BGDA Practical Placenta - Villi Development
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Chorionic Villi
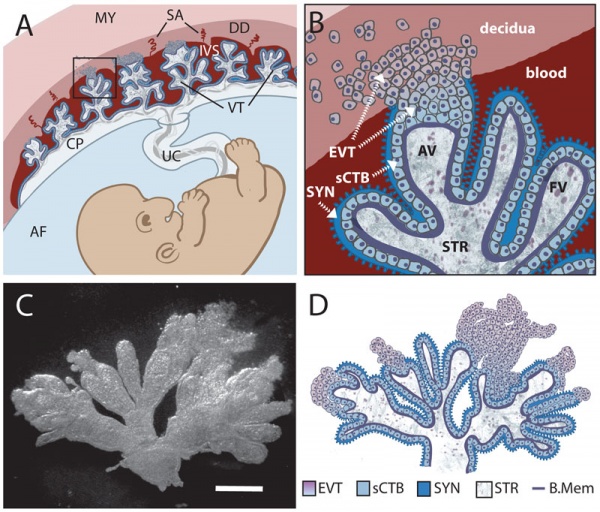
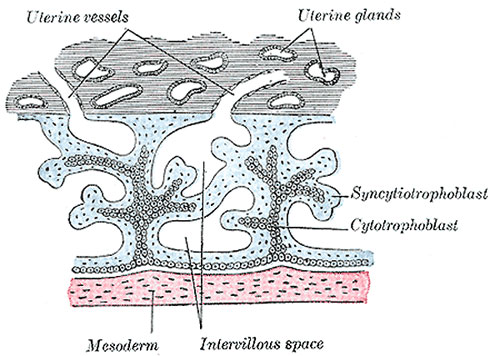
Primary villiWeek 2 - first stage of chorionic villi development. Trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) form finger-like extensions into maternal decidua. |
|
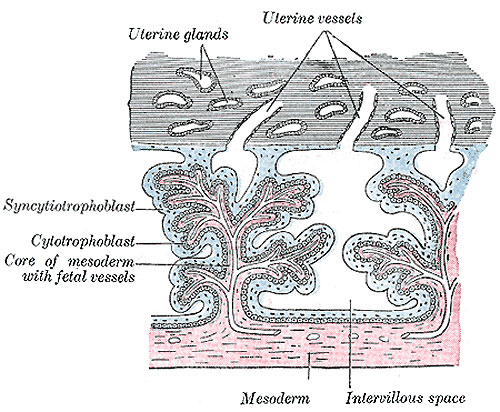
Secondary villiWeek 3 - second stage of chorionic villi development Extra-embryonic mesoderm grows into villi, covers the entire surface of chorionic sac. Basal region will form chorionic plate. |
|
Tertiary villiWeek 4 - third stage of chorionic villi development. Mesenchyme differentiates into blood vessels and cells, forms arteriocapillary network, fuse with placental vessels, developing in connecting stalk. |
|
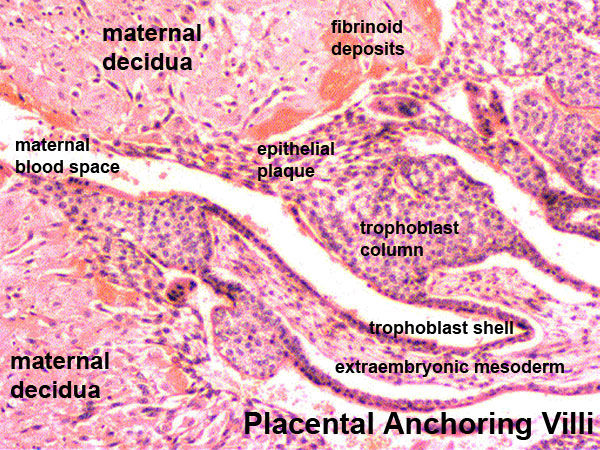
- stem villi - or anchoring villi, cytotrophoblast cells attached to maternal tissue.
