Musculoskeletal System - Abnormalities
| Embryology - 23 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
There are a large number of different musculoskeletal abnormalities affecting one or a combination of bone and muscle development in the skull, trunk and limbs. This page therefore can only broadly introduce the topic and link to other resources with more specific information.
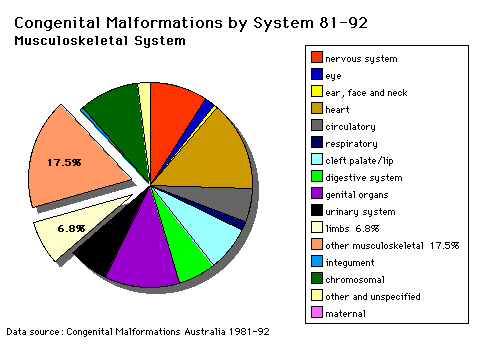
Musculoskeletal and limb disorders together form the largest group of congenital defects that occur in Australia. The three most commonly occurring are developmental dysplasia of the hip, cleft palate, cleft lip and palate.
Some defects appear as obvious malformations, such as syndactyly and limb reductions. Other muscular defects only become obvious postnatally when the muscles are required to be used, those in highest use are respiratory (diaphragm, intercostals) and anti-gravity (those that hold you upright) muscles.
International Classification Diseases - Musculoskeletal
| System Abnormalities | ||||
|---|---|---|---|---|
|
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Congenital Musculoskeletal Abnormalities | Hip Displasia | Scoliosis | Duchenne Muscular Dystrophy | Muscular Dystrophy | Calcaneovalgus |
| Older papers |
|---|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
|
Australian Statistics
The ten most frequently reported birth defects in Victoria between 2003-2004.
- Hypospadias
- Obstructive Defects of the Renal Pelvis or Obstructive Genitourinary Defects
- Ventricular Septal Defect
- Congenital Dislocated Hip
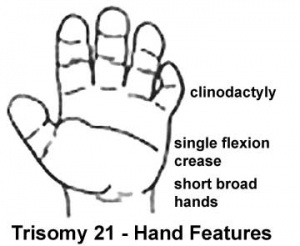
- Trisomy 21 or Down syndrome
- Hydrocephalus
- Cleft Palate
- Trisomy 18 or Edward Syndrome - multiple abnormalities of the heart, diaphragm, lungs, kidneys, ureters and palate 86% discontinued.
- Renal Agenesis/Dysgenesis - reduction in neonatal death and stillbirth since 1993 may be due to the more severe cases being identified in utero and being represented amongst the increased proportion of terminations (approximately 31%).
- Cleft Lip and Palate - occur with another defect in 33.7% of cases.
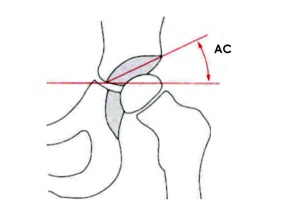
Developmental Dysplasia of the Hip
ICD-11 LB74.0 Developmental dysplasia of hip
|
Also called Congenital Hip Dislocation.
- Instability: 1:60 at birth; 1:240 at 1 wk: Dislocation untreated; 1:700
- congenital instability of hip, later dislocates by muscle pulls or gravity
- familial predisposition female predominance
- Growth of femoral head, acetabulum and innominate bone are delayed until the femoral head fits firmly into the acetabulum.
Barlow test
(Barlow maneuver) A clinical term to describe a physical examination of the newborn for Developmental dysplasia of the hip (DDH). The examiner adducts the hip (bringing the thigh towards the midline) while applying light pressure on the knee, directing the force posteriorly. A positive sign is the hip being dislocatable, if the hip can be popped out of socket with this test. This test is then combined with the Ortolani test (maneuver). The test is named after Thomas Barlow (1845 – 1945) a British royal physician.
