Book - A Very Young Ovum In Situ
| Embryology - 24 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Leopold G. A Very Young Ovum In Situ (1907) translated by Vogt WH. CV Mosby and Co. St Louis.
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
A Very Young Ovum In Situ
Prof. Leopold
Geheimer Medizinalrat, Director Of The Royal Gynecologic
Clinic And School For Midwifery. Member Of The
Royal Medical Board Of Dresden.
Comprising The Fourth Volume Of The "Arbeiten Aus Der Frauen Klinik In Dresden."
With Sixteen Lithographic Plates
Authorized English Translation
By
W. H. Vogt, M. D.
Gynecologist And Obstetrician To The Lutheran Hospital St. Louis, Missouri
C. V. Mosby Co.
St. Louis 1907
Introduction
The Ovum which forms the subject of this investigation originates from a young woman who committed suicide with phosphorus. The post mortem examination was performed by -Obermedizinalrat Prof. Dr. Schmorl, in the pathological institute of the Friedrichsstaedter hospital in Dresden.
The fact that this woman had committed suicide suggested the possibility of a pregnancy and for that reason the anterior wall of the uterus was split and the specimen carefully hardened, first in formalin and then in increasing strengths of alcohol. Although repeated and careful examinations of the endometrium were made with a magnifying glass, no ovum could be detected. Still the greatly swollen mucous membrane which was divided into irregular areas by furrows, as we are accustomed to see in a pregnant uterus, was conspicuous and induced us to make repeated examinations during the process of hardening. Finally a small spot was detected, lighter than the surrounding tissue, situated on the posterior wall of the corpus uteri a little below its center and immediately above a deep furrow. In order to study this small spot more carefully, a square piece of mucous membrane about 1 cm. long, with its underlying muscularis was excised and after further hardening by the laboratory assistant, Mr. Ernst Thomas, cut into a continuous series of sections, five microns thick and then stained in haematoxylineosin. The middle one hundred and sixty sections comprised a very small ovum whose measurements were 1.4 mm. long 0.9 mm. deep and 0.8 mm. wide, an ovum about the size of that described by Peters, however a trifle smaller, its length being 0.2 mm. shorter than that of Peters, which measured 1.6 mm. in length, 0.8 mm. in depth and 0.9 mm. in breadth. No information
could be obtained concerning the time of the last or first missing menstruation. Hence it seems useless to attempt any estimate of the age of this ovum. In the following pages it is intended to compare the results of the microscopic examinations with those of Peters, since this one and the one described by him are the two smallest and youngest human ova ever observed.
The accompanying plates were carefully drawn by the artist, Richard Scholz, exactly true to nature and without any attempt to obtain a diagramatic effect.
I wish to thank the artist, as well as the publisher, for the excellent reproduction of these figures and for the valuable services they have thereby rendered science.
There will be considered:
- The Decidua Vera.
- The Implantation of the Ovum with the formation of the capsularis and the fibrinous covering, which lies over the ovum on the mucous membrane. ("Gewebspilz" of Peters.)
- The "Eianlage" and the Ovular Chamber "Eikammer."
- The Trophoblast and its surrounding blood spaces.
- The Syncytium.
A germinal plate which was found in Peters' specimen could not be discovered in any of the sections of this new ovum. Whether its absence be possibly due to the general phosphorus poisoning must remain an open question until more specimens of such an early stage are obtained. It must be remembered that the woman from whom the Peters ovum was obtained, also committed suicide, but with caustic potash, which is capable of producing a very acute hyperemia of the mucous membrane of the pelvic organs.
Some of the ova described by Marchand, Rossi Doria, Graf von Spec, Heukelom, Mertens, etc., can hardly be pronounced normal specimens free of objections. The indications for the post mortem in such instances will necessarily be either a suicide or an acute illness caused by poisoning or some intercurrent disease (such as pneumonia, burns, etc.), or a disease of the sexual organs necessitating a removal of the uterus. All of these conditions, especially in the early stages of pregnancy, will hardly ever fail to lead to some changes in the circulatory apparatus of the uterus. Nevertheless some portions of both the uterus or the ovum may be found in a very satisfactory state of preservation.
Of the three young ova described by Marchand, the first had a defective fibrinous capsule, supposedly injured during a curetage. The second was infiltrated with blood and yet Marchand did not hesitate to investigate these defective specimens, to study such difficult problems as the trophoblast and the syncytium and finally drew, although with great precaution, certain conclusions.
In order to satisfy myself of the value of this specimen I submitted several sections to my esteemed colleagues, Obermedizinalrat Prof. Dr. Schmorl and Prof. Graf von Spec in Kiel, whom I wish to thank for a careful examination of these slides. Prof. Graf von Spec did not question in the least the good histological preservation of this specimen. He called attention to the great scientific value of this new ovum and pointed out the frequent occurrence of a congested area surrounding the seat of implantation in this stage of development. The ovum of Peters, which may be one-half to one day older, also shows this marked congestion of the blood vessels in the immediate neighborhood of the ovum.
We must bear in mind that during or immediately after the penetration of the ovum into the endometrium, a pronounced afflux of blood is a natural consequence. Regarding this only a study of other very young ova, which can be expected in the near future, will throw more light on this problem, until then it seems permissible to disregard the objection that the poisoning with phosphorus might interfere with the reliability of the histological picture presented by our specimen. At any rate it must be emphasized, that this latest ovule, exactly like that of Peters', the one demonstrated by Graf, von Spec in Kiel, and the very small ovum described by me in my atlas ("Uterus und Kind") were found in' situ embedded in an uninjured mucous membrane in a perfect condition.
The detailed discussion in the following chapter will be simplified by a general preliminary consideration of the mucous membrane elevation which harbors the ovum. This is done in the following table, which contains only the findings pertaining to this point in the sections 1 to 160.
This table shows plainly that the fibrin coat ("Gewebspilz" of Peters) which covers the top of the mucous membrane elevation ("Schleimhauthuegel") consists of two adjoining portions. The one we can follow from sections 10 to 68, where it has almost disappeared. The second portion begins in section 75 and disappears again completely in section 103. In a similar manner the glands and the blood vessels can be followed. This preliminary general consideration furnishes a good picture of the enormous number of glands and capillaries and shows how the glands gradually are crowded out through the dilatation and rupture of the capillaries in the surrounding tissue.
This general survey alone demonstrates the fact that the minute ovum is completely encircled by free blood spaces.
It affords me great pleasure to say a few words regarding the translation of my book, which Dr. Vogt has so kindly undertaken. A few years ago Dr. Vogt was a pupil of mine who for many months assisted me both in theoretical and practical work. I shall owe to this translation a widespread acquaintance with this highly interesting specimen, herein described, among my many friends and former pupils, as well as my colleagues on the other side of the ocean.
It is hoped that this book will instigate further research concerning the earliest stages of human existence.
Prof. Dr. Leopold.
Dresden, Koenigliche Frauenklinik, January, '07.
Translator's Preface
The deplorable fact that numerous important contributions to medical literature," appearing in the German language, remain unread by the English-speaking fraternity as the result of an imperfect acquaintance with that tongue, induced me to undertake the translation of this valuable study of one of the youngest human ova found in situ. When requested to do this work by my esteemed former chief, Prof. Dr. Leopold, I was impressed with the necessity of preventing the English-speaking profession from remaining unacquainted with a work of such high order.
This book should prove interesting and instructive not only to the embryologist and the obstetrician, but also to the profession in general, and if by its translation I shall have succeeded in disseminating a clearer knowledge of this complex subject, I shall feel amply repaid for my labor.
In conclusion I wish to thank my friend and colleague, Dr. Hugo Ehrenfest, for the very kind and valuable assistance which he rendered me in the translation of the book, and I also wish to express my indebtedness to Mr. Geo. Heithaus, stud. med. for his aid in the reading of the proofs.
W. H. Vogt, M. D.
St. Louis, Mo., September, 1907. 4977 Lotus Ave.
Consideration of the Reconstruction of the Ovum from Sections 1-160
I. The Mucous Membrane Elevation which Harbors the Ovum, and the Decidua Vera
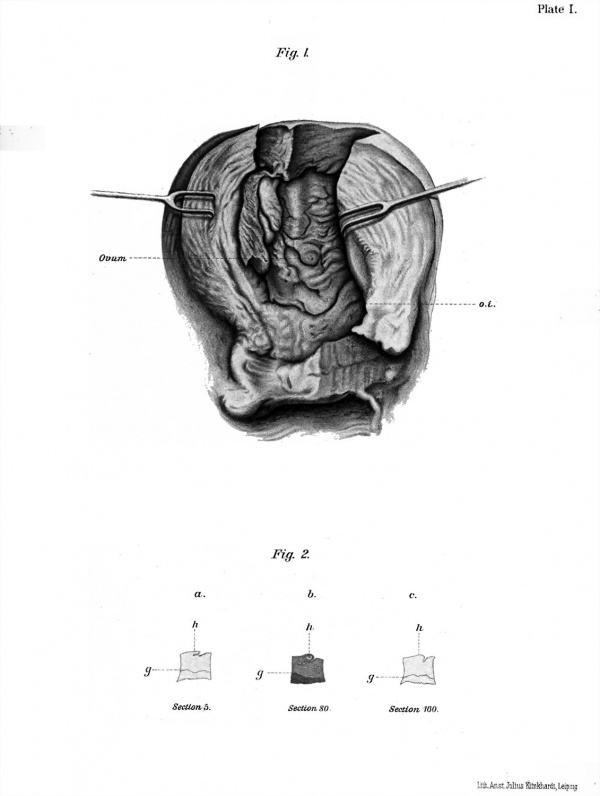
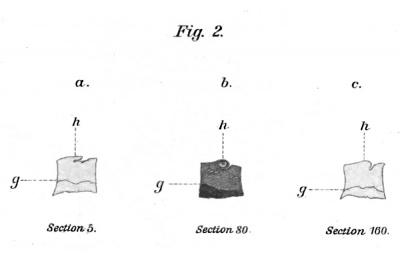
The mucosa, which lines the corpus uteri, is about 5 mm. thick in the fundus and anterior wall but about 8 mm. thick in the middle of the posterior wall. As previously mentioned, numerous deep and irregular furrows divide the mucous membrane into a number of fields. Toward the internal os (Plate I Fig. 1. o. i.) the mucosa suddenly becomes thinner and assumes the characteristic appearance of the plicae palmatae. It is here only 2 to 4 mm. thick. Since, as is well known, the mucous membrane of the uterus has no submucosa, a sharp line divides it from the underlying muscularis (Fig. 2, g.). Any thin section passing through both mucosa and muscularis, if held to the light, will distinctly show this sharp division both in the pregnant and the non-pregnant uterus. Nevertheless the connection between the mucosa and the underlying muscularis is a very firm one. The blind ends of the uterine glands are fastened by means of a very fine meshed connective tissue near the funnel shaped cavities and holes formed by the muscular fibres which are visible immediately below the mucosa, both in transverse and oblique sections.
