Prostate Development
Introduction
The male gonad, the testis, differentiates embryonically initially under the influence of the Y chromosome. Later under the influence the gonad-derived fetal testosterone acting through androgen receptors, a region of the urogenital sinus (UGS) mesenchyme differentiates to form the primordial prostate buds. The buds then signal back to the overlying epithelium, inducing duct formation, this was one of the early studied (1970's) example of an mesenchymal-epithelial interaction in development.
The reproductive function of the prostate becomes active at puberty where prostate secretions contribute the majority by volume of the ejaculate containing spermatozoa.
The prostate gland is generally in the news due to its late postnatal adult growth changes, enlarged due to benign nodular hyperplasia, and the male health effects of prostate cancer. Prostate cancer is the second most common malignant tumor in western males and anatomically involves the prostate peripheral zone. (More? "Movember")
There are also currently separate pages describing Genital - Male Development | Spermatozoa Development | Testis Development | Prostate Development.
| Puberty
Some Recent Findings
|
Textbooks
- Human Embryology (2nd ed.) Larson Chapter 10 p261-306
- The Developing Human: Clinically Oriented Embryology (6th ed.) Moore and Persaud Chapter 13 p303-346
- Before We Are Born (5th ed.) Moore and Persaud Chapter 14 p289-326
- Essentials of Human Embryology, Larson Chapter 10 p173-205
- Human Embryology, Fitzgerald and Fitzgerald Chapter 21-22 p134-152
- Developmental Biology (6th ed.) Gilbert Chapter 14 Intermediate Mesoderm
Prostate Development Overview
- fetal testosterone stimulates urogenital sinus mesenchyme through androgen receptors
- urogenital sinus mesenchyme acts on the overlying epithelium to stimulate cell proliferation
- urogenital sinus epithelium then forms prostate ductal progenitor, the prostatic buds
- prostatic buds then grow into the urogenital sinus mesenchyme
Prostate Bud Growth
- specification phase - instructive developmental cues define where buds will form in the UGS
- initiation phase - prostatic buds begin to form
- elongation phase - proliferation, cell adhesion, and cell migration coordinate outgrowth of prostatic buds into UGM.
Based on the recent review.[2]
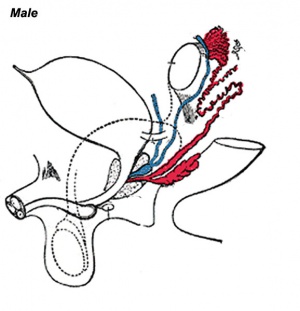
Genital Development Overview
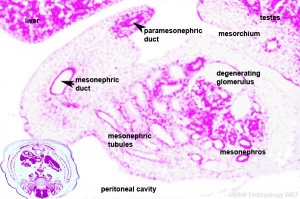
Three main stages during development, mesonephric/paramesonephric duct changes are one of the first male/female differences that occur in development, while external genitaila remain indeterminate in appearance for quite a while.
- Differentiation of gonad (Sex determination)
- Differentiation of internal genital organs
- Differentiation of external genital organs
The 2nd and 3rd stages dependent on endocrine gonad. Reproductive development has a long maturation timecourse, begining in the embryo and finishing in puberty. (More? Puberty Development)
Mouse Prostate Development
The mouse has been used extensively as a model of prostate embryonic development. A similar androgenic regulation occurs of in ventral epithelial bud affecting number and pattern forming in the mouse urogenital sinus.[3]
- begins in fetal mice ductal progenitors (or buds) emerge from urogenital sinus epithelium
- prostatic buds develop in response to androgens, which activate androgen receptors in UGS mesenchyme
- two rows of 3-4 prostatic buds at birth
- Links: Mouse Development
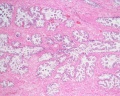
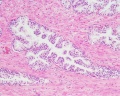
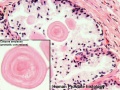
Prostate Histology

|

|
|
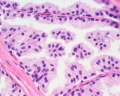
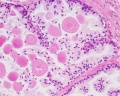
| Human prostate histology | Corpora Amylacea | Submucosal gland |
| (adult, H&E low power overview) | (adult, H&E detail) | (adult, H&E high power detail) |
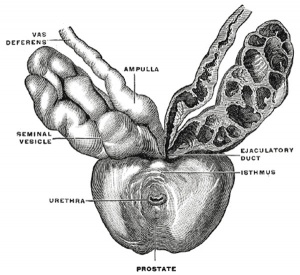
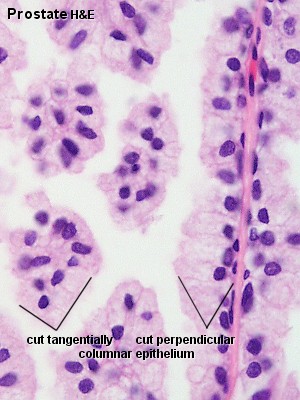
Anatomy
The prostate is the largest accessory sex gland in men (about 2 × 3 × 4 cm). It contains 30 - 50 tubuloalveolar glands, which empty into 15 - 25 independent excretory ducts. These ducts open into the urethra. The glands are embedded into a fibromuscular stroma, which mainly consists of smooth muscle separated by strands of connective tissue rich in collagenous and elastic fibres. The muscle forms a dense mass around the urethra and beneath the fairly thin capsule of the prostrate.
