes in the cortex.
- T lymphocyte (cell) - named after thymus, where they develop, the active cell is responsible for cell-mediated immunity. (More? Electron micrographs of nonactivate and activated lymphocytes)
- thymus - thymus has a key role in the development of an effective immune system as well as an endocrine function. Immune system T cells are essential for responses against infections and research relates to the postnatal development of T cells within the thymus. Thymus Development
- tonsils - mucosal-associated lymphoid tissues consists of: 2 palatine tonsils (tonsilla palatina), adenoids (tonsilla pharyngealis) and 1 lingual tonsil (tonsilla lingualis)
- tonsillar ring - ring of lymphoid tissue (tonsils) around where the mouth and nasal cavity meet the throat.
- vermiform appendix - see appendix, anatomical region containing gut-associated lymphoid tissue located within the gastrointestinal tract at the beginning of the colon. The anatomy is as a finger-like structure that arises from the cecum. The length (2.5-13 cm) is longer in both infants and children and also has more abundant lymphatic tissue in early life. The wall structure is similar to the small intestine (though with no villi), nor plicae circularis. Lymph nodules surround the lumen of the gastrointestinal tract and extend from the mucosa into the submucosa.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 19) Embryology SH Lecture - Lymphatic Structure and Organs. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/SH_Lecture_-_Lymphatic_Structure_and_Organs
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G