Nutrition
| Embryology - 25 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose. |
Introduction
This current page is a start page for your exploration of topics related to nutrition and development.
While there are many sites and information available concerning postnatal nutrition, prenatally research has mainly focussed on developmental effects of specific deficiencies (folate and iodine) and the teratogenic effects of retinoic acid.
See Australian Pregnancy Care Guidelines (2018)[1] and also the National Health and Medical Research Council (NHMRC) (2006) publication NHMRC - Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes.[2] "The Nutrient Reference Values outline the levels of intake of essential nutrients considered to be adequate to meet the known nutritional needs of practically all healthy people for prevention of deficiency states. The document can be used by health professionals to assess the likelihood of inadequate intake in individuals or groups of people." Some text on this current page is modified from this report.
In Australia and New Zealand
Before mandatory folic acid fortification was introduced:
- mean dietary folic acid intakes for women aged 16–44 years (the target population) in Australia was 108 micrograms (μg) of folic acid per day and in New Zealand was 62 μg of folic acid per day, well below the recommended 400 μg per day.
- there were 149 pregnancies affected by NTDs in 2005 in Australia (rate of 13.3 per 10,000 births) in the three states that provide the most accurate baseline of NTD incidence (South Australia, Western Australia and Victoria), and 63 pregnancies affected by NTDs in 2003 in New Zealand (rate of 11.2 per 10,000 births).
Before mandatory iodine fortification was introduced:
- large proportions of the Australian and New Zealand population had inadequate iodine intakes.
- national surveys measuring median urinary iodine concentration (MUIC) in schoolchildren, an indicator of overall population status, confirmed mild iodine deficiency in both countries.
- the concentration was 96 μg per litre in Australia, and 66 μg per litre in New Zealand, less than the 100–200 μg per litre considered optimal.
The Nobel Prize in Chemistry 1937 Walter Norman Haworth "for his investigations on carbohydrates and vitamin C" and Paul Karrer "for his investigations on carotenoids, flavins and vitamins A and B2".
| Nutrition Links: nutrition | Vitamin A | Vitamin B | Vitamin C | Vitamin D | Vitamin E | Vitamin K | folate | iodine deficiency | neural abnormalities | Axial Skeleton Abnormalities |
Some Recent Findings
In this study, we aimed to compare serum 25(OH)D levels in women with and without gestational diabetes mellitus (GDM), and to identify the serum 25(OH)D levels associated with GDM. We recruited 40 women with GDM and 40 healthy pregnant women, aged 20-40 years and in the second trimester, at Gulhane Education and Research Hospital. We excluded women with chronic diseases, preeclampsia, pre-GDM, multiple pregnancies, and those taking medications related to calcium or vitamin D metabolism. We took anthropometric measurements and blood samples during the second trimester. Of the 80 pregnant women, pre-pregnancy body mass index was significantly higher among the GDM group than the healthy group (26.4 ± 5.73 kg/m2 vs. 22.6 ± 3.56 kg/m2, p = .001). Serum 25(OH)D levels in women with GDM were significantly lower than those in healthy women (16.8 ± 9.90 ng/mL vs. 20.9 ± 8.16 ng/mL, p = .016). The prevalence of severe vitamin D deficiency was as high as 72.5% among women in the GDM group, with a 1.74-fold increased risk of deficient status. Levels of 25(OH)D lower than a cutoff value of 14.0 ng/mL were determined to be related to GDM. These study results suggest that maternal vitamin D deficiency in mid-pregnancy is significantly associated with development of GDM."
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Fetal Nutrition <pubmed limit=5>Fetal Nutrition</pubmed> |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
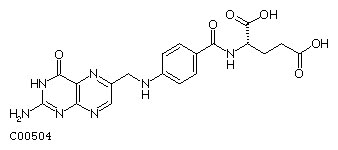
Folic Acid
| In 2001, the Australian estimated birth prevalence of neural tube defects was 0.5 per 1,000 births (National Perinatal Statistics Unit). Low maternal dietary Vitamin B9 as folic acid (folate, folacin) has been shown to be associated with the development of neural tube defects. |
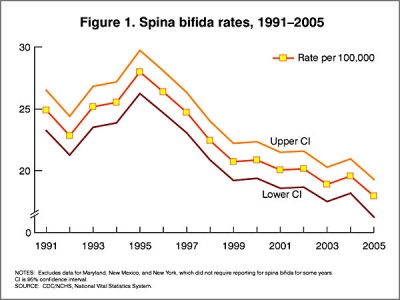
In the U.S.A. the Food and Drug Administration in 1996 authorized that all enriched cereal grain products be fortified with folic acid, with optional fortification beginning in March 1996 and mandatory fortification in January 1998.
