The printable version is no longer supported and may have rendering errors. Please update your browser bookmarks and please use the default browser print function instead.
| Educational Use Only - Embryology is an educational resource for learning concepts in embryological development, no clinical information is provided and content should not be used for any other purpose.
|
Introduction
There are a variety of prenatal techniques for estimating approximate birth weight that are relevant for preterm, term and prolonged pregnancy. Ultrasound two- and three-dimensional scanning methods are the basis of most current techniques. There are also standard autopsy weight curves that have been developed from second and third trimester fetal and also neonatal autopsy. Low birth weight is accurately defined as a statistical indicator for development. High birthweight definition on the other hand varies in the literature and between countries with a lower cut-off above 4000 gm or 4500 gm.
At birth, infants are generally weighed as soon as possible and may also be monitored during the neonatal period. In Australia, the average birthweight for all babies born: (1991) 3,350 grams, (2004 3,370 grams and (2015)[1] 3,327 grams. Also in 2015 6.5% (19,852) of liveborn babies were of low birthweight.[1]
- Links: ultrasound | DOHAD | maternal diabetes | macrosomia
Some Recent Findings
- New Australian Birthweight Centiles[2] "All singleton births in Australia of 23-42 completed weeks' gestation and with spontaneous onset of labour, 2004-2013. Births initiated by obstetric intervention were excluded to minimise the influence of decisions to deliver small for gestational age babies before term. Current birthweight centile charts probably underestimate the incidence of intra-uterine growth restriction because obstetric interventions for delivering pre-term small for gestational age babies depress the curves at earlier gestational ages. Our curves circumvent this problem by excluding intervention-initiated births; they also incorporate more recent population data. These updated centile curves could facilitate more accurate diagnosis of small for gestational age babies in Australia."
- Fetal brain development in small-for-gestational age (SGA) fetuses and normal controls[3] "Objective To assess whether fetal brain structures routinely measured during the second and third trimester ultrasound scans, particularly the width of the cavum septi pellucidi (CSP), differ between fetuses small for gestational age (SGA), fetuses very small for gestational age (VSGA) and normal controls. Methods In this retrospective study, we examined standard ultrasound measurements of 116 VSGA, 131 SGA fetuses and 136 normal controls including the head circumference (HC), transversal diameter of the cerebellum (TCD), the sizes of the lateral ventricle (LV) and the cisterna magna (CM) from the second and third trimester ultrasound scans extracted from a clinical database. We measured the CSP in these archived ultrasound scans. The HC/CSP, HC/LV, HC/CM and HC/TCD ratios were calculated as relative values independent of the fetal size. Results The HC/CSP ratio differed notably between the controls and each of the other groups (VSGA P = 0.018 and SGA P = 0.017). No notable difference in the HC/CSP ratio between the VSGA and SGA groups could be found (P = 0.960). The HC/LV, HC/CM and HC/TCD ratios were similar in all the three groups. Conclusion Relative to HC, the CSP is larger in VSGA and SGA fetuses than in normal controls. However, there is no notable difference between VSGA and SGA fetuses, which might be an indicator for abnormal brain development in this group."
- Diagnosing Small for Gestational Age during second trimester routine screening: Early sonographic cluesFatihoglu E & Aydin S. (2020). Diagnosing Small for Gestational Age during second trimester routine screening: Early sonographic clues. Taiwan J Obstet Gynecol , 59, 287-292. PMID: 32127152 DOI. "Small for gestational age (SGA) is generally defined as birth weight being at or below the 10th percentile. Children with SGA have a higher risk for complications. There is a need for early predictors, as the accurate diagnosis rate is only 50%. In the current study, we aimed to evaluate diagnostic performance of ultrasound (US)/color Doppler ultrasound (CDUS) parameters (umbilical vein-UV, right portal vein-RPV diameter/flow rate, and portal sinus-PS diameter) examined at 20-22 gestational week as SGA diagnostic factors. CONCLUSION: UV, RPV, and PS diameters can be earlier predictors for SGA diagnosis. Routinely evaluation of these parameters during second trimester screening can increase SGA diagnosis rates and serve for early diagnose."
- Impact of biometric measurement error on identification of small- and large-for-gestational-age fetuses[4] OBJECTIVES: First, to obtain measurement-error models for biometric measurements of fetal abdominal circumference (AC), head circumference (HC) and femur length (FL), and, second, to examine the impact of biometric measurement error on sonographic estimated fetal weight (EFW) and its effect on the prediction of small- (SGA) and large- (LGA) for-gestational-age fetuses with EFW < 10th and > 90th percentile, respectively. CONCLUSIONS: Measurement error in fetal biometry causes substantial error in EFW, resulting in misclassification of SGA and LGA fetuses. The extent to which improvement can be achieved through effective quality assurance remains to be seen but, as a first step, it is important for practitioners to understand how biometric measurement error impacts the prediction of SGA and LGA fetuses."
|
| Older papers
|
| These papers originally appeared in the Some Recent Findings table, but as that list grew in length have now been shuffled down to this collapsible table.
