BGDA Practical Placenta - Diagnostic Techniques
| Practical 14: Implantation and Early Placentation | Villi Development | Maternal Decidua | Cord Development | Placental Functions | Diagnostic Techniques | Abnormalities |
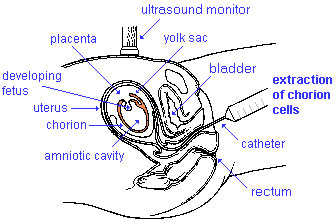
Chorionic Villus Sampling
|
Chorionic Villus Sampling test is done in GA week 10 to 12.
The test is done by looking at cells taken from the chorionic membrane or placenta. No anaesthetic is required, and a test result is usually available in two to three weeks. When the test is carried out by an obstetrician experienced in the technique, the risk of miscarriage related to the test is about 2%. Potential disadvantages include maternal cell contamination, placental mosaicism and failure to obtain an adequate specimen. This may result in the need for a repeat procedure or amniocentesis.
|
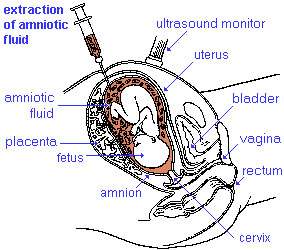
Amniocentesis
|
Amniocentesis is a prenatal diagnostic test carried out mainly between GA week 14 to 18.
Amniotic fluid is taken from the uterus, sent to a diagnostic laboratory and embryonic cells isolated from the amniotic fluid. No anaesthetic is required, and a result is usually obtained in about three to four weeks. When the test is carried out by an obstetrician experienced in the technique, the risk of a miscarriage related to the test is about 1 %.
|
What does a DNA Sequencer look like?
Ultrasound
Placenta - position, size and structure.
|
| Ultrasound 12wk |
| Page | Play |
Placenta Term Parameters
There are a variety of diagnostic and morphological measurements that can be made of the placenta during pregnancy and at term.
Simple measurements of overall placental diameter, thickness and volume:
- placental diameter - is measured in the transverse section by calculating the maximum dimensions of the chorionic surface.
- placental thickness - is measured at its mid-portion from the chorionic plate to the basilar plate, on a longitudinal plane (less than 4 cm at term). Excludes any abnormalities (fibroids, myometrial contractions, or venous lakes). The placental thickness approximates in millimeters to the weeks of gestation.
- placental volume - is measured by a range of different methods and calculations, more recently with three-dimensional ultrasound.
Amniotic Fluid Volume
The amniotic fluid volume increases as the embryo and then fetus grows and rate of change varies during the pregnancy.
- up to 8 weeks - increases at 10 ml/week
- 8 to 13 weeks - increases at 25 ml/week
- 13 to 21 weeks - increases at 60 ml/week
- 21 to 33 weeks - amniotic volume increase starts decreasing and eventually levels.
- 34 weeks (GA) - peaks at about 800 mL.
- 40 weeks (GA) - about 600 mL at term.
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
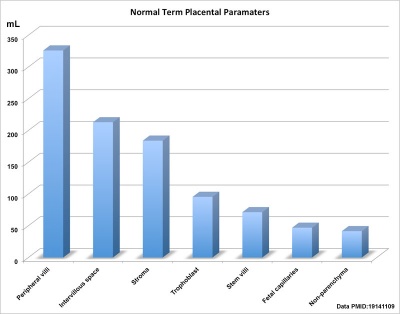
Term placental composition, villous capillarization and the mean cross-sectional areas of peripheral villi and capillaries, data from a study sample of 15 normal placenta (mean placental volume, 652 ml). [1]
| Variable | Unit | Placenta (mean, n = 15) |
| Intervillous space | mL | 213 |
| Stem villi | mL | 71.4 |
| Peripheral villi | mL | 326 |
| Trophoblast | mL | 95.5 |
| Stroma | mL | 184 |
| Fetal capillaries | mL | 46.9 |
| Non-parenchyma | mL | 41.5 |
| Peripheral villi | km | 89.2 |
| Fetal capillaries | km | 310 |
| TS area villi | µm2 | 3700 |
| TS area capillary | µm2 | 150 |
| Capillaries | mL mL-1 | 0.147 |
| Length ratio | km km-1 | 3.6 |
- ↑ <pubmed>19141109</pubmed>
Terms
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 19) Embryology BGDA Practical Placenta - Diagnostic Techniques. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_Placenta_-_Diagnostic_Techniques
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G