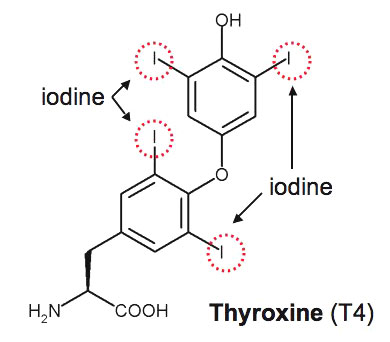
Iodine
|
Thyroxine (T4) molecular structure showing iodine positions (red rings) |
"Iodine is an essential nutrient that humans need in very small quantities. The thyroid uses iodine to produce hormones vital to ensure normal development of the brain and nervous system before birth, in babies and young children. For this reason, it is very important that pregnant and breastfeeding women get enough iodine. The National Health and Medical Research Council recommends that all women who are pregnant, breastfeeding or considering pregnancy, take an iodine supplement of 150 micrograms (μg) each day. Women with pre-existing thyroid conditions should seek advice from their medical practitioner prior to taking a supplement."
|
- Links: iodine deficiency | Iodine supplementation for Pregnant and Breastfeeding Women NHMRC - Nutrition & Diet Publications
Vitamins
Australian 2018 Pregnancy Care Guidelines[1]
- "Supplements of vitamins A, C and E are not of benefit during pregnancy and may cause harm"
There are several different vitamins with a standardised classification by a letter and number.
Vitamin A
Retinoic acid is a metabolite of Vitamin A (retinol) and may affect prenatal development. Postnatal dietary supplementation of children is recommended when diet may be inadequate. Vitamin A is required for many systems including: visual system, cell function for growth, epithelial integrity, red blood cell production, immunity, and reproduction.
The following text is from a review of published data.[12]
What is already known on this topic
- Vitamin A is an essential nutrient; it must be obtained through diet
- In low and middle income countries, many people (especially children) do not eat enough vitamin A
- Vitamin A deficiency is related to vision problems and increased susceptibility to infectious disease and death
- WHO recommends vitamin A supplements for children, pregnant women, and breastfeeding mothers
What this study adds
- There have been 43 trials of vitamin A for children aged 6 months to 5 years old, including about 215,633 children
- In low and middle income countries, vitamin A supplementation is associated with a 24% reduction in mortality
- Vitamin A supplementation might reduce mortality by preventing measles and diarrhoea; it also prevents blindness
- The evidence for vitamin A is compelling and clear; further trials comparing vitamin A with placebo would be unethical
- spermatozoa - "Retinoic acid appears to act in a pulsatile manner, periodically driving spermatogonial differentiation and meiotic onset at discrete points along testis tubules, and as a result, is likely to be responsible for generating and maintaining the cycle of the seminiferous epithelium."[13]
Vitamin B
The Vitamin B group consists of eight separate water-soluble vitamins that play important roles in cell metabolism. See also Folic Acid
Vitamin B3
Vitamin B3 (niacin, nicotinic acid, nicotinamide) A recent Spanish study of dietary intake of vitamins during pregnancy and risk of having a small for gestational age (SGA) newborn, showed a protective effect vitamin B3 and B6.[14] Using 3 mouse models of preeclampsia, vitamin B3 alleviated or prevented miscarriage, prolonged pregnancy period, and improved the growth of the fetuses.[15]
Vitamin B3 and L-tryptophan together are the main dietary precursors for synthesis of nicotinamide adenine dinucleotide (NAD), a key cofactor in many cellular metabolic processes.
Vitamin B9
Vitamin B9 (folacin, Folic acid) and folate the naturally occurring form, are an important dietary requirement for normal neural development. Low levels have been show associated with neural tube defects including spina bifida.