See also the Discussion Page for other references listed by year and References on this current page.
- Associations Between the Features of Gross Placental Morphology and Birthweight[5] "The placenta plays a critical role in regulating fetal growth. Recent studies suggest that there may be sex-specific differences in placental development. The purpose of our study was to evaluate the associations between birthweight and placental morphology in models adjusted for covariates and to assess sex-specific differences in these associations. We analyzed data from the Stillbirth Collaborative Research Network's population-based case-control study conducted between 2006 and 2008, which recruited cases of stillbirth and population-based controls in 5 states. Our analysis was restricted to singleton live births with a placental examination (n = 1229). Characteristics of placental morphology evaluated include thickness, surface area, difference in diameters, shape, and umbilical cord insertion site. We used linear regression to model birthweight as a function of placental morphology and covariates. Surface area had the greatest association with birthweight; a reduction in surface area of 83 cm2, which reflects the interquartile range, is associated with a 260.2-g reduction in birthweight (95% confidence interval, -299.9 to -220.6), after adjustment for other features of placental morphology and covariates. Reduced placental thickness was also associated with lower birthweight. These associations did not differ between males and females. Our results suggest that reduced placental thickness and surface area are independently associated with lower birthweight and that these relationships are not related to sex." placenta
- Relationship between birth weight to placental weight ratio and major congenital anomalies in Japan[6] "Recent studies have indicated that birth weight to placental weight (BW/PW) ratio is related to perinatal outcomes, but the effect of congenital abnormalities on BW/PW ratio remains unclear. We performed this study to elucidate correlations between BW/PW ratio and congenital abnormalities. Subjects were 735 singleton infants born at 34-41 weeks of gestation admitted to our center between 2010 and 2016. Of these, 109 infants (15%) showed major congenital anomalies. Major congenital anomalies and subgroups were diagnosed according to European Surveillance of Congenital Anomalies criteria. The primary outcome was the association between BW/PW ratio and major congenital anomaly, and secondary outcomes were the distribution pattern of BW/PW ratio with major anomalies and by major anomaly subgroups in each categorization (<10th percentile, 10-90th percentile, or >90th percentile) of BW/PW ratio. BW/PW ratio was not associated (P = 0.20) with presence (adjusted mean BWPW ratio = 5.02, 95% confidence interval [CI] 4.87-5.18) or absence (adjusted mean BW/PW ratio = 4.91, 95%CI 4.85-4.97) of major anomalies, after adjusting for gestational age and sex. Proportions of infants with major anomalies according to BW/PW ratio categories were as follows: 12% in <10th percentile, 15% in 10-90th percentile, and 25% in >90th percentile of BW/PW ratio. Among major anomalies of the nervous system, congenital heart defects, and orofacial clefts, BW/PW ratio showed equally distributed trend across the three BW/PW ratio categories, but showed unequally distributed trend for anomalies of the digestive system, other anomalies/syndromes, or chromosomal abnormalities. BW/PW ratio was not associated with major congenital anomaly, and was distributed diffusely according to major anomaly subgroups. Major anomalies may tend to aggregate in the 90th percentile of the BW/PW ratio."
