BGDA Practical Placenta - Implantation and Early Placentation
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Early Placenta
|
|
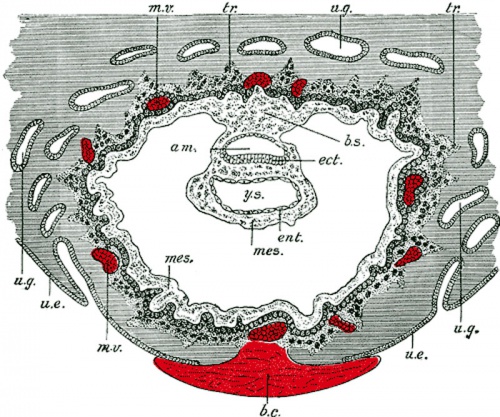
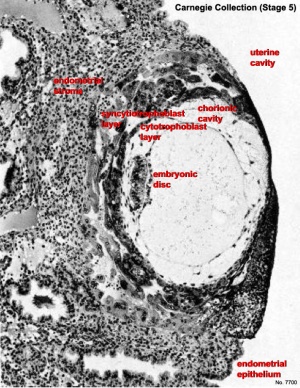
| Human Embryo Day 8 to 9 | Human Embryo - early implantation (stage 5) |
Uterine surface view of implantation site
Simplified Cartoons
Movies
|
|
|
|
Terms
- adplantation - The term used to describe the initial process of the blastocyst (conceptus) attachment to the uterine endometrium wall at the site of implanation following hatching from the zona pellucida.
- cytotrophoblast - The "cellular" trophoblast layer surrounding (forming a "shell") the early implanting conceptus. Beginning at uterine adplantation, proliferation and fusion of these cells is thought to form a second outer trophoblast layer, the syncytiotrophoblast. The cytotrophoblast layer contributes to formation of the placental villi, the functional component of the fetal placenta.
- decidua basalis - The term given to the uterine endometrium at the site of implantation where signaling transforms the uterine stromal cells (fibroblast-like) into decidual cells. This forms the maternal component of the placenta, the decidualization process gradually spreads through the remainder of the uterus, forming the decidua parietalis.
- decidualization - The process by which uterine stromal cells differentiate in response to both steroid hormones and embryonic signals into large epitheliod decidual cells. This process is essential for the progress of implantation and establishing fetal-maternal communication.
- endometrial gland - The mucous secreting gland associated with the epithelium lining the uterus. These glands develop and secrete each menstrual cycle and are thought to provide initial blastocyst nutrition prior to implantation.
- endometrium - The epithelium lining of the non-pregnant uterus. During pregnancy this epithelium undergoes changes described as the decidual reaction and is renamed the "decidua".
- extraembryonic coelom - The space found outside the embryo, amniotic cavity, yolk sac and chorionic cavity.
- extraembryonic mesoderm - Cells from the conceptus that contribute to placenta and fetal membranes. Described as "extraembryonic" because it is tissue lying outside the embryonic trilaminar disc (ectoderm, mesoderm and endoderm) and "mesoderm", because of the connective tissue cellular organization. In animal models, this extraembryonic mesoderm has been shown to arise from the same source as embryonic mesoderm during gastrulation.
- haemochorial - The type of placenta where the chorion comes in direct contact with maternal blood. This is the type of human placentation.
- implantation - The term used to describe the process of conceptus invasion of the uterus endometrium (epithelium and underlying stroma) by the blastocyst (conceptus). This process follows conceptus adplantation (attachment) to the endometrium. Abnormal implantation is where this process does not occur in the body of the uterus (ectopic) or where the placenta forms incorrectly. In humans, implantation occurs during the second week of development.
- placenta - (Greek, plakuos = flat cake) The developmental organ formed from maternal and fetal contributions in animals with placental development. In human, the placenta at term is a discoid shape "flat cake" shape; 20 cm diameter, 3 cm thick and weighs 500-600 gm. Placenta are classified by the number of layers between maternal and fetal blood (Haemochorial, Endotheliochorial and Epitheliochorial) and shape (Discoid, Zonary, Cotyledenary and Diffuse). The functional exchange region are the placental villi or chorionic villi. The placenta has many different functions including metabolism, transport and endocrine.
- syncytiotrophoblast - A multinucleated cell currently thought to form by the fusion of another trophoblast cell the cytotrophoblasts, within the trophoblast layer (shell) of the implanting conceptus. In early development, these cells mediate implantation of the conceptus into the uterine wall and secrete the hormone (human Chorionic Gonadotrophin, hCG) responsible for feedback maintainance of the corpus luteum (in maternal ovary) and therefore maintaining early pregnancy.
- villi - Plural of villus, which is a thin projection from a surface. A term used to describe the many functional units together of the fetal placenta.
- villous cytotrophoblast - (VCT) Trophoblast cells located on chorionic villi (as opposed to extravillous cytotrophoblasts) that can also fuse to form the syncytiotrophoblasts.
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
Carnegie Stage 5
Historically this early implantation stage was divided into 3 separate sub-stages (a-c).
Stage 5a
Stage 5b
Stage 5c
Maternal Immune
How does the implanting conceptus avoid immune rejection by the maternal immune system? There are a number of maternal and embryonic mechanisms that are thought to act to prevent immune rejection of the implanting conceptus, though the complete mechanism(s) are unknown. This is particularly relevant to Assisted Reproductive Technologies involving donor eggs.
Below are some examples of research on this topic.
Decidual Immune Cells
- Specialised immune cells.
| Decidual Macrophages (Mϕ) | Decidual T cells | Uterine Natural Killer cells |
|---|---|---|
|
|
|
Chemokine Gene Silencing
- Remove the attraction of maternal immune cells.
A mouse study[1] has shown that the normal immune response to inflammation, accumulation of effector T cells in response to chemokine secretion does not occur during implantation. This is prevented locally by epigenetic silencing of chemokine expression in the decidual stromal cells.
Corticotropin-Releasing Hormone
- Kill the maternal immune cells.
Both maternal and implanting conceptus release CRH at the embryo implantation site. This hormone then binds to receptors on the surface of trophoblast (extravillous trophoblast) cells leading to expression of a protein (Fas ligand, FasL) that activates the extrinsic cell death pathway on any local maternal immune cells ( T and B lymphocytes, natural killer cells, monocytes and macrophages).[2] (Note - This cannot be the only mechanism, as mice with dysfunctional FasL proteins are still fertile).