In Fig. 1 the somewhat lighter spot, marked "Ovum," indicates the seat of implantation of the small ovum. It lies in a slightly protruding elevation of the mucosa ("Schleimhauthuegel") nearer its slope, which gradually loses itself in a broad and rather deep furrow, (vide Fig. 2, a 2. c. Fig. 23, sections 94 to 96.)
In about the first ten sections this little hill appears as a horizontal fold of the mucosa with a sharp edge (Fig. 2. a. h.) which, as can be seen under the microscope, begins with a blunt extremity and has a gland passing through its entire length. This gland in its middle portion is dilated and folded and lined in its entirety with perfectly preserved cuboidal epithelium.
Gradually this hill like elevation becomes more rounded (Fig. 2. b. h.) with a sharp groove on its right side. This shape is maintained through almost all of the sections until section 160 is reached, where it takes on a more club shaped appearance. The furrow to its right has become somewhat shallower and now runs perpendicular.
We might be led to believe that this elevation was brought about by the embedding of the ovum, but the further examination of the specimen will show that the mound is only the marginal elevation of a mucous membrane field, lying just above a groove, through which the ovum has bored its way.
This ovum, like the ovule of Peters, in all probability has entirely sunk into the mucous membrane, so that we also find in this case the ovular chamber completely surrounded by a decidua vera which extends up into the cap which covers the top of the ovum and protrudes into the uterine cavity. Besides this decidual tissue the cap contains the fibrinous cover consisting of two layers or two flat portions, while in Peters' case the closure of the small opening on the top is formed by the fibrin lid alone, in this case the nidus of the ovum represents a completely closed cavity which on its top carries the fibrinous cover. In investigating the histologic structure of this mucous membrane elevation our attention is at once drawn to the decidual tissue, the glands and the blood vessels, the ovular chamber and its fibrin cover. Since the two last named structures will be considered in the next chapter, the enveloping tissue alone shall here be described.
It is probably unnecessary to state that the younger the ovum, the better will be the opportunity of studying the origin of certain structures such as the decidual cells, the syncytium, the intervillous spaces, etc.
If any doubt has still existed concerning the fact that the decidual cells are nothing else but hypertrophied connective tissue cells of the uterine muscosa and have nothing to do with the leucocytes, this doubt is now dispelled by this specimen.
The mucous membrane enveloping the ovum is swollen and appears edematous. Large connective tissue cells with long processes form a delicate network. These cells contain large nuclei which in some cases completely fill the cell body. Some cells have two nuclei, and like Peters (1. c. page 15.), I was able to observe signs of karyokinesis in them.
In the vicinity of the capillaries and larger blood vessels, which are enormously dilated and in some places ruptured, we find many red blood corpuscles lying between the decidual cells.
In this way the somewhat exaggerated histologic picture of hyperemia and actual suffusion of the mucous membrane (compare Fig. 25. Section 142) is formed, not unlike that described as occurring during menstruation, by the author 1 , later by.Gebhard 2 , and recently by Sellheim. 3
Between the blood vessels and glands the decidual tissue is distributed partly in fine and coarse bands, partly in form of an outstretched network and there is as yet no distinction possible between a decidua compacta and decidua spongiosa, since we find thick compact layers and broad bands of decidual tissue in the superficial as well as the deeper layers of the mucosa.
Noteworthy is the wealth of glands and their course. In the sections on either side of the ovum (Sections 1 to 30 and 120 to 160) some of the glands can be followed in their entire length up to their entrance into the uterine cavity (Fig. 3, Section 4. Fig 25, Section 142). At the opening and in the middle they are often greatly dilated. Here their walls are folded, forming larger and smaller waves which like papillae protrude into glandular lumen and suggest the picture of a beginning adenoma In the deeper portions the glands are lined with a perfectly preserved cylindrical epithelium which however becomes more distinctly cuboidal the closer the glands approach the base of the peripheral wall of the ovular chamber.
Since the latter is made up of blood spaces, as will be demonstrated later, the surrounding decidual tissue also is 'infiltrated with blood, as can be seen in Fig. 25, Section 142 (Plate XV bl.).
As a result of this mucosa hemorrhage the glands in the immediate vicinity of the ovum also are filled with red blood cells and are in a state of partial dissolution exactly like during menstruation.* The epithelium loosens from the glandular walls and disappears among the blood corpuscles. The delicate connective tissue of the gland wall becomes loosened -and is dissolved; the further the ovular envelope moves toward the periphery, the more the glands become displaced. Their outer walls are flattened, their inner walls dissolved. Certain sections (37 to 105) show this process very plainly. It is best observed by following the three longest. The one in shape of an arch, reaches the ovum and partly encircles it, the second passes to the right, the middle one ends blindly near the ovum and as its cavity expands, gradually disappears.
1 Leopold, Studien ueber die L T terus Schleimhaut (Archiv. f. Gynaek Bd. XI).
2 Gebhard. Pathol. der Weibl. Geschlechtsorgane.
3. Sellheim-Nagel. Handbuch der Phyiol. des Menschen, II 1, pages 96 to 98. Figs. 38-41.
4. Nagel. 1. o. Fig. 41.
The Figs. 14 (Plate VIII) and 23 (Plate XIII) show especially the arches formed by the left and right glands. In Fig. 22 (Plate XII) we see only a trace of the end of the middle gland, whereas in Fig. 24 (Plate XIV) the section 165, which lies further away from the ovum proper, again shows the end of the middle gland, which is dilated and filled with blood, (dr.)
From this can be seen that the glands are considerably dilated and hypertrophied. The "Eianlage" acts as a foreign body and presses the glands toward the wall. The "Eianlage" furthermore, together with the free extravasated red blood, destroys and dissolves glands and thus helps to form the intercommunicating blood spaces of which we will presently speak. None of the sections furnished any proof for the assumption that the glands open directly into the ovular chamber, or that the ovum entered the mucosa through the mouth of a dilated gland. No signs were found of any well preserved glandular epithelium or even rests of such lining this cavity. This is furthermore made improbable since, as we have seen before, the glands in their entirety, including the walls and epithelium in the immediate vicinity of the . ovum, are dissolved as the result of its growth.
The mucous membrane elevation and all the adjoining tissue down to the muscularis, is very vascular. The structure and course of the blood vessels during the first weeks of pregnancy have been carefully described in a number of excellent works and we refer to them for further information. Here only those facts shall be emphasized which seem most important in connection with the very earliest stage of pregnancy. Since they are dealt with only in the work of Peters, a confirmation or further elaboration of his contribution would seem very desirable.
In the deeper portions of the mucosa, especially in the thicker layer of the decidual trabeculae, one still meets with little arteries twisted like cork screws. As a rule they are found cut either transversely or lengthwise, the latter often accompanying the glands for a long distance. On cross section the capillaries show around their endothelial lining a second and sometimes a third delicate ring of endothelium. The closer the ovum is approached, the greater becomes the number of capillaries and the greater is their distention and the extravasation of red blood cells into the surrounding tissue. .If the delicate wavy walls of these distended capillaries are carefully examined, it will be seen that at certain places there are defective areas or even tears, through which the erythrocytes escape into the adjoining tissue. They loosen the glands and detach the swoolen epithelium which now lies crumbled in the gland duct. In this way a coalescence of glands and capillaries is effected which in the neighborhood of the ovum results in the continuous formation of new intercommunicating blood spaces. If Figs. 7 and 8 ('Plate IV) marked "c," are carefully studied, this process can be better understood than describing the same. Figure 14 (Plate VIII) is still better, in which c and c indicate the adjoining cavities filled with blood.
The confluent blood spaces are best seen in Fig. 22 (Plate XII) where "c" shows fine septa as the remains of the tissue which at first separated the glands from the capillaries. As the "Eianlage" grows these septa become still thinner and are finally completely dissolved, so that at "c" the blood spaces are in direct communication with their neighbors c l and c 2 , and the latter again with the ovular chamber and its blood spaces. Attention is here called to the fact (which later on will be dealt with in detail), that the trophoblast processes have anchored themselves to the walls of these spaces at c x and c 2 . Thus it is self-evident that in the entire periphery of the ovum these trophablast processes are surrounded and nourished by connecting blood spaces. These conditions are seen more distinctly in section 94 (Fig. 23, Plate XIII). At "c" a broad blood space runs almost parallel with the glands to the ovular chamber. At c l another one passes from the left inward and breaks up into several blood spaces which communicate with the ovular chamber. It is best seen at c 2 , where a dilated capillary, running to the left and upwards, like through a slit, appears in the cavity.
A striking similarity is obvious, if we compare these pictures with those in my atlas ("Uterus und Kind" plate VI) illustrating injected intervillous spaces in the fifth month of pregnancy, which communicate with vessels of the serotina. It seems justifiable to deduce from Figs. 22 and 23, that already in the first days of pregnancy, as described by Peters and myself, the capillaries, through their dilatation, their breaking up into the surrounding tissue and their dissolution into enormous blood spaces which communicate with the ovular chamber, form the first rudiments of the intervillous spaces.
How do these statements compare with those of Peters, Graf von Spec (1. c. pg. 2.) and the various researches made on animals, as compiled by Pfannenstiel 1 ? In this early stage Peters has also observed decidual cells. He could not find a sharp division in the mucosa between a compacta and spongiosa.
1 Winckel. Handbuch der Geburtshilfe. Bd. I. 1, pg. 194.
The mucous membrane elevation in which his ovum lies, protrudes but slightly and still has a superficial epithelium covering its margin. The glands are greatly dilated, lie around the ovum meridionally and also have no communication with the ovular chamber, the latter pressing them aside. In his sections also various uterine glands (Plate I) are seen filled with blood, the surrounding of the ovum containing an enormous wealth of greatly dilated capillaries which in part are changed .into wide blood spaces exactly as in my specimen. In his Plate I, a large blood space is seen to the right and below, like an extravasation surrounding almost half the periphery of the ovum, communicating freely with those blood lacunae in which the trophoblastic processes are directly immersed.
Although the similarity between Peters' and my specimen is striking, still attention must be called to certain apparently existing differences. In Peters' specimen the trophoblast everywhere lies in direct contact with the inner wall of the envelope of the ovum and an embryonic rudiment is plainly visible. In my specimen, on the other hand, the trophoblast has not as yet everywhere reached the inner wall. It still partly floats, in the blood which fills the ovular chamber. In spite of repeated and careful examinations no trace of an embryonic formation could be detected.
Whether this floating of the trophoblast in the blood of the ovular chamber and the absence of an embryonic "Anlage" is possibly only due to a pathological extravasation of blood between the ectoblast and mesoderm, is still a question which, must be decided later. This difference, which in this connection is simply registered, is striking and might warrant the question, whether the ovum in my specimen is not possibly a few hours younger than that of Peters, and, whether within the next one-half day the junction between the trophoblast and the inner wall of the ovular envelope would not have been completed. This, however, must 'remain a mere assumption until other specimens of such an early stage have been found.