- Association between Vitamin Intake during Pregnancy and Risk of Small for Gestational Age[7] "Pregnancy increases the requirements of certain nutrients, such as vitamins, to provide nutrition for the newborn. The aim was to analyze the association between dietary intake of vitamins during pregnancy and risk of having a small for gestational age (SGA) newborn. A matched case-control study was conducted (518 cases and 518 controls of pregnant women) in Spain. ... A protective association was observed between maternal dietary intake of vitamins A and D and SGA. For vitamin B3 and B6, the observed protective effect was maintained after adjusting for potential confounding factors. For vitamin B9, we found only an effect in quintiles 3 and 4. Protective effect for vitamin B12 was observed in 4th and 5th quintiles. No associations were detected between dietary intake of vitamins B2, E and C intake and SGA." nutrition
- Birthweight and Childhood Cancer: - Preliminary Findings from the International Childhood Cancer Cohort Consortium (I4C)[8] "Evidence relating childhood cancer to high birthweight is derived primarily from registry and case-control studies. We aimed to investigate this association, exploring the potential modifying roles of age at diagnosis and maternal anthropometrics, using prospectively collected data from the International Childhood Cancer Cohort Consortium. We pooled data on infant and parental characteristics and cancer incidence from six geographically and temporally diverse member cohorts [the Avon Longitudinal Study of Parents and Children (UK), the Collaborative Perinatal Project (USA), the [Europe_Statistics#Danish_National_Birth_CohortDanish National Birth Cohort] (Denmark), the Jerusalem Perinatal Study (Israel), the Norwegian Mother and Child Cohort Study (Norway), and the Tasmanian Infant Health Survey (Australia)]. Birthweight metrics included a continuous measure, deciles, and categories (≥4.0 vs. <4.0 kilogram). Childhood cancer (377 cases diagnosed prior to age 15 years) risk was analysed by type (all sites, leukaemia, acute lymphoblastic leukaemia, and non-leukaemia) and age at diagnosis. We estimated hazard ratios (HR) and 95% confidence intervals (CI) from Cox proportional hazards models stratified by cohort. A linear relationship was noted for each kilogram increment in birthweight adjusted for gender and gestational age for all cancers. Similar trends were observed for leukaemia. There were no significant interactions with maternal pre-pregnancy overweight or pregnancy weight gain. Birthweight ≥4.0 kg was associated with non-leukaemia cancer among children diagnosed at age ≥3 years, but not at younger ages. Childhood cancer incidence rises with increasing birthweight. In older children, cancers other than leukaemia are particularly related to high birthweight. Maternal adiposity, currently widespread, was not demonstrated to substantially modify these associations."
- Outcomes of neonates with birth weight⩽500 g: a 20-year experience[9] "Ethical dilemmas continue regarding resuscitation versus comfort care in extremely preterm infants. Counseling parents and making decisions regarding the care of these neonates should be based on reliable, unbiased and representative data drawn from geographically defined populations. ...About a third of neonates admitted to NICU with ⩽500 g BW survived, with 33% of those surviving, demonstrating age-appropriate development at a 24-month follow-up visit."
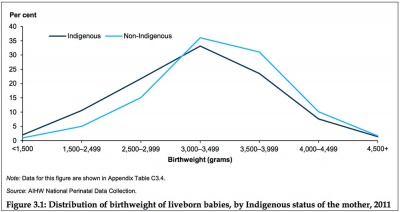
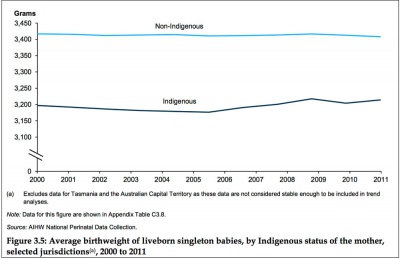
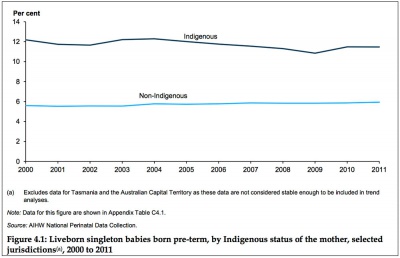
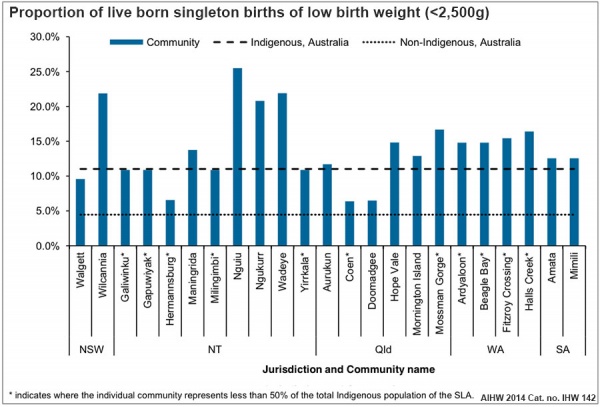
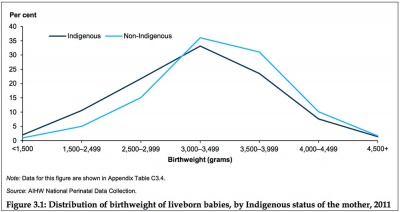
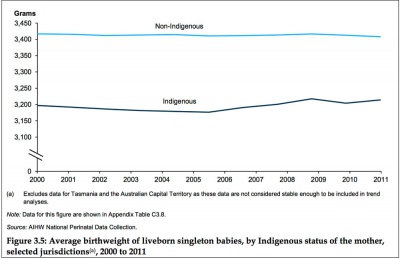
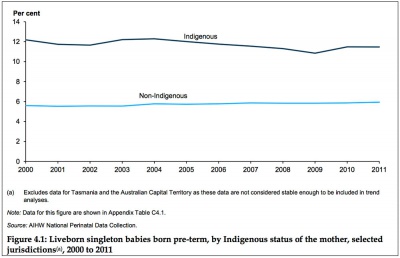
- Australian Institute of Health and Welfare - Birthweight of babies born to Indigenous mothers[10] "Birthweight of babies born to Indigenous mothers provides an overview of the birthweight of babies born to Indigenous mothers, including recent trends and information on factors associated with birthweight variation. According to data from the National Perinatal Data Collection, 3.9% of all births in 2011 were to Indigenous mothers. Excluding multiple births, 11.2% of liveborn singleton babies born to Indigenous mothers were of low birthweight—2.5 times the rate for non-Indigenous mothers (4.6%). Between 2000 and 2011, there was a statistically significant decline in the low birthweight rate among Indigenous mothers, and the gap in birthweight between babies born to Indigenous and non-Indigenous mothers declined significantly over this period."