- branched villi - grow from sides of stem villi, region of main exchange, surrounded by maternal blood in intervillous spaces.
- terminal villi - not active outgrowths caused by proliferation of the trophoblast. Passive protrusions induced by capillary coiling due to growth of the fetal capillaries within the mature intermediate villi (third trimester).
- chorionic plate - region of membrane at the base of the villi through which placental arteries and vein passes.
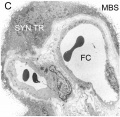
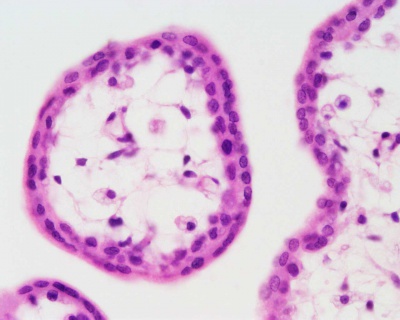
Anchoring Villi Histology
| Moodle Lab Virtual Slides
(you must be logged in to Moodle) |
Please note that there are additional slides listed in the current set, only the first placenta slide and the cord cross-section will be covered in detail in the practical class.
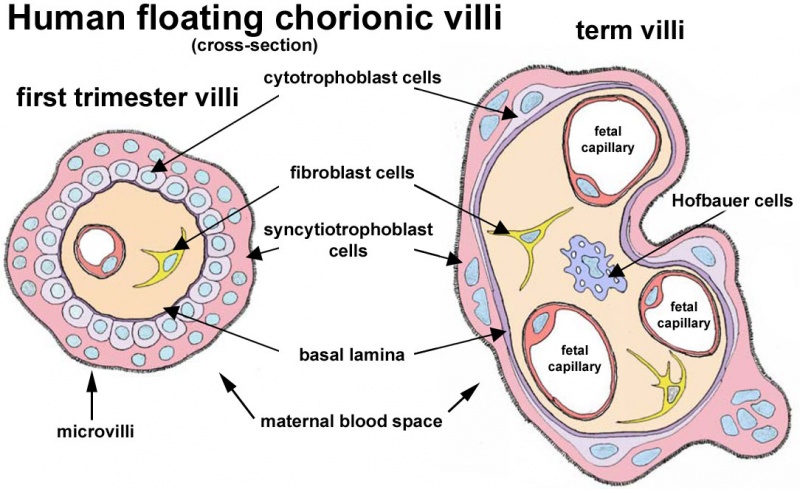
Villi Development
| First Trimester | Third Trimester |
|---|---|
|
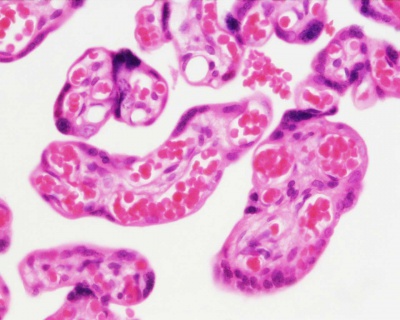
|
Virtual Slide
We will now look at an example of first trimester placentation in a Virtual Slide.
| Slide - Human Placenta |
Please note that there are additional slides listed in the current set, only the first placenta slide and the cord cross-section will be covered in detail in the practical class.
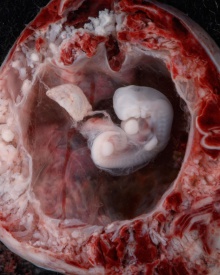
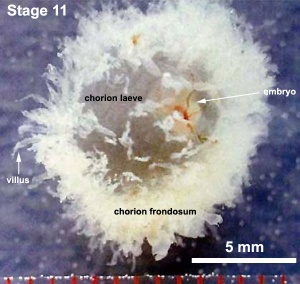
Chorionoic Villi Location
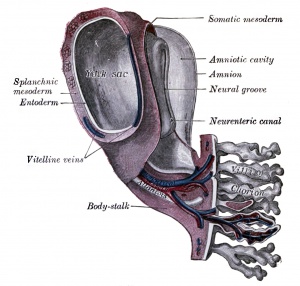
Originally villi cover entire chorionic surface and then become restricted to decidua basalis region forming 2 regions:
- Frondosum - "leafy" where villi are mainly located.
