Musculoskeletal System - Pelvis Development
| Embryology - 16 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
The pelvis is a developmentally complex skeletal structure requiring the fusion of separate elements and articulation with both the axial skeleton and lower limb. Postnatally, the human upright posture has also placed highly species specific physical demands on this structure. Developmental dysplasia of the hip is also one of the 3 most common (along with cleft palate, cleft lip) skeletal abnormalities.
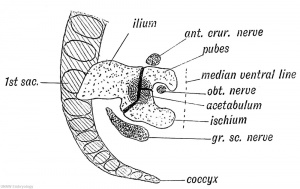
The skeletal pelvis consists of: the sacrum and coccyx (axial skeleton), and pelvic girdle formed by a pair of hip bones (appendicular skeleton). Before puberty, he pelvic girdle also consists of three unfused bones: the ilium, ischium, and pubis. In chicken, the entire pelvic girdle originates from the somatopleure mesoderm (somite levels 26 to 35) and the ilium, but not of the pubis and ischium, depends on somitic and ectodermal signals.[1]
The mesoderm forms nearly all the connective tissues of the musculoskeletal system. Each tissue (cartilage, bone, and muscle) goes through many different mechanisms of differentiation.
The musculoskeletal system consists of skeletal muscle, bone, and cartilage and is mainly mesoderm in origin with some neural crest contribution.
The intraembryonic mesoderm can be broken into paraxial, intermediate and lateral mesoderm relative to its midline position. During the 3rd week the paraxial mesoderm forms into "balls" of mesoderm paired either side of the neural groove, called somites.
Somites appear bilaterally as pairs at the same time and form earliest at the cranial (rostral,brain) end of the neural groove and add sequentially at the caudal end. This addition occurs so regularly that embryos are staged according to the number of somites that are present. Different regions of the somite differentiate into dermomyotome (dermal and muscle component) and sclerotome (forms vertebral column). An example of a specialized musculoskeletal structure can be seen in the development of the limbs.
Skeletal muscle forms by fusion of mononucleated myoblasts to form mutinucleated myotubes. Bone is formed through a lengthy process involving ossification of a cartilage formed from mesenchyme. Two main forms of ossification occur in different bones, intramembranous (eg skull) and endochondrial (eg limb long bones) ossification. Ossification continues postnatally, through puberty until mid 20s. Early ossification occurs at the ends of long bones.
The pelvis is also covered in some urogenital studies.[2][3][4][5] Musculoskeletal and limb abnormalities are also one of the largest groups of congenital abnormalities.
See also the Anatomical Record - Special Issue:The Human Pelvis: Anatomy, Development and Function (April 2017).[6]
- Links: pelvis | shoulder | appendicular skeleton | axial skeleton
| Historic Pelvis |
|---|
|
Thomson A. The sexual differences of the fetal pelvis. (1899) J Anat Physiol. 33(3): 359-380. Ruth EB. A study of the development of the mammalian pelvis. (1932) Anat. Rec. 53(2): 208 - |
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Note this search term may result in listing some papers related to renal development. Search term: Pelvis Embryology | Pelvis Development |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page. |
Textbooks
- The Developing Human: Clinically Oriented Embryology (8th Edition) by Keith L. Moore and T.V.N Persaud - Moore & Persaud Chapter 15 the skeletal system
- Larsen’s Human Embryology by GC. Schoenwolf, SB. Bleyl, PR. Brauer and PH. Francis-West - Chapter 11 Limb Dev (bone not well covered in this textbook)
- Before we Are Born (5th ed.) Moore and Persaud Chapter 16,17: p379-397, 399-405
- Essentials of Human Embryology Larson Chapter 11 p207-228
Timeline
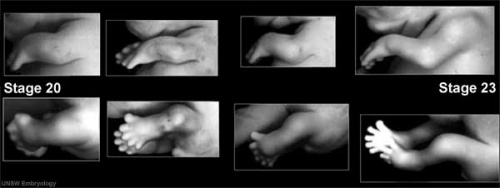
The following timeline data comes from a recent CT and MRI study of late human embryos from the Kyoto Collection.[8]
| Carnegie Stage | Event |
|---|---|
| 18 | chondrification centres of the ilium, ischium, and pubis first appears. Located around the acetabulum and grew radially. |
| 20 | iliac crest formed while the iliac body's central part remained chondrified. |
| 22 | Sacroiliac joint forms. |
| 22 | Iliac body is discoid. The growth rate was greater in the ilium than in the sacrum-coccyx, pubis, and ischium. |
| 23 | Articulation of the pubic symphysis, connection of the articular column in the sacrum, and Y-shape connection of the three parts of the hip bones to the acetabulum. |
| Early Fetal | connection of the ischium and pubic ramus. |
| Data from human CT and MRI study.[8] | |
| Links: pelvis | pelvis timeline | joint | limb | timeline | |
Muscle Development (Myogenesis)
- Early myogenic progenitor cells in the dermomyotome can be initially identified by the transcription factor Pax3.