At any rate the same vascularity which is observed in our two specimens, is also found in the uteri of animals. "The changes in the maternal mucosa surrounding the ovum, in the various mammalia, are differently described. A formation of new vessels in the immediate neighborhood of the chorion, often to a great extent, is regularly found. In advanced stages noticeable vascular changes also occur in the deeper layers of the mucous membrane 1 ."
1 Pfannenstiel in Winekel 1. c. pg. 198.
"Very important are the results of researches made on animals regarding the first relation between the surface of the ovum and the vascular system of the maternal mucosa. This relation is established very early, both in the insectivora and the rodents. The ectoblast thickens at the placental site by the formation of numerous layers and lacunae soon form which become filled with maternal blood. The manner in which the blood gains access to these spaces is not sufficiently understood, but it is certain that the new formation of maternal blood vessels near the ectoblast is enormous and that from them the ectoblast lacunae receive their blood supply."
"The maternal blood from the very beginning remains in a closed channel and in regular circulation. Frommel has demonstated the same conditions in the bat. In the carnivora, e. g., the cat, these maternal vessel walls are also preserved in the placenta. The significance of this fact for human placentation is evident. In animals the "intervillous" spaces appear very early; they are filled with blood from the very beginning and are in constant and lasting communication with the maternal blood vessels. These same conditions no doubt also prevail in the human."
From the above description this presumption is proved a certainty, even for the earlier stages of the human ovum. '
The vascularity of the mucosa in my specimen, in its relation to menstrual conditions, is still another subject worthy of consideration in this chaper
Peters estimates the age of his ovum as from 3 to 4 days by assuming a relation between it and the menstruation which for the first time had just failed to appear. He bases his assumption on the history of the case and on the histological condition of the decidua, which, "in every respect resembles the description given of decidua menstrualis immediately preceding menstruation." 2
From the history Peters endeavors to show that on the day of her suicide (October 1st) the pregnant woman was about to menstruate. From the state of development of the Eianlage and the entire ovum itself, no other conclusion could be drawn, save that this represented the impregnated ovum of the expected menstruation. Based on these facts he estimated the age of the ovum as possibly three to four days.
Although I agree with Peters in regard to the manstruationlike appearance of the mucosa, I cannot coincide with him in his calculations from the history of the case.
1 Pfannenstiel 1. c. pg. 200.
2 Peters 1. c. pg. 16.
We read' on page 3 of Peters' work that the woman had her last normal menstruation on September 1st, 1895. At the end of September (on September 28th, according to the normal type, and no statement to the contrary is made) the menses should have reappeared. They did not, however, return at the expected time, and the woman, fearing pregnancy, committed suicide on October 1st. This would be 3 to 4 days after the expected appearance of the menses. Or, if we assume from certain observations that the ovule escapes from the matured follicle about two days before menstruation, the suicide was committed five to six days after the expulsion of the ovum from the follicle and the impregnated ovule presumably would then be five to six days old. Probably it is only a lapsus calami when Peters on page 16 states, that the woman was about to menstruate on the day of the suicide ; he should have said that her death occurred about three to four days after the expected menstruation, which for the first time had failed to appear.
Whether or not this ovum be four or six days old does, however, not in the least diminish the value of this specimen, for by its examination Peters has certainly succeeded in throwing new light on the embedding theory of the human ovum.
An accurate idea of the respective age of such ova we shall have only after more such small ova have been described, of cases in which absolutely reliable histories have been obtained. At present one seems justified in associating his specimen with the first missing menstruation.
The same surely holds true of my specimen, even without a history, since there is not even a suggestion of a embryonic rudiment, of an amnion, etc., present, as was found .in 'Peters' ovum.
I am, however, willing to refrain from making any estimate of the age of my ovum. Later investigators who may have the good fortune to work with reliable specimens of cases in which accurate histories are obtainable, may then determine the age of my specimen.
Of a very similar character is also the ovum demonstrated by Graf von Spec in Kiel in 1905. It also comes from a woman who committed suicide by taking oxalic acid. "The mucosa of the uterine body, as is characteristic for pregnancy, was divided into irregular areas by deep furrows. One field immediately in front of the right tubal opening, on the anterior wall, was more prominent and had an umbilication with a marked discoloration. This aroused the suspicion of being the nidus of the ovum. Histologic sections made of this portion of the mucosa proved to be very satisfactory for examination and on demonstration through the epidiascope showed the following condition : Taking up about two-thirds of the free surface of this prominent mucosa area, in a cavity of the interglandular connective tissue of the mucosa, an ovum 1.5 x 2.5 mm. was situated. It had but few villi and contained an embryo in a very rudimentary stage. Between the surfaces of the chorion and uterine tissue, here and there, small quantities of blood could be seen which escaped from ruptured vessels. The walls of the ovular chamber were entirely made up of elements of the interglandular connective tissue. All the glands opened into the uterine cavity, none into the ovum chamber. Like the ovum of Peters, the serotina, i. e., the mucosa, between the ovum and uterine muscularis, contained, within greatly dilated endothelial tubes, large blood clots apparently formed still during life. This blood served a double purpose, furnishing nutriment to the ovum and protecting the deeper portions of the mucosa against the corrosive action of the ovum. That portion of the envelope of the ovum which separates the cavum of the uterus from that of the ovum, consisted of a thicker or thinner layer of interglandular connective tissue covered towards the uterine lumen by a single stratum of epithelium."
Thus it can be seen that also in this specimen the ovular envelope is formed by decidual tissue, none of the uterine glands open into it, and near the ovum, especially in the serotina, large blood masses lie in immensely dilated endothelial tubes.
II. The Embedding of the Ovum. The Capsularis. The Fibrin Cover ("Gewebspilz Of Peters”)
Since it has been established by Graf von Spec for the guinea pig and by Peters for the human being, that the ovule bores its way through the surface of the mucosa, it has become the duty of the later investigators to determine whether this is the only mode of nidation or whether not occasionally a circumvallation occurs arising from the mucosa surrounding the ovum.
Pfannenstiel 1. c. page 194, is correct in saying: "The ovum described by Peters is already completely or almost completely enveloped by the mucous membrane. In spite of the great value of this specimen, in spite of the fact that it has revolutionized our views concerning ovular nidation, we should not forget that this is the only specimen extant of this early stage of development and it would seem advisable not to go too far in its interpretation."
Which, then, are the similarities and which the differences between mine and 'Peters' specimen ?
First of all, it is to be noted that the mucosa elevation on the sides of the ovule almost up to the fibrin cover, is still covered with a surface epithelium (Fig. 3. e. Plate II).
Close to the fibrin cover the epithelium becomes irregular, is partly swollen and partly detached. In some, sections (Figs. 7 & 9, e,e, 'Plates IV & V) it extends like in Peters' specimen (Plate I U.E.) under the fibrin cover, as a narrow band. At the^ slope towards the furrow (F) it is practically absent.
Special stress is to be laid on the fact that under the center of the fibrin cover where it lies closest to the summit of the ovum, no more regular surface epithelium is met with. Likewise nowhere within the ovular chamber can even a trace of epithelial lining be found which connects with the surface epithelium.
One peculiar condition which appears only in the sections 15-19 (Figs. 5 & 6 Plate III) must be described. in detail. To the right, below the center of the fibrin cover, a depression (e. s.) is noticed which is lined by a few cuboidal cells (Fig. 5) whose resemblance to epithelial cells cannot be denied. Among them, however, are a few broader cell bodies with large nuclei which are not unlike syncytial cells. This supposition is strengthened by the fact that with high magnification one can see a few large syncytial cells extending from the nearest trophoblast plugs towards the depression e. s. (More details will be given in a later description of the trophoblast, Fig. 10.)
This funnel shaped depression is still distinctly visible in Fig. 6 at e. s. Here, however, it is filled with red blood cells which have escaped from the ovum chamber and in their- further course cannot be differentiated from the blood cells which infiltrate the structureless fibrin mass. (Fi.)
This funnel shaped depression seems worthy of special note and probably deserves to be particularly considered in all future investigations. It is certainly the only visible and partly preserved connection between the ovular chamber and the uterine cavity.
What will be its significance? It might be regarded as the remains of a glandular orifice, yet much speaks against this. First of all there is no gland opening anywhere within a wide area of this spot, especially outside of the fibrin cover. Naturally so, since the glands have been displaced by the ovum and lie more meridionally. We have already shown that the glands do not take any direct part in the formation of that cavity which harbors the ovum and that this chamber nowhere in its interior carries a lining of uterine epithelium. If this funnel was actually a gland orifice the good preservation of its cells would be striking in contrast to the glandular openings still visible to the sides of the ovum, since their epithelial cover consists almost only of swollen, detached and liquified cells.
The question suggests' itself, however, whether this funnel shaped depression does not indicate the site where the ovum has entered the mucosa. My ovum does not show any "Anlage" of an embryo and therefore must be younger than that of Peters, in which an amniotic cavity with an exocoelum is distinctly visible. The assumption may be justified that my ovum has just accomplished its nidation and is about to become sufficiently anchored to the ovular envelope by sending out trophoblastic processes. The fact that this place at e. s. represents the only visible connection, obviously leads to the question, whether or not the ovum has possibly here entered the mucosa. This place is certainly about to become obliterated by the encroachment of decidual cells from both sides, but there is still a relation extant between the interior and exterior. At a place within the blood filled space of the ovular chamber lying closest to the depression e. s. (in Fig. 6), an escape of red blood cells can be followed, one sees how they collect at e. s. and from here permeate the fibrinous cover. Thus one seems justified in assuming that also the fibrinous cover has originated here, that it serves more or less as a lid and that it is supplied with red blood cells until the envelope completely surrounds the ovum.
Before the structure and development of this fibrinous cover is considered in detail, the process of embedding of the ovum, and the ovular chamber must be considered. In all sections (Figs. 14, 22 & 23, Plate VIII, XII & XIII) the decidua completely surrounding the ovum, shows the indentical histological structure. Although varying in thickness at different places, especially at the summit of the ovum and at both sides of the mucosa elevation, the decidua everywhere consists of thin wavy fibres containing larger and smaller decidua cells, numerous capillaries and a large number of extravasated red blood cells. One can therefore not say that the mucosa has reflected itself from the two sides over the ovum, lying in its chamber, nor can assert, that a scar can be seen on the summit of the ovular elevation.
Everything points rather to the fact, which has been proved by Peters, that the ovum has burrowed its way into the mucosa, in our specimen somewhat asymmetrically in a mucosa elevation. The point of entrance in our case has become almost completely obliterated, but there still persists a narrow channel from which some blood oozes, the latter accumulates at the summit of the ovum and becomes transformed into the fibrinous cover.