Vitamin B12
Vitamin B12 has been shown to enhances TBX1 gene expression that can improve DiGeorge syndrome (velocardiofacial syndrome) outcomes in the mouse model of the disease.[16]
Abnormalities - Pernicious anaemia is an autoimmune condition that results in an inability to absorb vitamin B12.
- Links: Folic Acid and Neural Tube Defects | DiGeorge syndrome | Neural System - Abnormalities | Neural System Development
Vitamin C
Ascorbic acid (vitamin C) is necessary for the formation of collagen, reducing free radicals, and aiding in iron absorption. Scurvy is a disease of dietary ascorbic acid deficiency that is very uncommon today, except in economically disadvantaged populations with poor nutrition. Occurance in children is very rare and can lead to musculoskeletal abnormalities, and has also been seen in neurologic illness.[17]
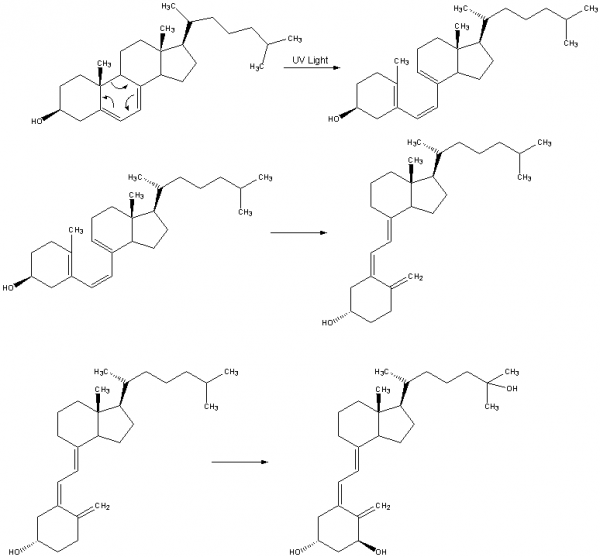
Vitamin D
Vitamin D3 is produced in the skin from 7-dehydrocholesterol in a photoreaction induced by ultraviolet B (UVB) radiation from the sun. This is then released into circulation where it is hydroxylated in the liver and kidney to a more active form. Circulating 25-hydroxyvitamin D3 (25[OH]D), the most commonly used index of vitamin D status, is converted to the active hormone 1,25 dihydroxyvitamin D3 (1,25[OH]2D), which, operating through the vitamin D receptor (VDR). The vitamin D receptor belongs to the nuclear receptor superfamily and singling regulates calcium homeostasis. (See 2008 review[18])
| Tissue | Substrate | Product |
|---|---|---|
| Integument | 7-dehydrocholesterol | Vitamin D3 |
| Liver | Vitamin D3 | 25-hydroxyvitamin D3 (calcidiol) |
| Kidney | 25-hydroxyvitamin D3 | 1,25-dihydroxyvitamin D3 (calcitriol, 1α,25-dihydroxyvitamin D) |
In the skin Vitamin D3 regulates both epidermal proliferation and differentiation. As a circulating hormone, it regulates calcium levels in the blood, required for bone and muscle development.
USA Institute of Medicine expert committee "calcium requirements varied with age, from 700 mg a day for children aged 1-3 years up to 1200 mg a day for women aged 51 to 70 and 1300 mg a day for teenagers and pregnant and lactating women."
- Australia - Newborn-serum 25OHD concentrations depend on the maternal circulating plasma 25OHD level at least during the third trimester. Neonatal 25OHD levels obtained by EIA correlated well with liquid chromatography/tandem mass spectrometry (LC-MSMS). Although the EIA values for neonates were greater than LC-MSMS values, this difference was not statistically significant.[19]
- UK - Avoidance of vitamin D deficiency in pregnancy in the United Kingdom: the case for a unified approach in National policy.[20]
- USA 2004 - Vitamin D requirements during pregnancy.[21]
The vitamin D receptor (VDR) is found on most non-skeletal human cells that may indicate a role in more than the bone and calcium metabolism.[22]
- respiratory tract is a consequence of its activity in the immune system.