Macroscopically the prostrate can be divided into lobes, but they are inconspicuous in histological sections. In good histological sections it is possible to distinguish three concentric zones, which surround the prostatic part of the urethra.
- peripheral zone contains large (main glands) whose ducts run posteriorly to open into the urethra
- internal zone consists of the so-called submucosal glands
- innermost zone contains mucosal glands
Secretory Glands
The secretory alveoli of the prostate are very irregularly shaped because of papillary projections of the mucosa into the lumen of the gland. The epithelium is cuboidal or columnar. Basal cells are again present, and the epithelium may look pseudostratified where they are found. The secretory cells are slightly acidophilic and secretory granules may be visible in the cytoplasm. Small extensions of the apical cytoplasm into the lumen of the alveoli may represent cells which release their secretory products (secretion is apocrine/merocine). The secretion of the prostate contains citric acid, the enzyme fibrinolysin (liquefies the semen), acid phosphatase, a number of other enzymes and lipids. The secretion of the prostate is the first fraction of the ejaculate.
The secretory ducts of the prostate are lined by a simple columnar epithelium, which changes to a transitional epithelium near the openings of the ducts into the urethra.
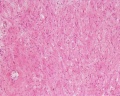
Corpora Amylacea
A characteristic feature of the prostate is the appearance of corpora amylacea in the secretory alveoli. They are rounded eosinophilic bodies. Their average diameter is about 0.25 mm (up to 2 mm). They appear already in the seventh month of foetal development. Their number increases with age - in particular past 50. They may undergo calcification. Corpora amylacea may appear in semen.
Additional Histology Images
- Above text and images modified from: Blue Histology - Prostate
Movies
Genital development animations
| Urogenital Sinus | Urogenital Septum |
| Male External | Testis Descent |
Historic Images of Genital Changes
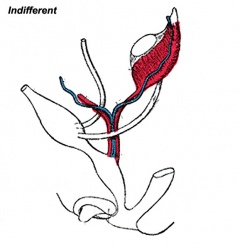
|
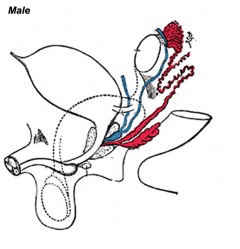
|
|
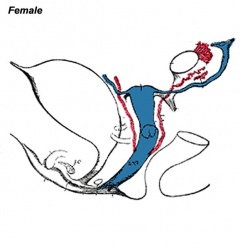
| Urogenital indifferent | Urogenital male | Urogenital female |
Abnormalities
Benign Nodular Hyperplasia
A postnatal adult ageing effect with an onset about 45 years of age, the prostate becomes enlarged due to benign nodular hyperplasia. By 60 years of age and older about 3/4 of the males are affected of which half will be symptomatic. This condition affects the mucosal glands.
Prostate Cancer
Prostate cancer is the second most common malignant tumor in western males and anatomically involves the prostate peripheral zone.
The dog has been used as a model of this condition as this species also spontaneously develop prostatic neoplasia. The cell line CT1258 has been derived from a spontaneous canine prostate carcinoma and can induce tumour formation in mice.
(More? "Movember")
References
Reviews
<pubmed>18801537</pubmed> <pubmed>18752494</pubmed> <pubmed>18557761</pubmed> <pubmed>18462432</pubmed> <pubmed>12645922</pubmed> <pubmed>10506934</pubmed> <pubmed>2577188</pubmed>
Articles
<pubmed>19523480</pubmed> <pubmed>18804104</pubmed> <pubmed>18393306</pubmed> <pubmed>18339840</pubmed> <pubmed>18028901</pubmed> <pubmed>17478449</pubmed> <pubmed>681909</pubmed>
Search PubMed
Search Pubmed "Prostate Embryology" Oct 2010 - All (775) Review (113) Free Full Text (171)
Search Pubmed: Prostate Embryology | Prostate Development | Corpora Amylacea |
Additional Images
Terms
- androgen receptor
- benign prostatic hyperplasia
- mesenchyme
- paraurethral gland - (Skene's gland) - female prostate gland is the correct nomenclature
- prostate gland - Greek, prostates = "one who stands before", "protector", a female prostate gland exists
- prostate cancer
- UGE - urogenital epithelium
- UGS - urogenital sinus
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 19) Embryology Prostate Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Prostate_Development
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G