Ortolani test
(Ortolani manoeuvre) A clinical term to describe a physical examination of the newborn for developmental dysplasia of the hip (DDH). This is a test for posterior dislocation of the hip. Using the examiner's thumb, abduct the infant's leg, while using the examiner's index finger to place anterior pressure on the greater trochanter. A positive sign is a distinctive 'clunk' which can be heard and felt as the femoral head relocates anteriorly into the acetabulum, usually becomes negative after 2 months of age. This test is combined with the Barlow test (manoeuvre). Named after Marino Ortolani, the test developer in 1976.
Abduction Splints
There is variable evidence for the use of abduction splinting during onset of walking in children on the maturation of mild dysplastic hips.[4]
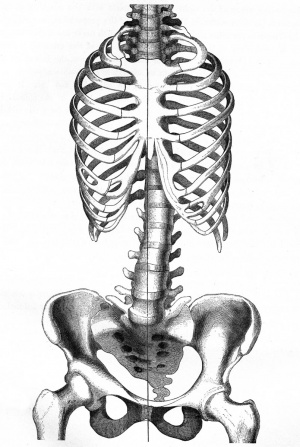
Scoliosis

ICD-11 FA70 Spinal deformities - FA70.1 Scoliosis
ICD-11 See also - LB73.25 Congenital scoliosis due to congenital bony malformation | FC01.5 Postradiation scoliosis FC01 Postprocedural disorders of the musculoskeletal system |

|
|
Chêneau's Brace

Dr. Chêneau fabricated the original "Chêneau Brace" in 1979 and is commonly used for the treatment of scoliosis and thoracic hypokyphosis in some European countries, though not commonly in either North America or the United Kingdom. The brace corrects by a system of multipoint pressure zones and expansion chambers.
Harrington Rod
Dr Paul Harrington, a USA orthopaedic surgeon, in 1953 designed the "Harrington implant", the first modern spinal instrumentation system that produced both correction and immobilization. This historic system has now been replaced by more modern systems.
- Links: axial skeleton
Scoliosis Research Society Questionnaires
The Scoliosis Research Society has a number of Patient Outcome Questionnaires available. The questionnaires relating to lumbar surgery are the SRS22R preoperative and the SRS30 one-year postoperative.[7][8]
For idiopathic scoliosis, the generic quality of life measurement quantified by SRS22R has been shown to be overall similar between males and females in treatment and age groups, but reduced in comparison with the general population.[9]
Muscular Dystrophy
| ICD-11 |
|---|
|
8C70 Muscular dystrophy 8C70.0 Becker muscular dystrophy 8C70.1 Duchenne muscular dystrophy 8C70.2 Emery-Dreifuss muscular dystrophy 8C70.3 Facioscapulohumeral muscular dystrophy 8C70.4 Limb-girdle muscular dystrophy 8C70.5 Scapuloperoneal muscular dystrophy 8C70.6 Congenital muscular dystrophy |
There can be abnormalities associated directly with muscle differentiation and function as well as those mediated indirectly by abnormalities of innervation or skeletal development and other associated systems.
Duchenne Muscular Dystrophy
The most common occuring in Boys and in Duchenne Muscular Dystrophy (DMD). This cause of the disease was discovered in 1988 as a mutation in dystrophin, a protein that lies under the muscle fiber membrane and maintains the cell's integrity. As skeletal muscles have little prenatal load or use it is not until postnatally that muscle wasting occurs, usually in the anti-gravity muscles first. This is a progressive disease usually detected between 3-5 years old.
- X-linked dystrophy
- large gene encoding cytoskeletal protein - Dystrophin
- progressive wasting of muscle, die late teens
Becker Muscular Dystrophy
A milder adult (30-40 years old) onset form of the disease Becker's Muscular Dystrophy (BMD) that involves mutations in the same dystrophin gene.
Autosomal Recessive Muscular Dystrophy
Dystroglycan, a protein that associates with both dystrophin and membrane molecules, is a candidate gene for the site of the mutation in autosomal recessive muscular dystrophies. A knockout mouse has been generated that has early developmental abnormalities.
Myotonic Dystrophy
|
ICD-11 8C71.0 Myotonic dystrophy
|
Myotonic dystrophy (DM) is the most common inherited, autosomal dominant neuromuscular disorder in adults, affecting 1 out of 8000 people. The disease causes myotonia and muscle weakness in skeletal muscles with a risk of life-threatening cardiorespiratory disorders. The disease is "amplified" through generations probably by a similar GC expansion associated with Huntington disease.