- vitamin D deficiency occurs with gastrointestinal diseases such as inflammatory bowel disease, coeliac disease, liver, pancreas or cardiac diseases.
- links to diabetes. VDR and 1α-hydroxylase have been detected in the cutaneous capillary vessels, endothelium, vascular smooth muscles, myocytes and cardiac fibroblasts.
| Kidney Endocrine | ||
|---|---|---|
| Hormone | Function | Comment |
| Renin | increase angiotensin-aldosterone system | paracrine, renin is released by juxtaglomerular cells |
| Prostaglandins | decrease sodium (Na+) reabsorption | paracrine, (PGE2) vasodilator regulate renal vascular reactivity |
| Erythropoietin | increase Erythrocyte production | endocrine, promotes red blood cell formation in bone marrow |
| 1,25 (OH)2 vitamin D | Calcium homeostasis | endocrine, biologically active form of vitamin D |
| Prekallikreins | increase Kinin production | paracrine, act locally to induce vasodilation and contraction of smooth muscle |
Calcium - For women with low dietary intake and high risk of pre-eclampsia, increased intake of calcium-rich foods or supplements may be beneifcial. (Australian Guideline 2018[1])
- Links: Vitamin D3 | Vitamin D3 synthesis | Integumentary | Nutrition | Endocrine Kidney | Parathyroid
Dietary Reference Intakes for Calcium and Vitamin D | Paediatric Endocrine Group; Paediatric Bone Australasia. Prevention and treatment of infant and childhood vitamin D deficiency in Australia and New Zealand: a consensus statement (2006) [23]
Vitamin E
Vitamin E has a role in immunity and cell function (controls free radicals mediated disturbances and maintains membrane integrity). Animal studies suggest a protective role for asthma risk.[24]
Tocotrienols are natural compounds acting as dietary members of the vitamin E family.[24] They are found in a number of vegetable oils, wheat germ, barley, and certain types of nuts and grains.
Vitamin K
A generic term for derivatives of 2-methyl-1,4-naphthoquinone that have coagulation activity. Daily requirement for vitamin K is about 1 µg/kg. In newborns vitamin K nutrition is at risk.
- Required for synthesis of prothrombin and proconvertin (stable factor, factor VII).
- May also be involved in synthesis of Stuart-Prower factor (factor X) and PTC (plasma thromboplastic factor, factor IX) since clotting defects due to deficiencies of these factors as well as to deficiencies of prothrombin and proconvertin occur in states of vitamin K deficiency.
- CDC finds cluster of newborns in Tennessee with bleeding disorder Report highlights importance of vitamin K shot at birth.
Iron
Maternal iron (Fe) deficiency can be a common disorder during pregnancy and also in the postnatal period for neonatal neural development. Haemoglobin is the iron-containing oxygen-transport metalloprotein located in maternal and fetal red blood cells and myoglobin is the equivalent protein located in muscle. Iron is also required in some cellular enzymatic processes as a cofactor.
During pregnancy the maternal blood volume increases and the packed cell volume and haemoglobin (Hb) concentration can fall, a condition is known as "anaemia of pregnancy" (haemoglobin value below 11 g/dL). Therefore an increase of about 50% above the recommended daily dietary intake of Fe is suggested during pregnancy. [25] Preventive treatment can include prophylaxis iron supplements and food fortification with iron.[26]
Fetal demands for iron are maximal during the third trimester. Prenatal maternal use of iron can also improve birth weight, in a linear dose-response fashion, perhaps reducing the risk of low birth weight.[27]
Similar micronutrient requirements have been identified for other trace metals such as copper (Cu), see the review.[28]
Australian 2018 Pregnancy Care Guidelines[1]
- Increasing intake of iron-rich foods reduces the risk of iron deficiency
- Unnecessary iron supplementation offers no benefit and has side effects at higher doses
- For women with low dietary intake, intermittent supplementation is as effective as daily supplementation in preventing iron-deficiency anaemia, with fewer side effects
- For women with identified iron-deficiency anaemia, low-dose supplementation is as effective as high dose, with fewer side effects
Calcium
For women with low dietary intake and high risk of pre-eclampsia, increased intake of calcium-rich foods or supplements may be beneifcial. (Australian Guideline 2018[1])
Protein
There are normally 20 amino acids found in proteins, some of which can be made by the body while nine are essential (unable to synthesise from simpler molecules) in the diet. Modified amino acids are the basis of several hormones, such as noradrenaline (norepinepherine), adrenalin (epinepherine) and thyroid hormone. (More? Endocrine System Development)
Essential amino acids
- histidine
- isoleucine
- leucine
- lysine
- methionine
- phenylalanine
- threonine
- tryptophan
- valine
Cysteine and tyrosine can partly replace methionine and phenylalanine.
Fats
- Fats are the highest form of energy for the body.
- Aid in the absorption of the fat-soluble vitamins (A, D, E and K) and other fat-soluble biologically-active components.
- Three major types of naturally-occurring fatty acids:
- saturated - mainly in animal-based foods. For example, found in milk, cream, butter and cheese, land animal meats.
- cis-monounsaturated - mainly in plant-based foods. For example, oleic acid found in olive, canola and peanut oils.
- cis-polyunsaturated - mainly in plant-based foods. For example, linoleic acid found in seed oils, eg sunflower, safflower and corn.
- trans fatty acids are produced by partial hydrogenation of polyunsaturated oils in food processing and also occur in ruminant animal foods.
Carbohydrates
- Dietary carbohydrate provides energy to specific tissues, for example the brain requires glucose.
- Note, infant's brain is large relative to body size and uses 60% of the infant’s total energy intake.
Fibre
- Dietary fibre is essential for proper gut function
- Related also to risk reduction for some chronic diseases (heart disease, certain cancers and diabetes).
Water
- Water is essential because it is required in quantities above the body’s production.
- Water loss from lungs and skin are responsible for 50% of total water turnover.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Department of Health (2018) Clinical Practice Guidelines: Pregnancy Care. Canberra: Australian Government Department of Health. (5 June 2019)
- ↑ 'Nutrient Reference Values for Australia and New Zealand Including Recommended Dietary Intakes. (2006) http://www.nhmrc.gov.au/publications/synopses/n35syn.htm PDF
- ↑ Ede G, Keskin U, Cemal Yenen M & Samur G. (2019). Lower vitamin D levels during the second trimester are associated with developing gestational diabetes mellitus: an observational cross-sectional study. Gynecol. Endocrinol. , , 1-4. PMID: 30599810 DOI.
- ↑ McCarthy EK, Murray DM, Malvisi L, Kenny LC, O'B Hourihane J, Irvine AD & Kiely ME. (2018). Antenatal Vitamin D Status Is Not Associated with Standard Neurodevelopmental Assessments at Age 5 Years in a Well-Characterized Prospective Maternal-Infant Cohort. J. Nutr. , , . PMID: 30169669 DOI.
- ↑ Baker BC, Hayes D & Jones RL. (2018). Effects of micronutrients on placental function: evidence from clinical studies to animal models. Reproduction , , . PMID: 29844225 DOI.
- ↑ Louvigne M, Rouleau S, Caldagues E, Souto I, Montcho Y, Bouvagnet AM, Baud O, Carel JC, Gascoin G & Coutant R. (2018). Association of maternal nutrition with transient neonatal hyperinsulinism. PLoS ONE , 13, e0195383. PMID: 29723237 DOI.
- ↑ Josefson JL, Reisetter A, Scholtens DM, Price HE, Metzger BE & Langman CB. (2016). Maternal BMI Associations with Maternal and Cord Blood Vitamin D Levels in a North American Subset of Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study Participants. PLoS ONE , 11, e0150221. PMID: 26942930 DOI.
- ↑ Gürke J, Hirche F, Thieme R, Haucke E, Schindler M, Stangl GI, Fischer B & Navarrete Santos A. (2015). Maternal Diabetes Leads to Adaptation in Embryonic Amino Acid Metabolism during Early Pregnancy. PLoS ONE , 10, e0127465. PMID: 26020623 DOI.
- ↑ Čapo I, Hinić N, Lalošević D, Vučković N, Stilinović N, Marković J & Sekulić S. (2015). Vitamin C Depletion in Prenatal Guinea Pigs as a Model of Lissencephaly Type II. Vet. Pathol. , 52, 1263-71. PMID: 25487414 DOI.
- ↑ Kositamongkol S, Suthutvoravut U, Chongviriyaphan N, Feungpean B & Nuntnarumit P. (2011). Vitamin A and E status in very low birth weight infants. J Perinatol , 31, 471-6. PMID: 21233795 DOI.
- ↑ NHMRC - Iodine supplementation for Pregnant and Breastfeeding Women 2010 [1]
- ↑ Mayo-Wilson E, Imdad A, Herzer K, Yakoob MY & Bhutta ZA. (2011). Vitamin A supplements for preventing mortality, illness, and blindness in children aged under 5: systematic review and meta-analysis. BMJ , 343, d5094. PMID: 21868478
- ↑ Hogarth CA & Griswold MD. (2013). Retinoic acid regulation of male meiosis. Curr Opin Endocrinol Diabetes Obes , 20, 217-23. PMID: 23511242 DOI.
- ↑ Salcedo-Bellido I, Martínez-Galiano JM, Olmedo-Requena R, Mozas-Moreno J, Bueno-Cavanillas A, Jimenez-Moleon JJ & Delgado-Rodríguez M. (2017). Association between Vitamin Intake during Pregnancy and Risk of Small for Gestational Age. Nutrients , 9, . PMID: 29168736 DOI.
- ↑ Takahashi N, Li F, Fushima T, Oyanagi G, Sato E, Oe Y, Sekimoto A, Saigusa D, Sato H & Ito S. (2018). Vitamin B3 Nicotinamide: A Promising Candidate for Treating Preeclampsia and Improving Fetal Growth. Tohoku J. Exp. Med. , 244, 243-248. PMID: 29563389 DOI.
- ↑ Lania G, Bresciani A, Bisbocci M, Francone A, Colonna V, Altamura S & Baldini A. (2017). Vitamin B12 ameliorates the phenotype of a mouse model of DiGeorge syndrome. Hum. Mol. Genet. , 26, 4540. PMID: 29036321 DOI.
- ↑ Noble JM, Mandel A & Patterson MC. (2007). Scurvy and rickets masked by chronic neurologic illness: revisiting "psychologic malnutrition". Pediatrics , 119, e783-90. PMID: 17332193 DOI.
- ↑ Stroud ML, Stilgoe S, Stott VE, Alhabian O & Salman K. (2008). Vitamin D - a review. Aust Fam Physician , 37, 1002-5. PMID: 19142273
- ↑ Thomas SD, Fudge AN, Whiting M & Coates PS. (2011). The correlation between third-trimester maternal and newborn-serum 25-hydroxy-vitamin D in a selected South Australian group of newborn samples. BMJ Open , 1, e000236. PMID: 22021888 DOI.
- ↑ Hyppönen E & Boucher BJ. (2010). Avoidance of vitamin D deficiency in pregnancy in the United Kingdom: the case for a unified approach in National policy. Br. J. Nutr. , 104, 309-14. PMID: 20594390 DOI.
- ↑ Specker B. (2004). Vitamin D requirements during pregnancy. Am. J. Clin. Nutr. , 80, 1740S-7S. PMID: 15585798
- ↑ Gruber BM. (2015). [The phenomenon of vitamin D]. Postepy Hig Med Dosw (Online) , 69, 127-39. PMID: 25614680
- ↑ Munns C, Zacharin MR, Rodda CP, Batch JA, Morley R, Cranswick NE, Craig ME, Cutfield WS, Hofman PL, Taylor BJ, Grover SR, Pasco JA, Burgner D & Cowell CT. (2006). Prevention and treatment of infant and childhood vitamin D deficiency in Australia and New Zealand: a consensus statement. Med. J. Aust. , 185, 268-72. PMID: 16948623
- ↑ 24.0 24.1 Cook-Mills JM & Avila PC. (2014). Vitamin E and D regulation of allergic asthma immunopathogenesis. Int. Immunopharmacol. , 23, 364-72. PMID: 25175918 DOI.
- ↑ Stoltzfus RJ, Dreyfuss ML. Guidelines for the Use of Iron Supplements to Prevent and Treat Iron Deficiency Anemia. (1998) Geneva, Switzerland: International Nutritional Anemia Consultative Group [UNICEF/WHO http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/1-57881-020-5/en/ PDF]
- ↑ Osungbade KO & Oladunjoye AO. (2012). Preventive treatments of iron deficiency anaemia in pregnancy: a review of their effectiveness and implications for health system strengthening. J Pregnancy , 2012, 454601. PMID: 22848829 DOI.
- ↑ Haider BA, Olofin I, Wang M, Spiegelman D, Ezzati M & Fawzi WW. (2013). Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta-analysis. BMJ , 346, f3443. PMID: 23794316
- ↑ Bailey LB, Stover PJ, McNulty H, Fenech MF, Gregory JF, Mills JL, Pfeiffer CM, Fazili Z, Zhang M, Ueland PM, Molloy AM, Caudill MA, Shane B, Berry RJ, Bailey RL, Hausman DB, Raghavan R & Raiten DJ. (2015). Biomarkers of Nutrition for Development-Folate Review. J. Nutr. , 145, 1636S-1680S. PMID: 26451605 DOI.
Reviews
Franasiak JM, Lara EE & Pellicer A. (2017). Vitamin D in human reproduction. Curr. Opin. Obstet. Gynecol. , 29, 189-194. PMID: 28562440 DOI.
Bailey LB, Stover PJ, McNulty H, Fenech MF, Gregory JF, Mills JL, Pfeiffer CM, Fazili Z, Zhang M, Ueland PM, Molloy AM, Caudill MA, Shane B, Berry RJ, Bailey RL, Hausman DB, Raghavan R & Raiten DJ. (2015). Biomarkers of Nutrition for Development-Folate Review. J. Nutr. , 145, 1636S-1680S. PMID: 26451605 DOI.
Leung BM, Wiens KP & Kaplan BJ. (2011). Does prenatal micronutrient supplementation improve children's mental development? A systematic review. BMC Pregnancy Childbirth , 11, 12. PMID: 21291560 DOI.
Articles
Bolland MJ, Grey A & Cundy T. (2012). Vitamin D and health in adults in Australia and New Zealand: a position statement. Med. J. Aust. , 197, 553; author reply 553-4. PMID: 23163681
Berry RJ, Bailey L, Mulinare J & Bower C. (2010). Fortification of flour with folic acid. Food Nutr Bull , 31, S22-35. PMID: 20629350 DOI.
Books
- Institute of Medicine (US) Panel on Micronutrients. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. Washington (DC): National Academies Press (US); 2001. Available from: http://www.ncbi.nlm.nih.gov/books/NBK222310/
Search Pubmed
Terms
- Adequate Intake - (AI) The average daily nutrient intake level based on observed or experimentally-determined approximations or estimates of nutrient intake by a group (or groups) of apparently healthy people that are assumed to be adequate. Used when an RDI cannot be determined.
- Estimated Average Requirement - (EAR) A daily nutrient level estimated to meet the requirements of half the healthy individuals in a particular life stage and gender group.
- Median Urinary Iodine Concentration - (MUIC) Urinary iodine concentration is the prime indicator of nutritional iodine status and is used to evaluate population-based iodine supplementation. The median value is determined from a population sample.
- Recommended Dietary Intake - (RDI) The average daily dietary intake level that is sufficient to meet the nutrient requirements of nearly all (97–98 per cent) healthy individuals in a particular life stage and gender group.
- Transient hypoglycemia - Refers to a slow or immature fasting adaptation process. often related to conditions or events occurring during birth and can occur during the first hours of life.
- Upper Level of Intake - (UL) The highest average daily nutrient intake level likely to pose no adverse health effects to almost all individuals in the general population. As intake increases above the UL, the potential risk of adverse effects increases.
- Urinary Iodine Concentration - (UIC)
- Some terms from NHMRC publication, adapted from Food and Nutrition Board: Institute of Medicine (USA and Canada).
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- World Health Organization (WHO)
- USA NIH
- Medline Plus Infant and Newborn Nutrition
- Australia NHMRC
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 25) Embryology Nutrition. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Nutrition
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G