It Peters' specimen the connective tissue does not as yet form so complete an envelope as in mine, in which the ovum has possibly already penetrated to a greater depth. In his case, therefore, the opening still existing in the decidual envelope is covered by a broad layer of fibrin partially organized. It is called by him the "Gewebspilz." The trophoblastic processes with their syncytial excrescences are directly attached to it
Concerning the clos.ure of the defect through which the ovum has penetrated, 'Pfannenstiel (1. c. page 220) has expressed himself very carefully. Since at that time Peters' specimen was the only one known, he considered the process of closure as uncertain. Descriptions of very young ova as given by Peters, Graf von Spec, Heukelom, Leopold and Keibel had stated "that at the point of closure not a distinct decidual tissue but a scar tissue is found, consisting chiefly of fibrin and showing an absence of blood vessels, also he himself was able to confirm the presence of this fibrinous scar tissue, he would not consider this question definitely settled since the formation of fibrin within the decidual envelope of the ovum is very common and often can be traced to an entirely different cause. It would seem possible that the final closure of the decidual capsule around the ovum is accomplished by a firm coalescence of the vascular connective tissue which proliferates from opposite sides. At this place, which is the most poorly nourished portion of the reflexa, soon afterwards signs of degeneration would appear especially so in ova which are more superficially embedded. The blood plug of Peters thus might possibly be considered an abnormal condition.
The assumption of Pfannenstiel that the ovum has an entirely decidual envelope is confirmed by my case, with the exception of that narrow opening at e. s. As mentioned before, it is caused by a deeper implantation of the ovum. Nevertheless, there is in our case, like in that of Peters, a large and very broad fibrinous cover lying over the top of the ovum, so that such a cover must form even in case of complete decidual inclusion. In any explanation, however, of the origin of this fibrinous cover one must consider this narrow opening through which the ovum sank (e. s. Fig. 5 & 6) and whence that tiny amount of blood has oozed to the surface and there coagulated.
In order to obtain a clear conception of this fibrinous lid one must first of all gain a precise idea of its form, length, width and structure. It can be seen in the microscopic sections from 10 to 70, then again from 75 to 103 and a trace of it finally in section 119.
The entire 160 microscopic sections are embedded so that the slope of the mucosa elevation with the furrow (F) lies to the right of the specimen and all illustrations follow the same rule. It will thus be perfectly plain, if in describing this fibrinous cover the term "left," applies to the direction toward the uterine fundus, the term "right," toward the slope of the mucosa elevation and the furrow (F).
If for the purpose of reconstruction, the various sections are placed together, one receives the impression, in a view from above, that two minute drops of coagulated blood lie on the mucosa elevation near its slope. The larger drop lies more towards the right edge of the uterus, the smaller and flatter one to the left. Still farther to the left in section 119 a trace of a coagulated mass can be seen.
All sections through the larger drop show its right half considerably thicker and more voluminous than the left. On the sections through the center, the fibrin appears in rolled up waves like a congealing substance. (Figs. 7, 9, 11, 14, 15. Plates IV, V, VII. VIII. IX.) In explaining this condition one must consider that this thicker portion is situated exactly over the fine fissure (e. s.) through which blood is still oozing from the ovular chamber. On the other hand one must keep in mind that the escaping drop, both in the lying or standing position of the woman, must gravitate downwards, i. e., in the direction of the slope of the mucosa elevation.
The size and structure of the fibrinous cover as well as its relation to the ovular chamber can be best understood from a study of some of the illustrations. In section 10 (Fig. 4, Plate II) the cover suddenly appears. It has the shape of an oblong cylinder, somewhat thicker to the right, whose left lower edge is intimately connected with the decidual envelope of the ovum. From the left some surface epithelial cells, already irregular, penetrate under the edge of the cover (e). On its surface lies a band varying in thickness that possibly consists of surface epithelia of the mucosa, which, however, are not discernable as such. The cover itself consists of a mass of fibrin in which here and there white and red blood corpuscles are met with.
Almost identical conditions are found in sections 15 and 19 (Figs. 5 and 6 Plate III), only that in Fig. 5, in the band on the surface, a few cuboidal epithelia can be seen, whose origin failed to determine.
In sections 22 (Fig. 7) and 27 (Fig. 8 'Plate IV) the fibrinous cover appears in a considerably changed form. Like a catterpillar with a large head, it lies on the ovular envelope, which has become thinner. Under its right and left edge (Fig. 7) traces of surface epithelium are seen. Its superficial portion contains a few white blood cells, in its interior a delicate network of fibres. Most conspicuous, however, is the folded appearance of the coagulated .mass to the right (Fig. 8 fi) which depresses the ovular envelope.
These conditions are most plainly visible in Fig. 9 (Plate V) and Fig. 11 (Plate VII). In the latter, representing section 30, at fi., fibrinous masses, like frozen waves, are heaped one upon the other, causing a deep indentation of the walls of the ovular chamber. In Fig. 13 the fibrinous masses contain a large amount of white blood cells, still more of them in Figs. 16 and 17, while in Fig. 15 the clubbed end of the cover is the thickest. Here over the depressed portion of the ovular envelope the fibrinous masses are arranged exactly like in a corpus luteum in the stage of organization.
Gradually the arrangement and signs of an organization make their appearance in the fibrin cover in form of connective tissue fibrils. Thus a sort of new formed protective layer develops over a portion of the ovular envelope. This portion in itself is very thin, but is further weakened by trophoblastic processes which, as will be described later, for the purpose of fixing the Eianlage, have penetrated into the summit of the ovular chamber. (Compare Peters.)
The formation of a protective cover for which the escaping blood droplets have been utilized, must be regarded, as has already been emphasized by Peters, an exceedingly important process and a wise provision of nature.
If Figs. 18 and 19 (sections 68-69) are compared it will be seen that the left portion of the fibrinous band has undergone a certain organization and reenforces the ovular envelope. The right clubbed shaped end is a mass of twisted fibrils which has gradually decreased in size and like a button (Fig. 19 kn) lies in a depression.
Since with section 70 the larger of the coagulated drops disappears, it must be assumed that the surface between sections 70 and 75 (Figs. 19 and 20 Plate XI) is free of any fresh deposit of fibrin, carries, however, the continuation of the organized portion.
In section 75 (Fig. 20) suddenly a new fibrinous layer appears. To the left of the mass, which is in a state of organization, lies a band varying in thickness which resembles the rests of surface epithelia and extends upwards along the edge of this new fibrinous cover, thus the observation described above is practically repeated. Again the cover becomes oblong but in this instance is thicker in the middle portion, but in general does not attain the length or thickness of the fibrinous cover previously described. There are a few white blood cells in its middle part. With section 105 this fibrin band has again disappeared, here (Fig. 24 Plate XIV) the ovular chamber being cut more laterally shows a thicker wall while in the preceding sections the fibrinous cover seemed to play the role of a reenforcement for the ovular chamber and of a protective layer, as was clearly shown in the pictures of the first mentioned larger fibrinous mass.
Concerning a fibrinous cover (Gewebspilz) in the ovules of Graf v. Spec (Kiel 1905) and of Beneke, we find the following references : Van Spec says on pg. 422 : "At the site of the funnel shaped depression the uterine tissue shows a defect which must be regarded the gate through which the ovum entered the endometrium during the process of implantation. This opening is sealed by a flat blood coagulum (fibrin, containing leucocytes and red blood cells). Thus the conditions are very similar to those described by Peters. The opening which appears with a diameter of not more than 0.8 mm., possibly is larger than at first produced by the ovum. This increase may be due to the stretching and* growth, possibly also to a histolytic action of the ovular wall."
Beneke reports on page 772: "The tissue plug (Gewebspfropf) which closes and fills the defect in the reflexa in general corresponds in its histologic structure to that described by Peters. It contains blood, fibrin, leucocytes, etc."
After this description one's attention obviously is again drawn to the question of the similarities and discrepancies between mine and Peters' ovum.
Up to this point both specimens are identical in all essential features.
In both we see the decidua vera in a condition of edematous infiltration. In both the ovule lies in a swollen mucosa near a furrow, in both instances the ovule has penetrated into the mucosa at a place deprived of epithelium and has pushed aside the tissue and the glands so that the latter follow a meridional, curved course. Over the top of the ovum the edges of the mucosa have approached each other in an attempt to close the ovular chamber completely. This process has progressed further in mine than in 'Peters' specimen. In both cases on the top of the arch, where the ovum has entered, a blood coagulum is found serving as a protective covering, which in Peters' specimen resembles a mushroom, in mine a caterpillar with a large head.
This variation in shape so well pronounced in all my sections, calls for a more appropriate name. Peters' term "Gewebspilz" certainly cannot be applied to my specimen. With the idea that such an expression should be applicable to all later cases it seemed most natural to select the term "fibrinous cover" (Fibrin decke). Whatever its name may be, however, the fact remains that in these two youngest human ova it was present, large and well developed. This explains the peculiar rests of fibrin found on the top of the ovum in older specimens, as, e. g., described in my atlas (Uterus und Kind, Plate I).
As first shown by Peters, our specimen also proves that the old circumvallation theory of the formation of the reflexa is incorrect, but still a reflexa is present. If one drops a stone into the water the latter closes over it and if an earth worm burrows itself into the ground, the hole made by it will again gradually be filled with the loosened soil. 'The rapidity with which it becomes closed will depend upon the character and structure of the soil.
It seems permissible to call rcflc.va in Peters' and my specimen, those decidual arches which approach each other approximately over the center of the ovum. One must, however, keep in mind that these arches have not newly formed and closed over the ovum, but that as a matter of fact, they have existed from the first beginning and that through them the minute ovule has burrowed its way. The arches become higher the more the ovum grows. It is obvious that the opening between the arches, i. e., the passageway of the ovum, finally again becomes closed by either a fibrinous plug or a fibrinous band.
In the following it will be shown that the great similarity existing between the microscopic pictures of Peters' and my specimen, leads to a like interpretation of the findings.
Peters (pg. 28) emphasizes that his ovum has become implanted in the swollen mucosa near a furrow, the same has occurred in my case. Since the uterine mucosa prepared to receive the ovum is traversed by numerous deep furrows, he thinks it might possibly happen "that the minute human ovule could be caught in such a groove and then actually could become embedded (exactly like the ovum of the erinaceus) if the edges of the furrow coalesced and finally closed." "In such an instance, however, the ovum would be completely encircled by a uterine epithelium and surely one or the other gland would be found opening into the ovum."
I agree, that an ovule in this way might enter such a furrow and be caught, but still it could there sink into the mucosa, but even if it should further develop while wedged in this groove, I cannot see the necessity that it should remain surrounded by uterine epithelium and that as Peters explains this protecting maternal layer should then be secondarily destroyed by the proliferation of the fetal trophoblast.