Two genetic types:
- DM1 - expansion of cytosine thymidine guanine (CTG) repeats in non-coding regions (3′-untranslated region) of the myotonic dystrophy protein kinase (DMPK) gene.
- DM2 - expansion of CCTG repeats in zinc finger protein 9 (ZnF9) gene.
Facioscapulohumeral Muscular Dystrophy
(FSHD) This form of muscular dystrophy is an autosomal dominant genetic disorder characterized by progressive muscle weakness and wasting that typically begins in the face, shoulder-girdle and upper arm. Currently thought to relate to an impaired muscle regeneration process.
- Links: skeletal muscle
Spinal Muscular Atrophy
| ICD-11 8B61 Spinal muscular atrophy (ICD-10-CM Diagnosis Code G12.9) |
Spinal muscular atrophy (SMA) is a rare neural genetic condition that leads to a loss of motor neurons and then progressive muscle wasting. The disease exists in several different forms: Type 1, Type 2, and Type 3a SMA. A new drug treatment using nusinersen (trade name Spinraza®) has led to the inclusion of SMA in the newborn heel-prick test (Guthrie test).
- Links: spinal cord
Congenital Myasthenic Syndromes
| ICD-11 |
|---|
|
Myasthenia gravis or certain specified neuromuscular junction disorders
|
A heterogeneous group of neuromuscular disorders (32 gene mutations, autosomal dominant or autosomal recessive) that have an impairment of neuromuscular transmission.[10] The most common causative genes are CHAT, COLQ, RAPSN, CHRNE, DOK7, and GFPT1.
- 8 presynaptic proteins
- 4 synaptic proteins
- 15 post-synaptic proteins
- 5 glycosilation proteins
Limb Abnormalities
Genetic
- Human Gene Mutations - mutation of any of the patterning genes will result in limb abnormalities (Will put Table on Web page mutations and terminology)
Type II syndactyly- HoxD13
Maternal
- thalidomide Phocomelia
- short ill-formed upper or lower limbs
- hyperthermia
- Links: limb abnormalities | thalidomide
Syndactyly
Fusion of fingers or toes which may be single or multiple and may affect: skin only, skin and soft tissues or skin, soft tissues and bone.
The condition is unimportant in toes but disabling in fingers and requires operative separation and is frequently inherited as an autosomal dominant.
The presence of this additional "webbing" reflects preservation of the developmental tissues that in normal development are removed by programmed cell death (apotosis).
Polydactyly
Presence of additional toes or fingers also called polydactylia or polydactylism. The condition is often treated surgically in the infant.
Ernest Hemingway in the 1930's had a six-toed cat (Snowball) showing a form of polydactyly and cats with a similar condition are now called "Hemingway cats".
(More? Limb Development Abnormalities - Polydactyly)
Polysyndactyly
| ICD-11 LB78 Polydactyly - LB78.0 Polydactyly of the thumb | LB78.1 Polysyndactyly | LB78.2 Postaxial polydactyly of fingers | LB78.3 Polydactyly of toes |
Developmental abnormality where there is a combination of polydactyly with syndactyly is known as polysyndactyly.
Triphalangeal Thumb (TPT)
| ICD-11 Structural developmental anomalies of the skeleton - LB76 Triphalangeal thumb | LD26.2 Syndromes with limb duplication, polydactyly, syndactyly or triphalangism |
|
Developmental abnormality with three phalanges instead of two, forming a long, finger-like thumb. Usually inherited as an autosomal dominant trait, gene locus chromosome region 7q36. |
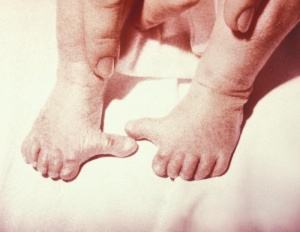
Calcaneovalgus
| ICD-11 LB98.2 Congenital valgus deformities of feet - LB98.22 Talipes calcaneovalgus |
- Occurs in about 5% of all newborns.