- Capsularis - smooth chorion, where villi are absent or not abundant.
|

|
|
|
|
|
|
Terms
- anastomosis - Term used to describe the connection between two tubes. Applied to describe the connection between peripheral blood vessels without an intervening capillary bed.
- angiogenesis - Term describing the development of new vessels from already existing vessels, this process is secondary to vasculogenesis which is the initial formation of first blood vessels by differentiation of pluripotent mesenchymal cells (extraembryonic mesoderm).
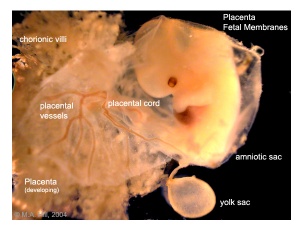
- chorion - The extraembryonic membrane generated from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange.
- chorionic cavity - The fluid-filled extraembryonic coelom (cavity) formed initially from trophoblast and extraembryonic mesoderm that forms placenta. chorion and amnion are made by the somatopleure. The chorion becomes incorporated into placental development. The avian and reptilian chorion lies beside the egg shell and allows gas exchange. In humans, this cavity is lost during week 8 when the amniotic cavity expands and fuses with the chorion.
- chorion frondosum - (frondosum = leafy) The chorion found on conceptus oriented towards maternal blood supply where the majority of villi form and proliferate, will contribute the fetal component of the future placenta.
- chorion laeve - (laeve = smooth) The smooth chorion found on conceptus away from maternal blood supply (towards uterine epithelium and cavity) with very few villi present.
- chorionic villus sampling - (CVS) The taking a biopsy of the placenta, usually at the end of the second month of pregnancy, to test the fetus for genetic abnormalities.
- cord blood - (human umbilical cord blood, HUCB) A term used to describe blood collected from the placenta usually after birth. Has been identified as a source of stem cells with potential therapeutic uses and is stored in Cord Blood Banks throughout the world.
- cotyledon - (Greek, kotyle = a deep cup) In the embryos of seed plants, the "seed leaves," in which nutrients are stored for use after germination. In placental animals, the term is also to describe the leaf-like structure of the placenta surface.
- cytotrophoblast - The "cellular" trophoblast layer surrounding (forming a "shell") the early implanting conceptus. Beginning at uterine adplantation, proliferation and fusion of these cells is thought to form a second outer trophoblast layer, the syncytiotrophoblast. The cytotrophoblast layer contributes to formation of the placental villi, the functional component of the fetal placenta.
- decidua basalis - The term given to the uterine endometrium at the site of implantation where signaling transforms the uterine stromal cells (fibroblast-like) into decidual cells. This forms the maternal component of the placenta, the decidualization process gradually spreads through the remainder of the uterus, forming the decidua parietalis.
- decidua basalis reaction - Term describing the maternal endometrial changes that occur initially at the site of, and following, blastocyst implantation. Seen as a deposition of glycogen, fibrin and proliferation of blood vessels. See also decidualization.
- decidual cell - The uterine stromal cells (fibroblast-like) that differentiate in response to both steroid hormones (progesterone) and embryonic signals. These cells then alter uterine environment to support further embryonic development as well as producing cytokines related to prolactin (PRL) and have an innate immune function.
- decidualization - (decidualisation) The process by which uterine stromal cells differentiate in response to both steroid hormones and embryonic signals into large epitheliod decidual cells. This process is essential for the progress of implantation and establishing fetal-maternal communication.
- fibrinoid layer - (Nitabuch's layer) A layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- floating chorionic villi - Term used to describe the placental microanatomy structure of chorionic villi that are not attached to the maternal decidua and float in the maternal blood-filled space (lacunae). Structurally the same as anchoring chorionic villi conceptus side that are attached to the maternal decidua.These villi go through the same stages of development: primary, secondary and tertiary villi.