In the premenstrual stage the epithelium of the uterine mucosa is loosened, swollen and rendered detachable by small subepithelial hemorrhages to such an extent that an intact, firmly adherent and continuous epithelial covering in such a furrow could not be expected and hardly ever is found. Therefore, from an anatomic histologic point of view, I cannot object against the possibility of ovular implantation in a furrow and would not regard it as surprising if a gland would run up to the ovular chamber (compare Fig. 24 dr t Plate XIV) and apparently open into it. Such facts do not alter my present assumption that the ovum passing through the superficial epithelium and pushing the glands aside, burrows itself into the mucosa.
In my opinion, it matters not where the ovum has become attached and where embedded, whether on the summit of a cotyledon (as in 'Peters' case) or near the slope of an elevation, as in my specimen, or in a furrow, the ovule will everywhere be the source of considerable irritation and a pronounced reaction in the adjoining tissues. This reaction has been so well described by Peters that I give my own opinion by simply citing his own words (pg. 29) : "One seems justified in assuming that at the site of implantation, either through mechanical irritation or by a provision of nature, the tissues become highly congested, plasma (edema) and corpuscular elements of the blood extravasate, the preformed endothelial tubules dilate, the mucosa swells and thickens. It still remains undecided in which manner the blood elements are set free, whether as a result of an increased pressure within the vessel or through rhexis or a free diapedesis, or possibly the capillary vessels have been opened by the epiblast, which has begun to proliferate as soon as it came in contact with the maternal tissues. The fact that the fibrinous plug which lies on the summit of the ovum pointing into the uterine lumen, consists of blood elements, almost forces us to assume that during the process of the embedding of the ovum into the edematous connective tissue stroma, the ovum, and its free surface towards the uterine cavity, is surmounted by a blood coagulum which protects it and possibly furnishes nutrition for that portion of the ovular surface which as yet has not established its connection with the maternal tissue."
If we compare the histologic pictures of our specimen- with this description, the sections 15 to 19 call for special attention, because they plainly prove the minimal but quite noticeable escape of blood from the ovular chamber into the fibrinous cover. We have also seen how the left half of the fibrinous lid has become more and more organized and in this way reenforced the decidual envelope and how to the right the large head of the fibrinous band, which lies in an indentation of the ovular chamber, closes the opening of entrance.
Still other similaraties can be detected. In Peters' ovum (Plate III, Fig. 4) there is also a lateral and central depression in the fibrin plug, so that the fetal ectoblast almost immediately touches it. On the other hand in his specimen the trophoblast processes also penetrate into the decidual layers over the summit of the ovum, so that in some places they become extremely thin and appear worm eaten.
Finally, it shall here be mentioned (Peters, pg. 44) that the envelope of the embryo of Graf v. Spec was surmounted by a flat blood coagulum.
III. The Eianlage and the Ovular Chamber (Eikammer)
\Vc have seen that the o.vule has burrowed itself, gradually pushing aside the decidual tissue. Some of the glands were dissolved, others displaced. The blood vessels were in a state of ^narked congestion, multiplication and coalescence. This shows clearly how the ovular chamber, especially its summit, consists <of decidual tissue and how large blood spaces adjoin its inner surface. These blood spaces are divided by trophoblastic columns and communicate directly with the surrounding capillaries situated in the wall of the ovular chamber.
In the next chapter these intercommunicating capillaries and irophoblast processes with their attachment to the inner surface oi the ovular envelope, shall be considered.
Here we shall first of all speak in general of the "Eianlage v (Fig. 18, Plate X). An exact idea of the form of the Eianlage could be gained only by a reproduction of pictures of all consecutive sections, which, for obvious reasons is impossible.
Studying only Fig. 18, the sections 60 to 70 and 80 and 81 in rir.te XI, Fig. 21, one gains the impression that a somewhat irregularly shaped structure lies almost in the center of the ovular chamber from which mesodermic processes extend from all sides. Some of these processes are covered with an ectodermal layer (Fig. 18 ekt.).
Here and there the ectoblast layer (e. g., at ek^) is detached by an extravasation of blood under it. This does not seem to be normal. At present, however, we must leave the question undecided how far this condition is pathologic or still physiologic in this earliest stage of development. The number of very young human ova so far known to us is still too limited, on the other hand in our case the ovule and the entire mucosa of the uterus is so well preserved that this one feature, even if pathologic, could not diminish the value of the other fiindings.
Considering the form of the Eianlage as it appears in our own specimen, we find in a series of consecutive sections that it is attached with a broad base to the inner wall of the ovular chamber near its summit (Fig. 18 a). This attachment is firm and the tissue is here also slightly permeated with red blood cells. If permitted to make a comparison one could say that the ovule sticks like a leech with its head to the inner wall of -the ovular envelope, while the rest of the body is suspended in the cavity. In order, however, to avoid any misunderstanding it is here stated that already in this stage long trophoblastic processes extend from the irregularly shaped Eianlage (Fig. 18, tr, tr, Plate X) which are attached to the chamber wall, and in this way, like thin threads, fasten the apparently floating ovum.
Even under very high magnification this Eianlage is apparently composed only of a congealed mass, traversed here and there by structureless, very delicate fibres, the latter passing chiefly along the sinuous periphery of the Eianlage. The actual contour, however, in the main is formed by small round or oblong cells with deeply stained nuclei which in connection with the transparent network of fibres create the picture of villous tissue, i. e.. of the "Anlage" of the mesoderm.
Before entering into a consideration of the trophoblast and its attachment, it may be well to recapitulate what has been said before. It seems important ' to have a clear conception of the condition of the ovum after it has entered the mucosa and of the condition of the endometrium at the time when the ovum is entering it. We assume that the most suitable time for implantation of the fertilized ovum is the last few days preceding the first missed menstruation.
In the premenstrual stage the mucosa is not only congested, but as is shown in Fig. 25, Plate XV, permeated by extra vasated blood. According to Gebhard, a second stage follows characterized by an accumulation of large extravasates in irregular lacunae of the mucosa. As a result of the rupture of some capillaries beneath the surface epithelium, subepithelial haematomata are formed from which, after slight detachment of the epithelium, blood escapes into the uterine cavity as -the visible menstrual flow.
The blood which has escaped from the capillaries thus spreads both beneath the epithelium and in the deeper layer of the mucosa as an irregular extravasate and also enters the glands (Gebhard). One must therefore bear in mind that this free blood lies chiefly in artificial cavities, not lined by an endothelium.
The fertilized ovum which in the premenstrual stage, i. e., 'before the menstrual flow has appeared, is about to enter the uterine mucosa, finds a markedly loosened tissue infiltrated with blood and will hardly experience any difficulty to pass through or push aside the loosened surface epithelium.
When the ovum has penetrated the superficial layers of the endometrium it is in a tissue permeated by the extravasates just described and lies either free in one of these extravasates or at least at the edge of one of them in the tissue of the mucosa. At any rate, we seem justified in assuming, that the fertilized ovum, immediately after its implantation, displays great vitality, that it will develop and that above all things it will attempt to fasten itself, which probably is most quickly accomplished by extending the first trophoblast processes.
My idea is, that the embedded ovum, for a very short time, either partly or completely, lies in a blood extravasate. Since these blood spaces have formed as a result of a rupture of capillaries they are devoid of a continuous endothelial lining and show an endothelium only at places where ruptured capillaries enter.
The ovum thus floats, possibly only for the first few hours, in a blood cavity, i. e., it is from the very beginning surrounded by a maternal blood from which it receives its nutriment. When and how quickly the entrance gate is closed again we do not know, it is possible that this, process varies as to mode and time. Many observations, however, suggest that the closure is effected by means of a drop of blood which coagulates and later becomes organized. (Peters, Leopold, Graf v. Spec.)
That it should be closed by a blood drop is not at all surprising, since the ovum breaking into the mucosa, so to say, has set a small wound and has opened up a blood cavity. From the latter a small amount of blood could easily ooze. This, then, would at the same time be the most natural process o*f restoration of the injury produced by the process of embedding.
Without these preliminary remarks it would be rather difficult to understand the following chapter dealing with the trophoblast.
In studying the trophoblast I had the same experience as Peters. The microscopic pictures are so varied and oftentimes so complex that it requires considerable time to properly interpret the findings. One often wonders what bold conclusions were drawn by onesself and other writers, concerning the very early stages of development, from the study of ova representing a much later period of pregnancy.
It is obvious that it should be the aim of both gynecologist and pathologic anatomist to search for all available material in order to place our knowledge, concerning the first days of embryonic life, upon a more secure basis.
After having followed the ovule up to its entrance into that irregular blood space of the mucosa, it becomes interesting to understand the action and functions of the ovum for the purpose of sustaining its existence. This is accomplished chiefly by means of the trophoblast.
IV. The Trophoblast andits Surrounding Blood Spaces. The Intervillous Circulation
In presenting this subject the following order seems the most appropriate : With the aid of sections 50 to 100 taken from the center of the ovum we elucidate :
- The boundaries of the elanlage and the trophoblastic processes.
- The manner by which these trophoblastic plugs become fastened to the inner wall of the ovular chamber.
- The blood spaces lying between the trophoblastic processes.
- The relation of these
Blood Spaces to the Confluent Capillaries in the Surrounding Tissue
ad. 1. In Figs. 16, 17 & 18 (Plates IX & X), the ectoblast cover and the trophoblast processes are seen. We are able to follow both their primary condition and further development.
The ectoblast (in Fig. 18 ekt. and Ek^. Figs. 16 & 17 ekt. and Figs. 26 & 27 Plate XVI) consists of a double row of cells. The inner row is composed of round, in some places oval cells adjoining each other with their pole ends and containing a dark stained nucleus which almost fills the cell. (Langhans' cells Figs. 26 & 27 1. z.). On the outside of this cell layer we find much larger cells which contain one or more nuclei. Many of these cells are considerably swollen, showing a fine granulation of their cellular substance (Syncytiurh). (Figs. 26 & 27 sy.) In following this ectoblastic band, which here and there is detached from the mesoblast, in the sections 47 and 60 represented in Figs.
16 & 17, we can establish several facts. At various places (e. g., Fig. 17 k) by a proliferation of the Langhans' cells the inner layer is thickened, forming small buds covered by the syncytium. These buds gradually become thicker and longer (Figs. 16 & 17 tr & Fig. 18 tr to the right), but almost everywhere remain covered with syncytial cells, as can be recognized in Figs. 16 & 17 under high magnification from the double layered band marked "ekt." (Fig. 27 sy.)
The ectoblast in this stage of delevopment has already sent out a number of short sprouts, but the mesoderm which is just forming has not as yet entered these processes, so that one cannot speak of villi in the usual meaning of this term.
It must, however, be emphasized that these earliest buds as well as the further developed processes (the ectoblastic band in Fig. 16) are completely surrounded by maternal blood and do not come in contact nor have any connection with the maternal tissue, especially decidual cells.
While this fact alone proves the close relationship of these two cell layers to the ectoblast, furthermore, in this stage of development of the ovum absolutely nothing speaks in favor of an assumption that the ectoblast or possibly its external cover the syncytium, etiologically has any relation to the maternal tissue. The ectoblast is a part of the Eianlage, its buds are the expression of the development of the latter. Without an Eianlage neither a formation of trophoblast nor a proliferation of syncytium is conceivable.
Following further the increase in the size of the trophoblastic buds (e. g., Fig. 18 tr. to the left; Fig. 16 tr to the left; Fig. 21 Plate XI; Fig. 22 tr, tr; Fig. 23 tr Plate XII & XIII) one notices that the Eianlage, besides these finest processes, gradually sends forth larger ones which tend to reach the inner surface of the ovular chamber. Peters has very appropriately (pg. 91) compared these trophoblastic processes to the arms of an octopus.
Here also nothing can as yet be seen of an extension of the mesoderm into these trophoblastic buds. It seems that first of all the ovum attempts to gain a firm hold and only later it proceeds to form true villi by the proliferation of the mesoderm.
ad. 2. How and where do the ends of the trophoblastic processes become attached to the wall of the ovular chamber?
In order to answer this question we must study not only the sections through the middle, but especially those through the lateral portion of the ovum. (100 to 120.) A very notable finding can be recorded. In speaking of the Eianlage it has been stated that it is attached like a leech with a broad head to the summit of the ovular envelope, but that here also the attachment is effected by a thin layer of ectoblast containing syncytial cells.
In looking over the sections through the lateral portion of the ovum one notices that coincident with the gradual disappearance of the Eianlage, broad trophoblastic processes and columns along the whole periphery of the ovum but especially near its summit, like a network, connect the Eianlage with the chamber walls.
The processes and columns consist of oval Langhans' cells darkly stained, closely pressed together and filled with round and oblong nuclei. Everywhere, especially so laterally, they are covered with large syncytial cells, some of them oblong irregularly shaped, others standing on their edge filled with oblong crescent shaped or with small nuclei tightly pressed together.
The ends of these processes with their syncytial cover have penetrated deeply into the thin layer of tissue over the summit of the ovum (Figs. 16 & 17 sy. Plate IX). Here, where the covering fibrinous band has almost disappeared, we meet with conglomerations of syncytial cells. Lying close together they almost create the impression of rests of surface epithelium (Figst 12 & 13 sy. Plate VII) ; yet their connection with syncytial cells emerging from deeper layers is so evident that any idea of their relation to rests of epithelium must be repudiated. There is still another fact which prohibits such an assumption. It has been mentioned several times that from the surface of the mucosa a narrow, irregular band resembling degenerated epithelium creeps over the edge of the fibrinous cover. In these sections also, in which the fibrinous cover is still missing, appearing only in later sections, this band, although somewhat uneven, again appears. Since here and there distinct cuboidal epithelial cells are visible, one seems justified in pronouncing it surface epithelium, it then would be a swollen rest which has remained between the two coagulated blood droplets lying on the summit of the ovum. For this reason there can be no association between the epithelial like rows of syncytium and the surface epithelium. (Compare Peters' Plate V Figs. 10 to 13, the epithelial like arrangement of syncytial cells.)
From this explanation one can understand how in Figs. 11 & 13 (Plate VII) syncytial cells arising from trophoblast (tr) have become arranged in rows and finally terminate in a large cluster of cells, (sy.)
The same holds true as mentioned before for the syncytial process (sy.) in Fig. 10 (Plate VI), which originates from the trophoblast.
In rather regular intervals but forming quite irregular arches the trophoblast processes which at first have floated more or less freely in the maternal blood spaces, approach the inner surface of the ovular chamber (Fig. 6 tr. Plate III) and by means of these arches subdivide the periphery of the chamber into smaller blood lacunae. (Fig. 15 tr; Figs. 22 & 23 tr.) Thus these lacunae develop within the trophoblastic shell of the ovum as is so excellently shown in 'Plate I of Peters' work.
Since the trophoblast excrescences and processes, as mentioned above, are covered with a syncytium, it becomes obvious that these blood lacunae are lined with a syncytial layer which is plainly visible everywhere on the concave side of the arches. (Fig. 23 sy.) In this manner the syncytium forms a line of demarcation between the trophoblastic framework and the blood lacunae.
In comparing these blood lacunae in the periphery of the ovum one notices at once a difference among them which one really must expect and which also is noticeable in Plate I of Peters' work. The lacunae lying near the summit are more or less closed, while those situated in the depth and on both sides are, by means of narrow channels, connected with the large blood spaces in the decidua. This difference explains itself in the following manner: In the lacunae near the summit (Fig. 6 tr), the closure of the arches is effected by the thin wall of reflexa or by the fibrin cover, while this is impossible in the remaining portion of the periphery. Here the vessel walls are opened as a result of their rupture. (Fig. 6, c.)
Whether the lacunae appear more closed or open, in both cases the manner in which the ends of the trophoblast processes become fixed to them is the same. It is effected by means of smaller and larger single syncytial cells, at times by groups of them which glue these processes to the decidual tissue.
How intimate this attachment may become which, especially in the tissue of the summit of the ovum, could be called an anchoring, can be seen in Fig. 11 (Plate VII). Here the trophoblast, together with its adjoining syncytial cells, has buried itself deeply into the decidual coat and advanced to "sy" with one large giant cell. A similar condition can be observed in Fig. 11 at tr and tr 1} where the syncytial cells radiate from the trophoblastic processes in various directions.
In the periphery of the ovum the connecting syncytial cells attach themselves to the nearest decidual trabeculae or to the remaining portions of the walls of the enormously dilated and ruptured capillaries and blood vessels. Hereby a connection of the latter with the blood lacunae is established and maintained.
The syncytium therefore does not only serve the important purpose of fastening and anchoring the trophoblast, but during the further development of the ovum brings about the gradual dissolution of more capillary walls (Fig. 28 Plate XVI) and in this manner constantly provides larger and larger blood spaces for the sustenance of the ovum.
Now that we have become acquainted with blood spaces which lie between the trophoblastic processes (ad. 3), it will be necessary to explain (ad. 4) the relation of these blood spaces to the confluent capillaries in the surrounding decidual tissue. For this purpose sections 81 to 96 and also Figs. 22 & 23 (Plates XII & XIII) must be studied.
In looking over these sections one must keep in mind the fact that the ovum has entered a tissue which as a result of the premenstrual state was highly congested. Blood vessels as well as glands were greatly dilated. Blood extravasated from the capillaries, passed into the interstitial tissue and finally also found its way into the glands. Thus the Kianlage was surrounded and the ovular chamber formed by a very loose and spongy tissue infiltrated with blood consisting in the main of dilated capillaries, many of them ruptured.
No matter how many specimens we examine and compare, the same condition will be noticed in all. The inner wall of the ovular chamber, as already mentioned, is formed partly by dilated capillaries and partly by open blood spaces with their intervening framework. Since the open blood spaces only recently have been closed capillaries, their inner wall, not everywhere but almost throughout, is lined with an enclothelium. In the immediate neighborhood of the blood lacunae, in the loose tissue, numerous large syncytial cells are found singly or in clusters, some of them lying close to the chamber wall. These cells, so to say, are the pathfinders for the syncytimn, which glues the trophoblastic processes to the wall. For this reason a great number of large syncytial cells are met with in the sections which pass far laterally through the ovum. (Fig. 4 sy. Plate II.)
It is noteworthy that wherever a syncytial cell lies close to a vessel wall the corresponding endothelial cell on the inside, in comparison to others, seems enlarged and contains a very large nucleus which either is oblong or undergoing segmentation.
One could feel inclined to think that the transformation of the endothelium into syncytium is the primary result and that the syncytium develops further from here. One then could conclude that the syncytium in the main originates from vessel endothelium. In our specimen, however, no support whatever can be detected for such an assumption. As a matter of fact, the conditions are as follows : The syncytial cells which cover the trophoblastic processes and attach themselves to the walls enter the tissue, become disseminated between the capillaries and glands especially in the remaining framework of tissue. They attach themselves to the walls of the capillaries which are still closed, corrode them and thus constantly open new blood spaces. 1
This process, e. g., is represented in the sections 86 to 89. Here we see large rows of syncytial cells which advance from a trophoblast process towards the wall of a transversely cut capillary and attach themselves to cells of the wall. (Fig. 28 sy. Plate XVI.) In the next section syncytial cells pass into a vessel wall. Its various layers become detached from each other. The tissue cells which formerly lay in closed arches as well as the endothelial cells are now unraveled. In the next sections we see blood cells oozing from these unraveled vessel walls. The syncytial cells force their way deeper and deeper into the lumen. Finally one sees only half of the wall of the vessel until this, too, is dissolved. In this way the peripheral blood spaces, one after the other, are destroyed by the never ceasing action of the syncytial cells and from these findings the conclusion must be drawn that already, /. c., even in this early stage of development, the intervillous spaces are indicated and even existing.
1 At the Congress in Kiel, Peters demonstrated drawings which show beautifully how endothelial cells become detached and necrotic exactly at those places where syncytial cells have attached themselves to the outside of capillaries; another proof that endothelial cells do not transform into syncvtium.
Correctly we cannot as yet speak of intervillous spaces because the mesoderm has not yet entered trophoblastic process so that villi in the strict sense of the word do not exist. In Peters' specimen (Plate II) they have already formed. Therefore, it would be more appropriate in our ovum to apply to these blood spaces the term "intertrophoblastic."
It seems, however, not desirable to add new difficulties by introducing a new term. The reader acquainted with the subject will know what is meant and it would seem permissible to speak of an "Anlage of intervillous spaces" even in this stage, since very soon villi actually will enter these trophoblastic excrescences.
What can be attributed to the findings?
I am well aware of the fact, that although it lies completely in situ and has been carefully handled, still it shows in a few sections, an excessive amount of blood which, here and there, has pressed the Eianlage together and detached the ectoblast. Owing to this I hesitated in publishing my findings, but since in the main all those conditions which I wish to demonstrate were so plainly visible, and so instructive, I was finally persuaded to do so by 'Prof. Graf v. Spec.
I believe that the description of my ovum is of value so long as no other ovum of the same age or possibly a younger one still better preserved is known. I will therefore compare my findings with those made on the youngest ovum known in literature.
Peters has extensively quoted all those writers who have described older ova and carefully compared his findings. Thus I am justified in limiting myself here to his description and his critical review of the literature on the subject, and shall emphasize only points of importance in these new findings. For a consideration of this subject, only a few of the recent contributions will be considered, and this will also appiy to the following chapter dealing with the syncytium : Pfannenstiel in Winckels Handbuch der Geburtshilfe, Rossi Doria, 1 Marchand, 2 Friolet, 3 Herrmann and Stolper, 4 Webster, 5 Graf v. Spec and Beneke 1. c.
- Footnotes
1 Ueber die Einbettung des menschlichen Fies. studiert an einem kleinen Ei der zweiten Woche. Arch. f. Gynaekologie 76.
2 Beobachtungen an jungen menschlichen Eiern. Anat. Hefte. 21. B.
3 Beitrag zum Studium der menschlichen Placentation. Leipzig, Thieme. 1904.
4 Zur Syncytiogenese beim Meerschweinehen. Wien, Hoelder. 1905.
5 Die Placentation beim Menschen. Uebers. von Kolischer. Berlin, O. Coblenz, 1906.
Peters' description of the trophoblast corresponds in all essential features with ours. He found the development, the structure and the lining of the trophoblast processes with syncytium exactly the same as I saw them. He says on page 49: "From the simple cuboidal cells of the central portion of the trophoblast one can successively follow, towards the surface, their transition into the large syncytial formations'
"Those blood lacunae which on their proximal surface carry a layer of ectoblast cells, are almost completely lined by a thin layer of protoplasm in which cell membranes not discernible and in which nuclei are visible, arranged in rows. In transverse sections these nuclei appear spindle shaped, in oblique and longitudinal sections they look flat, often irregularly bent and in their appearance seem identical with the nuclei previously described in the peripheral layer of the ectoblast. This thin protoplasma coat which in the central portion of the blood lacunae resembles a layer of epithelium, continues on the lateral walls of the lacunae, thus enclosing the trophoblast columns."
Peters therefore also finds the blood within the lacunae separated from the trophoblastic excrescences and columns, especially within the arches, by a syncytial lining.
As far as that area of the decidua compacta is concerned, which immediately adjoins the trophoblast (Umlagerungszone of Peters pg. 52), here surrounding the entire ovum, especially on the side of the serotina, greatly dilated maternal blood vessels and a large number of transverse sections through glands are seen,. The uterine mucosa here is not only edematous, but also abundantly infiltrated with blood elements.
Further away from the ovum in Peters' specimen (Plate I) a large endothelial tube is visible from which a number of larger and smaller vessels branch off. These encircle the ovum like meridians the globe. "They communicate with the blood lacunae of the trophoblast near the oyular pole, often only after having first passed through a part of the 'Umlagerungszone' or through intermediate layers lying between it and. the compacta. In other places these vessels after only a short course open into the lacunae at points near the serotina."
As regards the relation of the trophoblast to the surrounding capillaries and their endothelial tubes, Peters' investigations (pg. 59) show that the trophoblastic processes do not bore their way into the endothelial walls as I have described, but that the blood has actively broken into the trophoblast. This condition Peters has depicted in that excellent illustration, Fig. 23, v Plate A, to which I cannot furnish an equal from any one of my sections. I have only been able to observe, as stated above, that at first the ovule lies in a premenstrual extravasate of blood in the mucosa, that next the trophoblast grows, by means of syncytial cells, which it sends out into the surrounding tissue, corrodes the next capillary and thus brings one capillary after the other in communication with the blood lacunae. Since the great vascularity, however, in the neighborhood of my ovum possibly is abnormal, I am willing to admit that most probably Peters' histologic findings are more correct and therefore his deductions more reliable. It must be added, however, that this difference in the findings is of little importance, since I could show exactly like Peters a point of much greater importance that a communication exists between the blood spaces within the trophoblastic arches and those lying farther away. We established in this way the fact, that at this early time intervillous blood spaces exist in a rudimentary and fully developed state.
Mention must be made of a rather important finding by Peters on an ovum 3x5 mm. large (i. e., much larger than my ovum), obtained from a woman who died of phosphorus poisoning. "With due regard to the fact that this was a case of phosphorus poisoning he states that in this ovum in which the trophoblast layer was already reduced to the double layered chorion epithelium (Langhans' cells plus syncytium) and which with its villi was embedded in a lake of blood, the intervillous space by means of a continuous layer of fibrin which completely surrounded the ovum, was separated from the compacta, pathologically changed by a suffusion of blood. Whether this fibrin layer by comparison with undoubtedly normal specimens can be regarded as the primary stage of the fibrin layer of Nitabuch is a question which cannot be answered."
I must mention that also, in my ovum, in some sections, especially near the border of the greatly dilated and open blood spaces which surround the ovum like a shell, such strips of fibrin are visible. I should like to refrain, however, from positively defining their significance.
The following points which have been clearly established by the descriptions given above must be emphasized : The formation of the blood lucanae in the trophoblast does not stand in any direct relation to the destruction and dissolution of the glands, a point which also has been made by Peters, (pgs. 75 & 76). Nowhere is syncytium formed from glandular epithelium.
I cannot agree with Pfannenstiel, who, also in all essential points in accord with Peters, holds different views in certain questions, e. g., concerning the mucosa surrounding the ovum. His observations are made on a comparatively too old an ovum, being almost two weeks old. He asserts (pg. 242) that in his belief the blood lacunae in the trophoblast are new formed capillaries of the decidua, whose walls either the endothelium or the surrounding connective tissue had transformed into syncytium. In none of my sections could I find any support of this view.
Like Peters, I found that the partitioned lacunae at the border, for the very reason that they are lying between the trophoblast columns and in fact are formed by them, are lined with a layer of syncytium which ceases where the ends of the trophoblastic processes peripherally reach either the framework of the mucosa or the walls of the open blood vessels. It seems questionable to me whether these lacunae, although of maternal origin, can be called new formed capillaries of the decidua. This is, however, a point of minor consequence. Of much more importance is the fact, that the syncytial coat of these lacunae, as has been demonstrated above, derives its existence from the Eianlage, i. e., from the ectoblast.
Most noteworthy findings have been made by Rossi Doria, who examined an ovum dating from the beginning of the second week of pregnancy. Aside from many observations which are fully in accord with those made by Peters and myself, his findings concerning the trophoblastic capsule are especially interesting.
He also claims that the fertilized ovum penetrates the extremely congested mucosa of the premenstrual stage and enters a space filled with extravasated blood. "The chorionic trophoblast excrescences from the ectoderm proliferate through the blood until they reach the surrounding connective tissue. They spread out with it and cause certain changes." These consist in a dilation and rupture of capillaries and in the formation of new extravasates in which the trophoblast forms new and longer processes. A formation of new blood vessels which has been claimed by Pfannenstiel has not been observed by Rossi Doria.
According to Rossi Doria, "the trophoblast corrodes the vessel walls and penetrates them with the syncytium. In defense the maternal tissue protects itself against the invasion of the trophoblast by means of a barrier of decidual cells (Umlagerungszone). In this manner both the fetal trophoblastic and the maternal capsules are formed."
This quotation alone proves sufficiently the great similarity between. Rossi Doria's and my descriptions, yet it may not be amiss to also point out the harmony of our views concerning the formation and lining of the trophoblastic lacunae. I will cite verbatim his description (pg. 503) since my observations are identical. "The syncytium breaks into the decidual coat especially into the perivascular spaces and beneath the endothelium as well as into the lumen of the blood vessels. All the giant cells which have been found by some observers in the decidua, in this stage of development of the ovum, are to be considered cells derived from the syncytium. (Compare my identical findings in Fig. 4). They have become separated from a pedicle at first existing and then even in a series of sections show the character of isolated cells. Often, however, they remain attached to the syncytium from which they originate, and then only by mistake can be pronounced giant cells."
According to Marchand (pg. 262) the developing ovum reacts upon the surrounding uterine inucosa like a malignant growth, it "eats its way" into the mucosa as Graf v. Spec has demonstrated for the earliest stage of the ovum of the guinea pig. Other claims of Marchand need not be considered here since the ova described by him are much older, two of them being in quite a defective condition.
The ovum described by Friolet and estimated to be from three to four weeks old also seems of limited value in a consideration of the very early stage. He agrees in all main points with Peters.
Herrmann and Stolper have made exhaustive researches concerning the ovum of the guinea pig and have arrived at the following conclusions: "1. In the guinea pig there exists but one kind of syncytium and this is positively fetal, having developed from the Anlage of the placenta. 2. There exists definite relations between the syncytium and maternal vessels ; and, 3. The villus of the placenta of the guinea pig in a certain stage of development, exactly like in the human placenta, shows the characteristic double layer of epithelial cover." Thus the similarity between mine and their findings is obvious.
Concerning the very meritorious work of Webster, it must be stated that in the main it presents a clear survey of all the findings which have been made in all the various months of pregnancy, but does not deal with any personal investigation of a new young ovum.
Beneke, who has examined a considerably older ovum (4.2x 2.2x1.2 mm.) with an embryo 1.86 mm. long, comes to deductions which are identical with Peters' and those of mine. In the main he confirms the views of Van Heukelom, Peters, Marchand and others concerning the structure of the trophoblast. He also considers the syncytial giant cells as originating from fetal ectoblast. He did not succeed in differentiating a Symplasma glandulare, conjunctivum and cndothclialc from fetal syncytium as has been done by Bonnet. The synctium displaces the endothelial cells of the dilated decidual blood vessels and the epithelium of the glands. A detailed report of his findings is still outstanding.
V. The Syncytium
In the previous chapters, in describing the ectoblast and trophoblast, mention has so frequently been made of the syncytium that no doubt can be left concerning my own views of its origin.
Since the opinions of most prominent investigators- are still at variance on this point, I shall once more consider the origin and function of the syncytium and shall quote disparaging views of others.
In accordance with Peters, my specimens (Figs. 16 and 17) show that the syncytium forms the external cell layer of the ectoblast and that it is first noticed in this situation. We have further observed that when the inner layer of cells (Langhans' cells) begin to send out small excrescences (Fig. 17 kn.) or longer processes, (Figs. 16 and 17 tr) these are covered with syncytium which closely follows all the larger and largest trophoblast columns and with them reaches the connective tissue of the ovular chamber.
In this manner the syncytium separates all the proliferations of the trophoblast from the surrounding blood.
Next it becomes the duty of the syncytium to connect the ends of the trophoblastic processes with the adjoining tissue, to corrode the surrounding vessels, to unravel their walls and finally to open up more and more blood spaces from which the growing ovum may derive its nutrition.
In all specimens thus the syncytium can be followed from within outwards, from the ectoblast towards the ends of the trophoblastic processes, but not in the reverse direction. It can be observed at the ends of the short trophoblastic excrescences, which have not as yet become adherent, in form of those well known processes which vary in shape but as a rule are knoblike. In studying these pictures and comparing them with others it seems impossible to come to any .other conclusion than that the syncytium is solely of fetal origin and that it forms the external cell layer of the ectoblast providing for the growth and nutrition of the ovum.