- Females are affected more often than males.
- Deformity can be unilateral or bilateral.
- external rotation of the calcaneus.
- an overstretched Achilles tendon.
- tight anterior leg musculature.
See the review "The Newborn Foot" (2004).[11]
Gastroschisis
| ICD-11 Structural developmental anomalies of the diaphragm, abdominal wall or umbilical cord - LB02 Gastroschisis |
By definition, it is a body wall musculoskeletal defect, not a gastrointestinal tract defect, which in turn impacts upon GIT development.
| Gastroschisis (paraomphalocele, laparoschisis, abdominoschisis, abdominal hernia) is an abdominal wall defect associated with evisceration of the intestine (2.5 cases/10,000 births), occuring more frequently in young mothers (less than 20 years old). There have been reports that this abnormality is increasing in incidence.
The abnormality is usually situated to the right of the umbilicus and abdominal contents, mainly gastrointestinal, are found outside the anterior body wall. |

|
| Can occur in isolation and also in association with other gastrointestinal anomalies (intestinal atresia, perforation, necrosis or volvulus). Defects in other organ systems have been reported in up to 35% of children. There are several theories as to the cause of this abdominal wall defect, including recently failure of the yolk sac and related vitelline structures to be incorporated into the umbilical stalk.[12]
The condition can often be detected by ultrasound scan. Reported as a high mortality defect, only 60% of children survive until the end of the first year of age. |
|
Gastroschisis patients are commonly small for gestational age (SGA, birth weight < 10th centile). Frequency line graphs of the birth weight distribution, Kolmogorov-Smirnov test confirmed that this difference was significant (p < 0.001).[13]
|
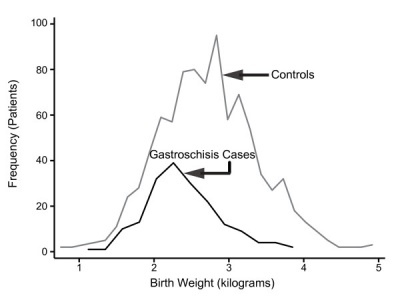
|
Gastroschisis Classification
There has been a recent attempt to classify gastroschisis in order to measure clinical outcomes.[14]
- Simple gastroschisis - intact continuous bowel that is not compromised or breached at delivery or presentation
- Complex gastroschisis - presence of one or more of intestinal atresia, perforation or intestinal necrosis at delivery or presentation, or missed atresia
- Links: gastroschisis | Ultrasound movie - Gastroschisis | UCSF Childrens Hospital - Gastroschisis | Brown University Image Bank- Abdominal Wall Defects
Inguinal Hernia
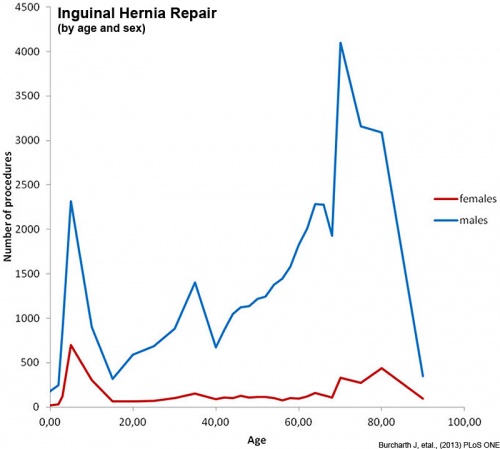
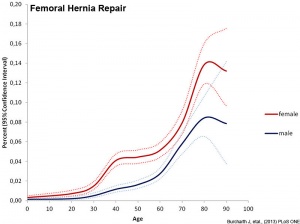
Inguinal hernias are more common in males and associated with the fetal/neonatal developmental descent of the testis through the abdominal wall. The following graphs are from a study of Danish data on postnatal hernia repairs[15]. In contrast, femoral hernia repairs occur mainly in adults in both sexes and increases with age.

|
|
| Inguinal hernia repair | Femoral hernia repair |
- Links: genital abnormalities
References
- ↑ Osborn DPS. etal; Mutations in INPP5K cause a form of congenital muscular dystrophy overlapping Marinesco-Sjögren syndrome and dystroglycanopathy. (2017) The American Journal of Human Genetics http://www.cell.com/ajhg/fulltext/S0002-9297(17)30019-8 Published online: February 9, 2017
- ↑ Chotigavanichaya C, Leurmsumran P, Eamsobhana P, Sanpakit S & Kaewpornsawan K. (2012). The incidence of common orthopaedic problems in newborn at Siriraj Hospital. J Med Assoc Thai , 95 Suppl 9, S54-61. PMID: 23326983
- ↑ Pannier S, Mugniery E, Jonquoy A, Benoist-Lasselin C, Odent T, Jais JP, Munnich A & Legeai-Mallet L. (2010). Delayed bone age due to a dual effect of FGFR3 mutation in Achondroplasia. Bone , 47, 905-15. PMID: 20673820 DOI.
- ↑ 4.0 4.1 Windhagen H, Thorey F, Kronewid H, Pressel T, Herold D & Stukenborg-Colsman C. (2005). The effect of functional splinting on mild dysplastic hips after walking onset. BMC Pediatr , 5, 17. PMID: 15958160 DOI.
- ↑ Postema SG, van der Sluis CK, Waldenlöv K & Norling Hermansson LM. (2012). Body structures and physical complaints in upper limb reduction deficiency: a 24-year follow-up study. PLoS ONE , 7, e49727. PMID: 23226218 DOI.
- ↑ Zaborowska-Sapeta K, Kowalski IM, Kotwicki T, Protasiewicz-Fałdowska H & Kiebzak W. (2011). Effectiveness of Chêneau brace treatment for idiopathic scoliosis: prospective study in 79 patients followed to skeletal maturity. Scoliosis , 6, 2. PMID: 21266084 DOI.
- ↑ Crawford CH, Glassman SD, Bridwell KH, Berven SH & Carreon LY. (2015). The minimum clinically important difference in SRS-22R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine , 40, 377-81. PMID: 25774463 DOI.
- ↑ Carreon LY, Kelly MP, Crawford CH, Baldus CR, Glassman SD, Shaffrey CI & Bridwell KH. (2018). SRS-22R Minimum Clinically Important Difference and Substantial Clinical Benefit After Adult Lumbar Scoliosis Surgery. Spine Deform , 6, 79-83. PMID: 29287822 DOI.
- ↑ Diarbakerli E, Grauers A, Danielsson A, Abbott A & Gerdhem P. (2019). Quality of Life in Males and Females With Idiopathic Scoliosis. Spine , 44, 404-410. PMID: 30180148 DOI.
- ↑ Finsterer J. (2019). Congenital myasthenic syndromes. Orphanet J Rare Dis , 14, 57. PMID: 30808424 DOI.
- ↑ Gore AI & Spencer JP. (2004). The newborn foot. Am Fam Physician , 69, 865-72. PMID: 14989573
- ↑ Stevenson RE, Rogers RC, Chandler JC, Gauderer MW & Hunter AG. (2009). Escape of the yolk sac: a hypothesis to explain the embryogenesis of gastroschisis. Clin. Genet. , 75, 326-33. PMID: 19419415 DOI.
- ↑ Payne NR, Simonton SC, Olsen S, Arnesen MA & Pfleghaar KM. (2011). Growth restriction in gastroschisis: quantification of its severity and exploration of a placental cause. BMC Pediatr , 11, 90. PMID: 22004141 DOI.
- ↑ Molik KA, Gingalewski CA, West KW, Rescorla FJ, Scherer LR, Engum SA & Grosfeld JL. (2001). Gastroschisis: a plea for risk categorization. J. Pediatr. Surg. , 36, 51-5. PMID: 11150437 DOI.
- ↑ Burcharth J, Pedersen M, Bisgaard T, Pedersen C & Rosenberg J. (2013). Nationwide prevalence of groin hernia repair. PLoS ONE , 8, e54367. PMID: 23342139 DOI.
Journals
- Scoliosis - the official journal of the Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) and affiliated with the International Research Society of Spinal Deformities (IRSSD), is ready to receive manuscripts on all aspects of the prevention, control, and treatment of scoliosis and other spinal deformities.
- BMC Musculoskeletal Disorders is an open access journal publishing original peer-reviewed research articles in all aspects of the prevention, diagnosis and management of musculoskeletal and associated disorders, as well as related molecular genetics, pathophysiology, and epidemiology.
Reviews
Perronnet C & Vaillend C. (2010). Dystrophins, utrophins, and associated scaffolding complexes: role in mammalian brain and implications for therapeutic strategies. J. Biomed. Biotechnol. , 2010, 849426. PMID: 20625423 DOI.
Le Rumeur E, Winder SJ & Hubert JF. (2010). Dystrophin: more than just the sum of its parts. Biochim. Biophys. Acta , 1804, 1713-22. PMID: 20472103 DOI.
Lapidos KA, Kakkar R & McNally EM. (2004). The dystrophin glycoprotein complex: signaling strength and integrity for the sarcolemma. Circ. Res. , 94, 1023-31. PMID: 15117830 DOI.
Gore AI & Spencer JP. (2004). The newborn foot. Am Fam Physician , 69, 865-72. PMID: 14989573
Articles
Singh SM, Kongari N, Cabello-Villegas J & Mallela KM. (2010). Missense mutations in dystrophin that trigger muscular dystrophy decrease protein stability and lead to cross-beta aggregates. Proc. Natl. Acad. Sci. U.S.A. , 107, 15069-74. PMID: 20696926 DOI.
Norwood FL, Sutherland-Smith AJ, Keep NH & Kendrick-Jones J. (2000). The structure of the N-terminal actin-binding domain of human dystrophin and how mutations in this domain may cause Duchenne or Becker muscular dystrophy. Structure , 8, 481-91. PMID: 10801490
Search PubMed
Search April 2010
- Musculoskeletal System Development - All (44637) Review (5065) Free Full Text (6601)
- Musculoskeletal Development - All (44637) Review (5065) Free Full Text (6601)
Search Pubmed: musculoskeletal system abnormalities
Additional Images
Terms
- centrum - (vertebral body) anatomical term referring to the main bony part of the vertebra that forms the majority of the axial skeleton.
- Cobb angle - clinical method of measuring the degree of scoliosis and post-traumatic kyphosis. Named after the American orthopedic surgeon John Robert Cobb (1903 - 1967) an American orthopedic surgeon.
- haemal arch - referring to the bony arch region within animal tail vertebra that contains blood vessels.
- idiopathic scoliosis - clinical term for a spinal column deformity appearing usually postnatally after the age of 10 years old.
- lordosis - clinical and anatomy term describing the curvature of the spine with the convexity toward the front. Normal to have lordosis in the cervical and lumbar regions of the spinal column.
- neural arch - referring to the bony arch region within vertebra that contains the spinal cord.
- notochord sheath - region surrounding the notochord. in teleost fish direct mineralization of this region, by intramembranous ossification, forms the initial vertebral centrum. (More? zebrafish)
- rib hump - clinical term for the prominence formed by ribs on the convexity of a curve, caused by rotation of the spine and attached ribs.
- spinal column - term referring to the musculoskeletal elements (vertebrae, ligaments, and intervertebral discs), that surround the spinal cord and form the axial skeleton.
- Spondylometaphyseal dysplasia - (SMD) rare form of bone dysplasia comprising various types of chondrodystrophy characterized by metaphyseal irregularities of the long bones, together with generalized platyspondyly of varying severity in the spine. First described in 1967 by Kozlowski. {More? image)
- synsacrum - in birds sacral and lumbar vertebrae fused region forming elongated sacral region.
- thoracic hypokyphosis - term referring to the backward curve in the upper spine is to great, round back, Scheuermann's disease, or simply kyphosis.
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- Scoliosis - the official journal of the Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) and affiliated with the International Research Society of Spinal Deformities (IRSSD).
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 23) Embryology Musculoskeletal System - Abnormalities. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Musculoskeletal_System_-_Abnormalities
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G