- haemotrophic nutrition - Term used to describe in late placenta development the transfer of blood-borne nutrition from maternal to embryo/fetus compared to early histiotrophic nutrition.
- histiotrophic nutrition - Term used to describe in early placenta development the intital transfer of nutrition from maternal to embryo (histiotrophic nutrition) compared to later blood-borne nutrition (hemotrophic nutrition). Histotroph is the nutritional material accumulated in spaces between the maternal and fetal tissues, derived from the maternal endometrium and the uterine glands. This nutritional material is absorbed by phagocytosis initially by blastocyst trophectoderm and then by trophoblast of the placenta. in later placental development nutrition is by the exchange of blood-borne materials between the maternal and fetal circulations, hemotrophic nutrition.
- Hofbauer cells - Cells found within placental villi connective tissue. Have a role as macrophages of mesenchymal origin with potentially additional functions (remodeling, vasculogenesis, regulation of stromal water content).
- hydatiform mole - A uterine tumour with "grape-like" placenta appearance without enclosed embryo formation, arises mainly from a haploid sperm fertilizing an egg without a female pronucleus. It is one form of gestational trophoblastic disease (GTD), a number of abnormalities including hydatiform mole, invasive mole, choriocarcinoma and placental site trophoblastic tumor (PSTT).
- Langhans layer - cytotrophoblast cell layer.
- Nitabuch's layer - (fibrinoid layer) The layer formed at maternal/fetal interface during placentation and is thought to act to prevent excessively deep conceptus implantation. Fibrin-type fibrinoid (maternal blood-clot product) and matrix-type fibrinoid (secreted by invasive extravillous trophoblast cells).
- persistent right umbilical vein - (PRUV) A placental cord abnormality associated with fetal abnormalities and poor neonatal prognosis. The estimated incidence of persistent right umbilical vein in a low-risk population is 1 : 526. PMID 12047534
- placenta - (Greek, plakuos = flat cake) The developmental organ formed from maternal and fetal contributions in animals with placental development. In human, the placenta at term is a discoid shape "flat cake" shape; 20 cm diameter, 3 cm thick and weighs 500-600 gm. Placenta are classified by the number of layers between maternal and fetal blood (Haemochorial, Endotheliochorial and Epitheliochorial) and shape (Discoid, Zonary, Cotyledenary and Diffuse). The placenta has many different functions including metabolism, transport and endocrine.
- placental arteries - (umbilical arteries) In placental animals, the blood vessels which develop within the placental cord carrying relatively deoxygenated blood from the embryo/fetus to the placenta. In humans, there are two placental arteries continuous with the paired internal iliac arteries (hypogastric arteries) arising off the dorsal aortas. At birth this vessel regresses and form the remnant medial umbilical ligament.
- placental cord - (umbilical cord) The placental cord is the structure connecting the embryo/fetus to the placenta. It is initially extra-embryonic mesoderm forming the connecting stalk within which the placental blood vessels (arteries and veins) form. In human placental cords the placental blood vessels are initially paired, later in development only a single placental vein remains with a pair of placental arteries. This structure also contains the allantois, an extension from the hindgut cloaca then urogenital sinus. Blood collected from the placental cord following delivery is a source of cord blood stem cells.)
- placental membranes - chorionic membrane A#amniotic membrane) General term to describe the membrane bound extra-embryonic fluid-filled cavities surrounding the embryo then fetus. In humans the A#amniotic membrane and chorionic membrane fuse.
- placental vein - (umbilical vein) In placental animals, the blood vessels which develop within the placental cord carrying relatively oxygenated blood from the placenta to the embryo/fetus. In humans, there are initially two placental veins which fuse to form a single vein. The resence of paired veins in the placental cord can be indicative of developmental abnormalities.