- Subsequent myogenic program development then depends on the myogenic determination factors (Myf5, MyoD, and MRF4), both Myf5 and MyoD are expressed in the limbs.
- Final differentiation of these cells into post-mitotic muscle fibers in the limb bud is regulated by another myogenic determination factor, Myogenin.
(Some of the above text modified from[10]
Links: Muscle Development
Limb Bone
Bone formation within the limb occurs by endochondral ossification of a pre-existing cartilage template. Ossification then replaces the existing cartilage except in the regions of articulation, where cartilage remains on the surface of the bone within the joint. Therefore bone development in the limb is initially about cartilage development or chondrogenesis.
In addition, there are two quite separate aspects to this development.
- Pattern - where the specific regions will commence to form cartilage, which will be different for each cartilage element.
- Chondrogenesis - the differentiation of mesoderm to form cartilage, which will be essentially the same program for all cartilage templates.
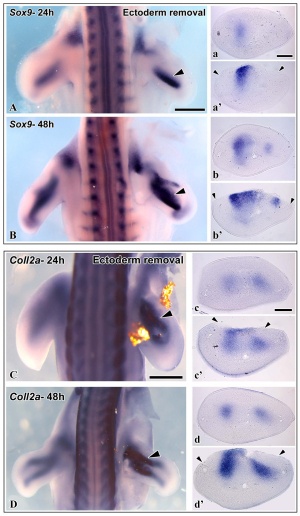
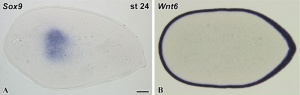
A recent study has identified that the overlying limb surface ectoderm potentially inhibits limb early chondrogenesis through Wnt6 signaling.[11]
Links: Cartilage Development | Bone Development
Molecular
Fibroblast Growth Factors
T-box Transcription Factors
Abnormalities
| ICD-11 |
|---|
| LB74 Structural developmental anomalies of pelvic girdle - LB74.0 Developmental dysplasia of hip
LB74.1 Congenital subluxation of hip | LB74.2 Unstable hip | LB74.3 Congenital coxa vara | LB74.4 Congenital coxa valga | LB74.5 Wide symphysis pubis | LB74.Y Other specified structural developmental anomalies of pelvic girdle | LB74.Z Structural developmental anomalies of pelvic girdle, unspecified |
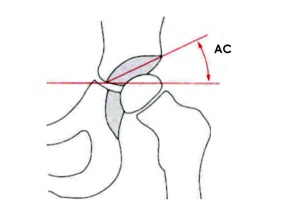
Developmental Dysplasia of the Hip
| ICD-11 LB74.0 Developmental dysplasia of hip |
- A condition caused by failure of the hip to correctly develop during the antenatal period. This condition is characterized by slippage of the hip from the socket. This condition may present with outward turning of the leg, reduced movement on one side of the body, shortness of one leg, uneven skin folds on thigh or buttocks, walking difficulties, or inward rounding of the lower back.
Developmental dysplasia of the hip ((DDH) or congenital hip dislocation is one of the 3 most common skeletal abnormalities and can range from unilateral or bilateral instability to complete dislocation at the femur acetabulum of the lower limb. See the recommendation statement for screening for developmental dysplasia of the hip.[14]
- Instability: 1:60 at birth; 1:240 at 1 wk: Dislocation untreated; 1:700
- congenital instability of hip, later dislocates by muscle pulls or gravity
- familial predisposition female predominance
- Growth of femoral head, acetabulum and innominate bone are delayed until the femoral head fits firmly into the acetabulum.
Barlow test
(Barlow maneuver) A clinical term to describe a physical examination of the newborn for Developmental dysplasia of the hip (DDH). The examiner adducts the hip (bringing the thigh towards the midline) while applying light pressure on the knee, directing the force posteriorly. A positive sign is the hip being dislocatable, if the hip can be popped out of socket with this test. This test is then combined with the Ortolani test (manoeuvre). The test is named after Thomas Barlow (1845 – 1945) a British royal physician.
Ortolani test
(Ortolani manoeuvre) A clinical term to describe a physical examination of the newborn for developmental dysplasia of the hip (DDH). This is a test for posterior dislocation of the hip. Using the examiner's thumb, abduct the infant's leg, while using the examiner's index finger to place anterior pressure on the greater trochanter. A positive sign is a distinctive 'clunk' which can be heard and felt as the femoral head relocates anteriorly into the acetabulum, usually becomes negative after 2 months of age. This test is combined with the Barlow test (maneuver). Named after Marino Ortolani, the test developer in 1976.
Abduction Splints
There is variable evidence for the use of abduction splinting during onset of walking in children on the maturation of mild dysplastic hips.[13]
Shoulder
The skeletal shoulder consists of: the clavicle (collarbone), the scapula (shoulder blade), and the humerus. Development of his region occurs through both forms of ossification processes.
- Links: shoulder
References
- ↑ Malashichev Y, Christ B & Pröls F. (2008). Avian pelvis originates from lateral plate mesoderm and its development requires signals from both ectoderm and paraxial mesoderm. Cell Tissue Res. , 331, 595-604. PMID: 18087724 DOI.
- ↑ Pillet J. Reconstruction des organes pelviens d’embryons humains de 12,5 et de 25 mm CR. (1967) Ass Anat 51: 819-827.
- ↑ Pillet J. Reconstruction du pelvis d’un embryon humain de 7.5 mm (Stade XVI de Streeter) CR. (1968) Ass Anat 52: 1013-1023.
- ↑ Pillet J (1969) Reconstruction des organes génito«-urinaires et des veines pelviennes d’un embryon de 12,5 mm (Stade XVII de Streeter) CR. Ass Anat 53 : 1817-1824.
- ↑ Pillet J. Reconstruction des organes pelviens d’un embryon de 5 mm (Stade XV de Streeter) CR. (1971) Ass Anat 54:705-715
- ↑ 6.0 6.1 DeSilva JM & Rosenberg KR. (2017). Anatomy, Development, and Function of the Human Pelvis. Anat Rec (Hoboken) , 300, 628-632. PMID: 28297176 DOI.
- ↑ Gajewska E, Sobieska M & Moczko J. (2018). Position of pelvis in the 3rd month of life predicts further motor development. Hum Mov Sci , 59, 37-45. PMID: 29602050 DOI.
- ↑ 8.0 8.1 8.2 Okumura M, Ishikawa A, Aoyama T, Yamada S, Uwabe C, Imai H, Matsuda T, Yoneyama A, Takeda T & Takakuwa T. (2017). Cartilage formation in the pelvic skeleton during the embryonic and early-fetal period. PLoS ONE , 12, e0173852. PMID: 28384153 DOI.
- ↑ Verbruggen SW & Nowlan NC. (2017). Ontogeny of the Human Pelvis. Anat Rec (Hoboken) , 300, 643-652. PMID: 28297183 DOI.
- ↑ Giordani J, Bajard L, Demignon J, Daubas P, Buckingham M & Maire P. (2007). Six proteins regulate the activation of Myf5 expression in embryonic mouse limbs. Proc. Natl. Acad. Sci. U.S.A. , 104, 11310-5. PMID: 17592144 DOI.
- ↑ 11.0 11.1 Geetha-Loganathan P, Nimmagadda S, Christ B, Huang R & Scaal M. (2010). Ectodermal Wnt6 is an early negative regulator of limb chondrogenesis in the chicken embryo. BMC Dev. Biol. , 10, 32. PMID: 20334703 DOI.
- ↑ Yu SR, Burkhardt M, Nowak M, Ries J, Petrásek Z, Scholpp S, Schwille P & Brand M. (2009). Fgf8 morphogen gradient forms by a source-sink mechanism with freely diffusing molecules. Nature , 461, 533-6. PMID: 19741606 DOI.
- ↑ 13.0 13.1 Windhagen H, Thorey F, Kronewid H, Pressel T, Herold D & Stukenborg-Colsman C. (2005). The effect of functional splinting on mild dysplastic hips after walking onset. BMC Pediatr , 5, 17. PMID: 15958160 DOI.
- ↑ US Preventive Services Task Force. (2006). Screening for developmental dysplasia of the hip: recommendation statement. Pediatrics , 117, 898-902. PMID: 16510673 DOI.
Reviews
Anatomical Record - Special Issue:The Human Pelvis: Anatomy, Development and Function. April 2017 DeSilva JM & Rosenberg KR. (2017). Anatomy, Development, and Function of the Human Pelvis. Anat Rec (Hoboken) , 300, 628-632. PMID: 28297176 DOI.
Hill RE. (2007). How to make a zone of polarizing activity: insights into limb development via the abnormality preaxial polydactyly. Dev. Growth Differ. , 49, 439-48. PMID: 17661738 DOI.
Articles
Satoh A, Makanae A & Wada N. (2010). The apical ectodermal ridge (AER) can be re-induced by wounding, wnt-2b, and fgf-10 in the chicken limb bud. Dev. Biol. , 342, 157-68. PMID: 20347761 DOI.
Galli A, Robay D, Osterwalder M, Bao X, Bénazet JD, Tariq M, Paro R, Mackem S & Zeller R. (2010). Distinct roles of Hand2 in initiating polarity and posterior Shh expression during the onset of mouse limb bud development. PLoS Genet. , 6, e1000901. PMID: 20386744 DOI.
Stefanov EK, Ferrage JM, Parchim NF, Lee CE, Reginelli AD, Taché M & Anderson RA. (2009). Modification of the zone of polarizing activity signal by trypsin. Dev. Growth Differ. , 51, 123-33. PMID: 19207183 DOI.
Search PubMed
Search Pubmed: Pelvis Development |
Additional Images
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 16) Embryology Musculoskeletal System - Pelvis Development. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Musculoskeletal_System_-_Pelvis_Development
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G