- Birthweight percentiles by gestational age for births following assisted reproductive technology in Australia and New Zealand, 2002-2010[11] "The comparison of birthweight percentile charts for ART births and general population births provide evidence that the proportion of SGA births following ART treatment was comparable to the general population for SET fresh cycles and significantly lower for thaw cycles. Both fresh and thaw cycles showed better outcomes for singleton births following SET compared with DET. Policies to promote single embryo transfer should be considered in order to minimize the adverse perinatal outcomes associated with ART treatment." Australian Statistics | Assisted Reproductive Technology
- Searching for the Definition of Macrosomia through an Outcome-Based Approach[12] "Macrosomia has been defined in various ways by obstetricians and researchers. The purpose of the present study was to search for a definition of macrosomia through an outcome-based approach. In a study of 30,831,694 singleton term live births and 38,053 stillbirths in the U.S. Linked Birth-Infant Death Cohort datasets (1995-2004), we compared the occurrence of stillbirth, neonatal death, and 5-min Apgar score less than four in subgroups of birthweight (4000-4099 g, 4100-4199 g, 4200-4299 g, 4300-4399 g, 4400-4499 g, 4500-4999 g vs. reference group 3500-4000 g) and birthweight percentile for gestational age (90th-94th percentile, 95th-96th, and ≥97th percentile, vs. reference group 75th-90th percentile). There was no significant increase in adverse perinatal outcomes until birthweight exceeded the 97th percentile. A birthweight greater than 4500 g in Whites, or 4300 g in Blacks and Hispanics regardless of gestational age is the optimal threshold to define macrosomia. A birthweight greater than the 97th percentile for a given gestational age, irrespective of race is also reasonable to define macrosomia. The former may be more clinically useful and simpler to apply." macrosomia
- Ten-Year Review of Major Birth Defects in VLBW Infants[13] "Birth defects (BDs) are an important cause of infant mortality and disproportionately occur among low birth weight infants. We determined the prevalence of BDs in a cohort of very low birth weight (VLBW) infants cared for at the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network (NRN) centers over a 10-year period and examined the relationship between anomalies, neonatal outcomes, and surgical care. ...Chromosomal and cardiovascular anomalies were most frequent with each occurring in 20% of affected infants. Mortality was higher among infants with BDs and varied by diagnosis. Among those surviving >3 days, more infants with BDs underwent major surgery (48% vs 13%, P < .001). Prevalence of BDs increased during the 10 years studied. BDs remain an important cause of neonatal morbidity and mortality among VLBW infants."
|
Birth Weight Classifications
The primary causes of VLBW are premature birth (born <37 weeks gestation, and often <30 weeks) and intrauterine growth restriction (IUGR), usually due to problems with placenta, maternal health, or to birth defects. Many VLBW babies with IUGR are preterm and thus are both physically small and physiologically immature.
| Human Birth Weight Classifications
|
no colour
|
| Birth weight (grams)
|
less 500
|
500 – 999
|
1,000 – 1,499
|
1,500 – 1,999
|
2,000 – 2,499
|
2,500 – 2,999
|
3,000 – 3,499
|
3,500 – 3,999
|
4,000 – 4,499
|
4,500 – 4,999
|
5,000 or more
|
| Classification
|
Extremely Low Birth Weight
|
Very Low Birth Weight
|
Low Birth Weight
|
Normal Birth Weight
|
High Birth Weight
|
Extremely Low Birth Weight
- Less than 500 grams (1 lb 1 oz or less)
- 500 – 999 grams (1 lb 2 oz – 2 lb 3 oz)
Very Low Birth Weight
- 1,000 – 1,499 grams (2 lb 4 oz – 3 lb 4 oz)
Low Birth Weight
- 1,500–1,999 grams (3 lb 5 oz – 4 lb 6 oz)
- 2,000–2,499 grams (4 lb 7 oz – 5 lb 8 oz)
Normal Birth Weight
- 2,500–2,999 grams (5 lb 9 oz – 6 lb 9 oz)
- 3,000–3,499 grams (6 lb 10 oz – 7 lb 11 oz)
- 3,500–3,999 grams (7 lb 12 oz – 8 lb 13 oz)
High Birth Weight
- 4,000–4,499 grams (8 lb 14 oz – 9 lb 14 oz)
- 4,500–4,999 grams (9 lb 15 oz – 11 lb 0 oz)
- 5,000 grams or more (11 lb 1 oz or more)
- see also macrosomia
Weight Conversions
| Extremely Low Birth Weight
|
Very Low Birth Weight
|
Low Birth Weight
|
Normal Birth Weight
|
High Birth Weight (macrosomia)
|
- Less than 500 grams (1 lb 1 oz or less)
- 500 – 999 grams (1 lb 2 oz – 2 lb 3 oz)
|
- 1,000 – 1,499 grams (2 lb 4 oz – 3 lb 4 oz)
|
- 1,500–1,999 grams (3 lb 5 oz – 4 lb 6 oz)
- 2,000–2,499 grams (4 lb 7 oz – 5 lb 8 oz)
|
- 2,500–2,999 grams (5 lb 9 oz – 6 lb 9 oz)
- 3,000–3,499 grams (6 lb 10 oz – 7 lb 11 oz)
- 3,500–3,999 grams (7 lb 12 oz – 8 lb 13 oz)
|
- 4,000–4,499 grams (8 lb 14 oz – 9 lb 14 oz)
- 4,500–4,999 grams (9 lb 15 oz – 11 lb 0 oz)
- 5,000 grams or more (11 lb 1 oz or more)
|
No Background Version
Human Birth Weight Classifications
| Birth weight (grams)
|
less 500
|
500 – 999
|
1,000 – 1,499
|
1,500 – 1,999
|
2,000 – 2,499
|
2,500 – 2,999
|
3,000 – 3,499
|
3,500 – 3,999
|
4,000 – 4,499
|
4,500 – 4,999
|
5,000 or more
|
| Classification
|
Extremely Low Birth Weight
|
Very Low Birth Weight
|
Low Birth Weight
|
Normal Birth Weight
|
High Birth Weight
|
Small for Gestational Age
Small for gestational age (SGA) is a term used for infants as having a birth weight more than 2 standard deviations (SD) below the mean or less than the 10th percentile for the gestational age (GA). WHO birthweight definitions are low birthweight as less than 2,500 grams, very low birthweight is less than 1,500 grams and extremely low birthweight: less than 1,000 grams. Growth restriction can be symmetrical (slow development with limited brain growth) or asymmetrical (head circumference and length are preserved and brain growth is relatively spared).
- Symmetric SGA (Weight, head circumference and length all below the 10th percentile) can be due to chromosomal abnormalities, intrauterine infection, severe placental insufficiency and or a constitutionally small infant.
- Asymmetric SGA (Weight below the 10th percentile) can be due to interference with placental function and or interference with maternal health in 3rd trimester.
There are a large number of known relationships between low birth weight and both maternal and fatal abnormalities, a few examples are shown below.
Z-score
The birth weight Z-score is a predictor of adverse neonatal outcome in severe placental insufficiencies.[14] For an individual birth weight, a z-score of -1 is one standard deviation below the mean birth weight of the cohort.
The Z-score classification system can be used to compare a child or a group of children to the reference population.
The Z-score (SD-score) = (observed value - median value of the reference population) / standard deviation value of reference population.
- Z-score scale is linear - therefore a fixed interval of Z-scores has a fixed height difference in cm, or weight difference in kg, for all children of the same age.
- Z-scores are sex-independent - allows evaluation of children's growth status by combining sex and age groups.
- Z-scores allow statistical calculations - such as means, standard deviations, and standard error to classify a population's growth status.
The Z-score classification system can also be used for population-based assessments, for example to monitor nutritional status malnutrition, health and within nutrition centers.
The z-score differences (Zdiff) uses standard deviation scores to analyze changes in growth for a particular observation period.
- Links:WHO
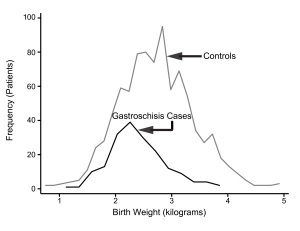
Fetal Gastroschisis
Gastroschisis Birth Weight Graph
Gastroschisis patients are commonly small for gestational age (SGA, birth weight < 10th centile). Frequency line graphs of the birth weight distribution.[15]
The abnormality is usually situated to the right of the umbilicus and abdominal contents, mainly gastrointestinal, are found outside the anterior body wall. Can occur in isolation and also in association with other gastrointestinal anomalies (intestinal atresia, perforation, necrosis or volvulus). Defects in other organ systems have been reported in up to 35% of children.
Maternal Elevated Testosterone
Maternal elevated testosterone levels is associated with low birth weight in humans. Hyperandrogenism associated with polycystic ovarian syndrome (PCOS) and pre-eclampsia have a higher prevalence of small-for-gestational age newborns. A rat model study suggests that maternal testosterone does not cross the placenta, to directly suppress fetal growth, but affects nutrient delivery to the fetus by down-regulating specific amino acid transporter activity.[16]
High Altitude
Altitude affects growth patterns measured in a a recent Peruvian study of 63,620 healthy infants born at low (150 m) and high (3000-4400 m) altitude were compared.[17] They found that in the third trimester "Mean and median birth weight differences between those born at low and high altitudes reached statistical significance after 35 and 33 weeks, respectively."
Canada
Definition: Live births with a birth weight of 4,500 grams or more, expressed as a percentage of all live births with known birth weight.
High birth weight can result in complications for the infant and mother during birth and may be associated with an increased risk of diabetes.
- Links: Canada Statistics | Statistics Canada, Vital Statistics, Birth Database.
Australia - Indigenous
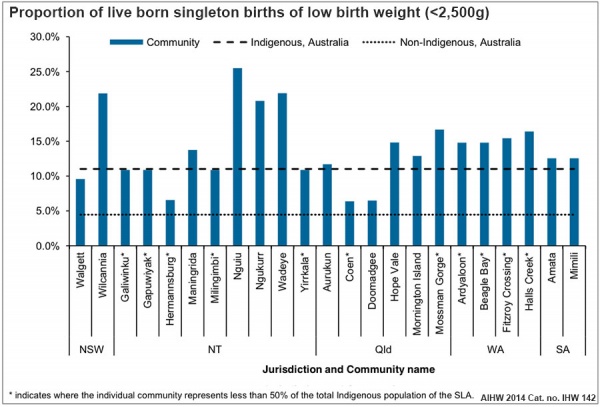
Australian low birth weight (2008–2009)[18]
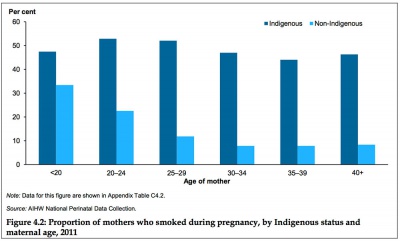
Data in graphs below from AIHW 2014 Report, Birthweight of babies born to Indigenous mothers.[10]
|
|
| Birthweight distribution
|
Average Birthweight (2000-2011)
|
|
|
| Preterm Birth
|
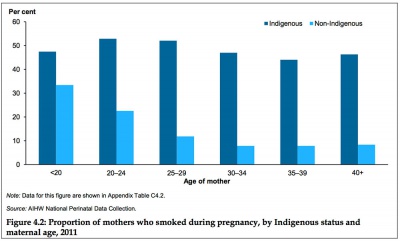
Smoking in Pregnancy
|
- Links: Australian Statistics | Preterm Birth | SmokingBirth weight reference percentiles for Chinese===
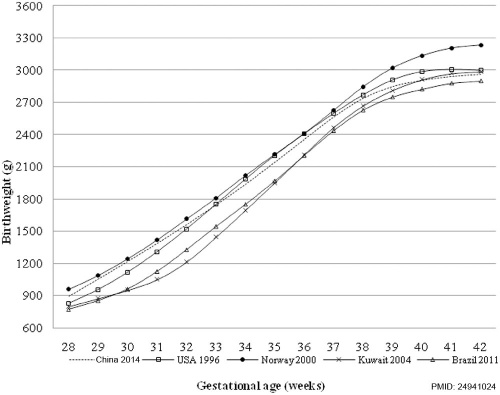
China
Birth weight reference percentiles for Chinese[12] "There have been moderate increases in birth weight percentiles for Chinese infants of both sexes and most gestational ages since 1980s, suggesting the importance of utilizing an updated national reference for both clinical and research purposes."
- Links: China Statistics
References
- ↑ 1.0 1.1 Australian Institute of Health and Welfare 2017. Australia’s mothers and babies 2015—in brief. Perinatal statistics series no. 33. Cat no. PER 91. Canberra: AIHW.
- ↑ Joseph FA, Hyett JA, Schluter PJ, McLennan A, Gordon A, Chambers GM, Hilder L, Choi SK & de Vries B. (2020). New Australian birthweight centiles. Med. J. Aust. , , . PMID: 32608051 DOI.
- ↑ Jacob E, Braun J, Oelmeier K, Köster HA, Möllers M, Falkenberg M, Klockenbusch W, Schmitz R & Hammer K. (2020). Fetal brain development in small-for-gestational age (SGA) fetuses and normal controls. J Perinat Med , , . PMID: 32126016 DOI.
- ↑ Wright D, Wright A, Smith E & Nicolaides KH. (2020). Impact of biometric measurement error on identification of small- and large-for-gestational-age fetuses. Ultrasound Obstet Gynecol , 55, 170-176. PMID: 31682299 DOI.
- ↑ Freedman AA, Hogue CJ, Marsit CJ, Rajakumar A, Smith AK, Goldenberg RL, Dudley DJ, Saade GR, Silver RM, Gibbins KJ, Stoll BJ, Bukowski R & Drews-Botsch C. (2019). Associations Between the Features of Gross Placental Morphology and Birthweight. Pediatr. Dev. Pathol. , 22, 194-204. PMID: 30012074 DOI.
- ↑ Takemoto R, Anami A & Koga H. (2018). Relationship between birth weight to placental weight ratio and major congenital anomalies in Japan. PLoS ONE , 13, e0206002. PMID: 30346975 DOI.
- ↑ Salcedo-Bellido I, Martínez-Galiano JM, Olmedo-Requena R, Mozas-Moreno J, Bueno-Cavanillas A, Jimenez-Moleon JJ & Delgado-Rodríguez M. (2017). Association between Vitamin Intake during Pregnancy and Risk of Small for Gestational Age. Nutrients , 9, . PMID: 29168736 DOI.
- ↑ Paltiel O, Tikellis G, Linet M, Golding J, Lemeshow S, Phillips G, Lamb K, Stoltenberg C, Håberg SE, Strøm M, Granstrøm C, Northstone K, Klebanoff M, Ponsonby AL, Milne E, Pedersen M, Kogevinas M, Ha E & Dwyer T. (2015). Birthweight and Childhood Cancer: Preliminary Findings from the International Childhood Cancer Cohort Consortium (I4C). Paediatr Perinat Epidemiol , 29, 335-45. PMID: 25989709 DOI.
- ↑ Upadhyay K, Pourcyrous M, Dhanireddy R & Talati AJ. (2015). Outcomes of neonates with birth weight⩽500 g: a 20-year experience. J Perinatol , 35, 768-72. PMID: 25950920 DOI.
- ↑ 10.0 10.1 AIHW 2014. Birthweight of babies born to Indigenous mothers. Cat. no. IHW 138. Canberra: AIHW. Viewed 5 August 2014 http://www.aihw.gov.au/publication-detail/?id=60129548202
- ↑ Li Z, Wang YA, Ledger W & Sullivan EA. (2014). Birthweight percentiles by gestational age for births following assisted reproductive technology in Australia and New Zealand, 2002-2010. Hum. Reprod. , 29, 1787-800. PMID: 24908671 DOI.
- ↑ 12.0 12.1 Ye J, Zhang L, Chen Y, Fang F, Luo Z & Zhang J. (2014). Searching for the definition of macrosomia through an outcome-based approach. PLoS ONE , 9, e100192. PMID: 24941024 DOI.
- ↑ Adams-Chapman I, Hansen NI, Shankaran S, Bell EF, Boghossian NS, Murray JC, Laptook AR, Walsh MC, Carlo WA, Sánchez PJ, Van Meurs KP, Das A, Hale EC, Newman NS, Ball MB, Higgins RD & Stoll BJ. (2013). Ten-year review of major birth defects in VLBW infants. Pediatrics , 132, 49-61. PMID: 23733791 DOI.
- ↑ da Silva FC, de Sá RA, de Carvalho PR & Lopes LM. (2007). Doppler and birth weight Z score: predictors for adverse neonatal outcome in severe fetal compromise. Cardiovasc Ultrasound , 5, 15. PMID: 17374167 DOI.
- ↑ Payne NR, Simonton SC, Olsen S, Arnesen MA & Pfleghaar KM. (2011). Growth restriction in gastroschisis: quantification of its severity and exploration of a placental cause. BMC Pediatr , 11, 90. PMID: 22004141 DOI.
- ↑ Sathishkumar K, Elkins R, Chinnathambi V, Gao H, Hankins GD & Yallampalli C. (2011). Prenatal testosterone-induced fetal growth restriction is associated with down-regulation of rat placental amino acid transport. Reprod. Biol. Endocrinol. , 9, 110. PMID: 21812961 DOI.
- ↑ Gonzales GF & Tapia V. (2009). Birth weight charts for gestational age in 63,620 healthy infants born in Peruvian public hospitals at low and at high altitude. Acta Paediatr. , 98, 454-8. PMID: 19038011 DOI.
- ↑ AIHW 2014. Health indicators for Remote Service Delivery communities: a summary report. Cat. no. IHW 142. Canberra: AIHW. Viewed 5 November 2014 http://www.aihw.gov.au/publication-detail/?id=60129548650.
Reviews
Articles
Hemming K, Hutton JL & Bonellie S. (2009). A comparison of customized and population-based birth-weight standards: the influence of gestational age. Eur. J. Obstet. Gynecol. Reprod. Biol. , 146, 41-5. PMID: 19581044 DOI.
Search Pubmed
Search Pubmed: Low Birth Weight | small for gestational age
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
| Birth Terms
|
- amniotomy - birth medical procedure thought to speed labor, where the amniotic sac is artificially ruptured using a tool (amniohook).
- birth - (parturition, partus, childbirth, labour, delivery). expulsion of the foetus from the uterus. (More? birth)
- Bishop score - (Bishop's score) A clinical test prior to birth named after the obstetrician/gynaecologist Edward H. Bishop (1913-1995) who published a 1964 paper "Pelvic Scoring For Elective Induction". (More? PMID 14199536)
- breech - fetal buttocks presented first and can also occur in different forms depending on presentation (complete breech, frank breech, footing breech, knee breech). (More? historic image)
- decidual activation - increased uterine proteolysis and extracellular matrix degradation.
- dilatation - opening of the cervix in preparation for birth (expressed in centimetres).
- effacement - shortening or thinning of the cervix, in preparation for birth.
- early cord clamping - placental cord clamping carried out in the first 60 seconds after birth.
- forceps - mechanical "plier-like" tool used on fetal head to aid birth.
- induction of labour - clinical procedure where labour starts artificially by using a membrane sweep, pessary or hormone drip.
- instrumental birth - birth process where the use of clinical instruments is required.
- labor - the maternal physiological process of birth. (More? birth)
- macrosomia - clinical description for a fetus that is too large, condition increases steadily with advancing gestational age and defined by a variety of birthweights. In pregnant women anywhere between 2 - 15% have birth weights of greater than 4000 grams (4 Kg, 8 lb 13 oz). (More? macrosomia)
- membrane rupture - breaking of the amniotic membrane and release of amniotic fluid (water breaking).
- morbidity - (Latin, morbidus = "sick" or "unhealthy") refers to a diseased state, disability, or poor health due to any cause.
- necrotising enterocolitis - clinical condition mainly seen in preterm infants, where portions of the bowel undergo necrosis.
- neonatal - the early postnatal period relating to the birth, it includes the period up to 4 weeks after birth.
- obstetric fistula - abnormal connection between the vagina and rectum or bladder caused by a prolonged obstructed labor.
- perinatal - the early postnatal period relating to the birth, statistically it includes the period up to 7 days after birth.
- presentation - how the fetus is situated in the uterus.
- presenting part - part of fetus body that is closest to the cervix.
- second stage of labour - passage of the baby through the birth canal into the outside world.
- tachycardia - rapid fetal heart rate (greater than 160 beats per minute) for the term fetus, usually determined by fetal monitoring.
- third stage of labour - interval from the birth of the baby to the expulsion of the placenta and membranes.
- tocolytic - a drug used to prevent or lessen uterine contractions.
- uterotonic - drug used to induce uterine contractions.
- umbilical cord acid-base analysis - clinical perinatal test used to assessing intrapartum hypoxia, measuring one or several indices: arterial umbilical cord blood pH, lactate, and base deficit. Hypoxia is indicated by a low pH, high base deficit and high lactate.
- vacuum extractor - (ventouse) rubber or metal suction cap device used on fetal head to aid birth.
- vertex presentation - (cephalic presentation) where the fetus head is the presenting part, most common and safest birth position.
- Z-score - (standard deviation scores) commonly used to assess growth of preterm infants. For an individual birth weight, a z-score of -1 is one standard deviation below the mean birth weight of the cohort.
- z-score differences - (Zdiff) uses standard deviation scores to analyze changes in growth for a particular observation period.
|
|
|
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 20) Embryology Birth Weight. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Birth_Weight
- What Links Here?
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G