- primary villi - (primary chorionic villi) Term describing the earliest stage of embryonic placenta development. In humans, the conceptus during week 2 this first stage of chorionic villi development consists of only the trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) forming finger-like extensions into maternal decidua. Initially these finger-like projections cover the entire surface of chorionic sac and later become restricted to the placental surface. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development. Placental villi stages: primary villi - secondary villi - tertiary villi
- secondary villi - (secondary chorionic villi) Term describing the second stage of embryonic placenta development. In humans, the conceptus during week 3 onward this stage of chorionic villi development consists of the trophoblastic shell cells (syncitiotrophoblasts and cytotrophoblasts) filled with extraembryonic mesoderm forming finger-like extensions into maternal decidua. Initially these finger-like projections cover the entire surface of chorionic sac and later become restricted to the placental surface. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development. Placental villi stages: primary villi - secondary villi - tertiary villi
- syncytiotrophoblast - A multinucleated cell currently thought to form by the fusion of another trophoblast cell the cytotrophoblasts, within the trophoblast layer (shell) of the implanting conceptus. In early development, these cells mediate implantation of the conceptus into the uterine wall and secrete the hormone (human Chorionic Gonadotrophin, hCG) responsible for feedback maintainance of the corpus luteum (in maternal ovary) and therefore maintaining early pregnancy.
- tertiary villi - (tertiary chorionic villi) Term describing the final stage of embryonic placenta development. In humans, the conceptus after week 3 the chorionic secondary villi now develop placental blood vessels within the core extraembryonic mesoderm. The villi form finger-like extensions that are either anchoring chorionic villi attached to the maternal decidua or floating chorionic villi in maternal lacunae. The villi stages are ongoing as the placenta continues to grow through both the embryonic and fetal development. Placental villi stages: primary villi - secondary villi - tertiary villi
- villi - Plural of villus, which is a thin projection from a surface. The term in development is used to describe the individual functional units together of the fetal placenta.
- Wharton's jelly - Placental cord (umbilical cord) gelatinous connective tissue composed of myofibroblast-like stromal cells, collagen fibers, and proteoglycans. Increases in volume (myxomatous, connective tissue embedded in mucus) at parturition (birth) to assist closure of placental blood vessels. Matrix cells from Wharton's jelly have recently been identified as a potential source of mesenchymal stem cells (MSC), also called mesenchymal stromal cell. This placental cord substance is named after Thomas Wharton (1614-1673) an English physician and anatomist who first described this placental tissue.
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
2013 Meeting Presentation - Placenta Embryology and Circulation
Cytotrophoblast Layer
There is a new interpretation of the changes that are occuring in the cytotrophoblast (CTB) layer during early to full-term human placenta development. Traditionally the interpretation was that the cytotrophoblast layer thinned and became discontinuous towards term. The thinning is thought due to the epithelium surface expanding at a faster rate than its volume. Two recent studies suggest that while the cytotrophoblast layer does indeed thin, it does not become discontinuous.
Syncytiotrophoblast Layer
The syncytiotrophoblast (STB) layer forms the epithelial covering of the entire villous tree. These cells are multinucleated, terminally-differentiated syncytium formed by the fusion of the underlying progenitor cytotrophoblast (CTB) cells. The process is described as "syncytialization" and is mediated by syncytin-1, an envelope protein of a human endogenous retrovirus W (HERV-W). The differentiation is regulated by chorionic gonadotropin (hCG) and the fusion of cytotrophoblast cells is ongoing during placental development.
Cellular parts derived from the syncytiotrophoblasts (apoptotic nuclei and microparticulate debris) can be shed into the maternal blood in which they are bathed. The apototic process appears to be part of the fusion mechanism between cytotrophoblast and the overlying multinucleate syncytiotrophoblast layer.
Studies have suggested that these cells are transcriptionally inactive. A recent study using a number of different detection techniques now suggests that at least some of the cells nuclei may still be transcriptionally inactive.
Mesenchymal Villi
Mesenchymal villi generate all other villous types:
- immature intermediate villi
- stem villi
- mature intermediate villi
- terminal villi
Mesenchymal villi continuously form out of the trophoblastic sprouts throughout pregnancy and have been considered the basis for growth and differentiation of the villous trees.
Human Villi Timeline
This is far more than even for additional information section Timeline Table
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |