Ovary Development: Difference between revisions
| Line 40: | Line 40: | ||
Later stages of follicle development are completely absent and will begin to only appear just prior to puberty. | Later stages of follicle development are completely absent and will begin to only appear just prior to puberty. | ||
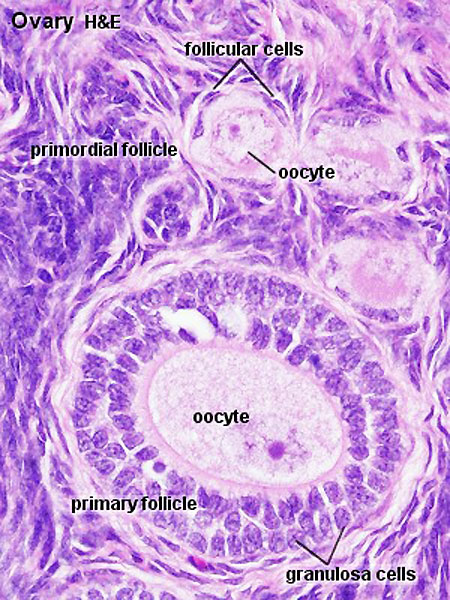
==Adult Follicle Structure== | |||
===Granulosa Cells=== | |||
* A specific cell type that proliferates in association with the oocyte within the developing follicles of the ovary. These cells form the follicle '''stratum granulosa''' and are also given specific names based upon their position within the follicle. | |||
* The '''membrana granulosa''' cells sit on the follicular basal lamina and line the antrum as a stratified epitelium. Following ovulation, these granulosa cells contribute to corpus luteum. | |||
* The '''cumulus oophorus''' is a column of granulosa cells that attaches the oocyte to the follicle wall. At ovulation, this column of cells is broken or separates to release the oocyte from its follicle attachment. | |||
* The '''corona radiata''' are the granulosa cells that directly surround the oocyte, and are released along with it at ovulation. Following ovulation, the corona radiata provide physical protection to the oocyte and are the initial structural barrier that spermatazoa must penetrate during fertilization. | |||
===Theca Interna=== | |||
(Greek, ''thek'' = box) The ovarian follicle endocrine cells forming the inner layer of the theca folliculi surrounding the developing follicle within the ovary. This vascularized layer of cells respond to leutenizing hormone (LH) synthesizing and secreting androgens (androstendione) transported to glomerulosa cells which process initially into testosterone and then by aromatase into estrogen (estradiol). Theca cells do not begin hormonal functions until puberty. | |||
===Theca Externa=== | |||
The ovarian follicle stromal cells forming the outer layer of the theca folliculi surrounding the developing follicle within the ovary. Consisting of connective tissue cells, smooth muscle and collagen fibers. | |||
==References== | ==References== | ||
Revision as of 08:27, 3 May 2010
Introduction
The female gonad is the ovary and is closely associated with female internal genital (reproductive) tract development. In humans, these laterally paired organs lie within the peritoneal cavity. Genes such as Wnt-4 and DAX-1 necessary for initiation of female pathway ovary development, female gonad is not considered a default process.
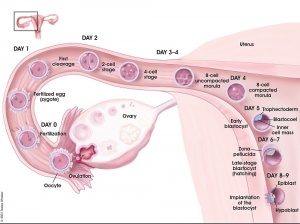
Initial gonad development in females and males is virtually identical with germ cells migrating into an indifferent gonad. In females with XX, the ovary then begins to develop and the subsequent structure and timecourse of germ cell then differs between males and females. In the ovary oocytes proliferate prior to birth and arrest in meiosis 1.
| Menstrual Cycle | X Chromosome | Genital System - Female | Oogenesis
Human Timeline
Approximate Timeline of human development listed below.
24 days - intermediate mesoderm, pronephros primordium
28 days - mesonephros and mesonephric duct
35 days - uteric bud, metanephros, urogenital ridge
42 days - cloacal divison, gonadal primordium (indifferent)
49 days - paramesonephric duct, gonadal differentiation
56 days - paramesonephric duct fusion (female)
100 days - primary follicles (ovary)
Oogenesis
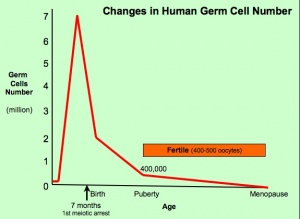
This graph shows the changes in human germ cell numbers in the ovary with age.
Total numbers peak at about 7 million (occuring in early fetal development) and then decreasing by apopotic cell death.
At puberty there remain only about 400,000 and only about 10% of these will be released through reproductive life.
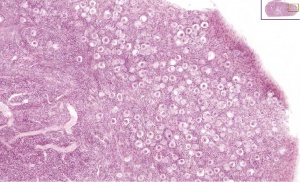
Infant Ovary
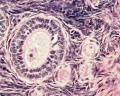
This image shows a region (see inset) of the infant ovary cortex.
There are a large number of developing oocytes which will eventually form a dense primordial germ layer at the ovary periphery.
Later stages of follicle development are completely absent and will begin to only appear just prior to puberty.
Adult Follicle Structure
Granulosa Cells
- A specific cell type that proliferates in association with the oocyte within the developing follicles of the ovary. These cells form the follicle stratum granulosa and are also given specific names based upon their position within the follicle.
- The membrana granulosa cells sit on the follicular basal lamina and line the antrum as a stratified epitelium. Following ovulation, these granulosa cells contribute to corpus luteum.
- The cumulus oophorus is a column of granulosa cells that attaches the oocyte to the follicle wall. At ovulation, this column of cells is broken or separates to release the oocyte from its follicle attachment.
- The corona radiata are the granulosa cells that directly surround the oocyte, and are released along with it at ovulation. Following ovulation, the corona radiata provide physical protection to the oocyte and are the initial structural barrier that spermatazoa must penetrate during fertilization.
Theca Interna
(Greek, thek = box) The ovarian follicle endocrine cells forming the inner layer of the theca folliculi surrounding the developing follicle within the ovary. This vascularized layer of cells respond to leutenizing hormone (LH) synthesizing and secreting androgens (androstendione) transported to glomerulosa cells which process initially into testosterone and then by aromatase into estrogen (estradiol). Theca cells do not begin hormonal functions until puberty.
Theca Externa
The ovarian follicle stromal cells forming the outer layer of the theca folliculi surrounding the developing follicle within the ovary. Consisting of connective tissue cells, smooth muscle and collagen fibers.
References
Search Pubmed: Ovary Development
Additional Images
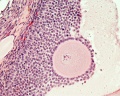
- Monkey-ovary x20he.jpg
Monkey ovary