The manner also in which the syncytial cells corrode, weaken and dissolve the vessel walls, leads us to but one conclusion, viz : that they must be fetal tissue originating in the Eianlage. One can see how they leave the ovum and advance into the tissue but never take the opposite direction. If the latter were true, a far larger number of syncytial cells would be found in the immediate neighborhood of the vessels of the ovular envelope. The fact that all trophoblastic processes, short and long, carry syncytium and that the arches of the trophoblastic lacunae are almost completely lined with a syncytial coat can hardly be brought into harmony with Pfannenstiel's claim, that the vessel endothelium is transformed into syncytium and that starting from here the syncytium gradually proceeds toward the ovum.
Peters, with whom I agree, expresses the following precise views concerning the genesis, the early appearance, and the location of the syncytium (pg. 87.) : "We occasionally, though rarely find within the trophblast, blood lacunae which as yet are not lined with syncytium. Otherwise, however, the syncytium is found distributed over the entire surface of the ovum, i. e., in all sections of the complete series here and there we find bands and masses of syncytial protoplasm varying in size, which either lie flat on the trophoblast or are connected with it by a irregular network of protoplasm or lie free in the blood lacunae or at times push forward toward the Umlagerungszone." On these facts Peters declares the syncytium to be a tissue of fetal origin and my specimens have forced me to the same conclusion.
This seems to settle the question whether the syncytium could possibly originate from uterine epithelium or decidual tissue. Peters has advanced so many and convincing arguments in opposing this view that I feel unable to add new ones.
The following are some of the points in which my views have changed as a result of the study of this youngest ovum and are now at variance with views formerly expressed : The origin of the Langhans' cells, the decidua of uterine epithelium in the neighborhood of the ovum (already corrected on a previous occasion), the origin of the intervillous spaces, and a few others.
A further advance of our knowledge of this problem depends upon the discovery of more very young human ova in situ, coming if possible from patients who have died suddenly but not as suicides. These specimens must be carefully preserved, painstakingly examined and the microscopic pictures reproduced in illustrations which are true to nature.
Explanation of Figures
Plate I
Fig. 1. The pregnant uterus split up its anterior wall. The light spot marked "ovum" denotes the site of embedding of the ovum. o. i.= Internal Os.
Fig. 2. Three microscopic sections demonstrating the mucous membrane elevation (h), in which the ovum lies, g line of separation of mucosa and musctilaris. 2a Section 5; 2b~ Section 80; 2c = Section 160. (Natural size.)
Fig. 1. The pregnant uterus split up its anterior wall. The light spot marked "ovum" denotes the site of embedding of the ovum. o. i.= Internal Os.
Fig. 2. Three microscopic sections demonstrating the mucous membrane elevation (h), in which the ovum lies, g line of separation of mucosa and musctilaris. 2a Section 5; 2b~ Section 80; 2c = Section 160. (Natural size.)
Plate II
Fig. 3. Section 4. Outer border of the mucous membrane elevation, e = surface epithelium, v = decidua vera. d Dilated and folded gland, showing beautifully preserved epithelium, c Capillaries. F Mucous membrane furrow. Obj. A A. Oc. 3.
Fig. 4. Section 10. fi = Fibrin cover, e = Rests of surface epithelium, c = Confluent blood vessels. F = Furrow, tr = Trophoblast processes, sy = Syncytial cells. Obj. A A. Oc. 3.
Plate III
Fig. 5. Section 15. Obj. AA. Oc. 12.
fi = Fibrin cover.
w = Rests of cubodial epithelium on the fibrin cover.
e = Underlying surface epithelium (?).
e.s. = The same depressed, simulating a gland opening. (See Text!).
c = Confluent blood spaces. Fig. 6. Section 19. Obj. A A. Comp. Oc. 4.
fi = Fibrin cover.
e.s. Trace of depression as seen more plainly in Fig. 5. (Section 15).
c = Confluent blood spaces.
tr = Trophoblast processes.
F Mucous membrane furrow. Red blood corpuscles between the depression, (e. s.) and fibrin cover.
Plate IV
Fig. 7. Section 22. .Obj. A A. Oc. 3.
fi = Fibrin cover.
e From the edges surface epithelium ( ?) is seen passing beneath the fibrin cover. Possibly syncytium.
d.v.= Decidua vera.
c = Confluent blood vessels.
tr = Trophoblast processes.
F = Mucous membrane furrow.
"ovum" = The Fianlage, laterally cut, is seen for the first time. Fig. 8. Section 27. Obj. A A. Comp. Oc. 4."
fi = Fibrin cover. To the right arranged in folds.
d.v.^ Decidua vera.
c Confluent blood vessels.
F = Mucous membrane furrow.
dr = Glands.
tr Several trophoblast processes have become anchored in the periphery of the mucous membrane.
sy = A plug with knob-like syncytial processes.
"ovum".= Eianlage becomes more distinct.
Plate V
Fig. 9. Section 26-28. Zeiss Obj. A A. Oc. 3.
fi = Fibrin cover. To the right arranged in folds. e = Border epithelium (?), passing from surface under fibrin cover. Probably a band of syncytium passing from trophoblast (tr). tr = Trophoblast processes.
Plate VI. Fig. 10. The left half of Fig. 9 highly magnified. Obj. Zeiss. Aprochr. 4.0 mm. Oc. 6.
fi = Fibrin cover.
e = Border epithelium.
tr = The trophoblast processes are connected with the syncytial cells, which might be mistaken for surface epithelium. (Compare Peters' Plate V. Fig. 12 and 13.)
Plate VII
Fig. 11. Section 30, Obj. AA. Oc. 8. The middle part of the Section was purposely omitted.
fi = Fibrin cover, symmetrical to the left, to the right many folds present, as in a corpus luteum. tr = Trophoblast processes terminating in a sy =syncytial club shaped ending.
e = Epithelial rests (?). Probably a band of syncytium coming from the trophoblast (tr).
Fig. 12. Section 32. Obj. Apochr. 4,0 mm. Oc. 3. tr = Trophoblast processes. sy = Syncytium.
Fig. 13. Section 39. Apochr. Obj. 4,0 mm. Oc. 3. fi Fibrin cover.
sy Syncytial bands, terminating to the right in a club-shaped mass of cells, tr = Trophoblast covered with (sy) syncytium.
Plate VIII
Fig. 14. Section 37. Obj. A A. Oc. 3.
fi Fibrin cover.
e = Rests of surface epithelium (?).
c = Confluent blood vessels.
F = Mucous membrane furrow.
dr = Glands. The lateral ones (to the left and above) open into the cavum uteri, to the right and below, into the furrow. The middle gland (m) divides into two branches.
The right branch approaches the ovular chamber, but does not open into it.
tr = Trophoblast processes.
sy = Mass of syncytium.
Plate IX
Fig. 15. Section 40. Obj. A A. Oc. 8.
fi = The club-like end of the fibrin cover showing the folded arrangement as in a corpus luteum.
tr = The arch-like arranged trophoblast can be traced to the epithelial-like bands beneath the club-like end of the. fibrin cover. Question, whether epithelial rest or not.
Fig. 16. Section 47. Obj. A A. Oc. 8.
fi = Fibrin cover partly undergoing organization.
ei Eianlage.
ekt = Ectoderm.
tr = Trophoblast processes.
sy Syncytial buds. Fig. 17. Section 60. "Obj. A A. Oc. 8. Lettering as in Fig. 16.
k Trophoblast buds with a syncytial covering. (See Fig. 16. under high magnification).
Plate X
Fig. 18. Section 63. Obj. D. Oc. 3.
fi.o.= Fibrin covering undergoing organization, ei = Eianlage. ekt and EMi~= Ectoderm, tr = Trophoblast processes.
a = Eianlage lying with its broad surface to the inner wall of the summit of the ovum.
Plate XI
Fig. 19. Section 69. Obj. AA. Oc. 3.
Kn^ The fibrin cover presents itself in its right process as a small structureless elevation.
Fig. 20. Fig. 21.
Plate XII
Fig. 22.
Plate XIII
Fig. 23.
Plate XIV
Fig. 24.
Plate XV
Fig. 25.
Plate XVI
Fig. 26.
Fig. 27.
Fig. 28.
Section 75. Obj. AA. Oc. 3.
Kn The knob-like projection again becomes longer and lies upon the organized fibrin.
s.b. = A cloddy band covering same. Section 80. Obj. A A. Oc. 4.
fi = The structureless fibrin cover again becomes longer and is similar to sections 10-25.
s.b. = A cloddy band lying upon same. Eianlage with numerous trophoblast processes. (Sketched).
Section 92. Obj. AA. Oc. 3.
fi = The fibrin cover partly covered by cloddy band, (s. b.) again becomes longer and lies upon the ovular summit.
F = Mucous membrane furrow.
c. ci, cs= Confluent dilated blood spaces.
dr ' Elongated glands surround the ovum.
tr = The trophoblast processes are anchored in the border of the ovular chamber by means of the syncytium.
Section 94. Obj. AA. Oc. 6. f
fi = The fibrin cover with its short cloddy band (s. b.), has again become somewhat longer and lies closely applied to the border tissue.
F = Mucous membrane furrow.
c, ci, c-= Confluent dilated blood spaces.
dr. dn. dr, = Glands. Those marked dn and drc in the illustration, reach almost to the uterine cavity. They are partly filled with blood and toward the base of the ovular chamber they appear partly displaced and partly dissolved. No gland is seen opening into the ovular chamber.
tr = Several trophoblast processes are anchored to the inner u-;:ll of the ovular chamber.
Section 105. Obj. A A. Oc. 8.
The fibrin cover is no Jonger present.
F = Mucous membrane furrow.
c = Confluent blood spaces.
dr. dn Glands. The one marked dn reaches almost to the ovular chamber.
tr = A number of trophoblast processes anchor themselves to the inner wall of the ovular chamber partly with syncytial offshoots.
Section 142. Obj. AA. Oc. 3.
c = Mucous membrane elevation with innumerable confluent blood spaces.
dr = Four large glands showing a partly tortous course with opening at dr.m.
bl = Blood free in the tissue.
Section 52. Obj. 4,0 mm. Oc. 3.
Ectoderm highly magnified (See Figs. 16, 17 and 18). 1. z. =Langhans' cells on the inside. sy = Syncytial cover on the outside.
Section 60 (See Fig. 17) under low power. Ectoderm under high magnification.
1. z. = Langhans' cells forming trophoblast cells and offshoots. They are covered externally like ectoderm bands in Fig. 26 with syncytium. Obj. 4,00 mm. Oc. 3. Section 90. Obj. 4,0 mm. Oc. 3.
sy = The syncytial cells advance from the trophoblast toward the wall of a transversely cut capiliary (ca) and corrode the vessel wall (en).
Cite this page: Hill, M.A. (2024, April 24) Embryology Book - A Very Young Ovum In Situ. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Book_-_A_Very_Young_Ovum_In_Situ
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G