BGDA Practical 3 - Oogenesis and Ovulation: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 161: | Line 161: | ||
* '''oogenesis''' - (Greek, ''oo'' = egg + ''genesis'' = origin, creation, generation) process of diploid oogonia division and differentiation into an haploid oocyte (egg) within the [[O#ovary|ovary]] (female gonad). Mammalian meiosis will only be completed within the oocyte if [[F#fertilization|fertilization]] occurs. | * '''oogenesis''' - (Greek, ''oo'' = egg + ''genesis'' = origin, creation, generation) process of diploid oogonia division and differentiation into an haploid oocyte (egg) within the [[O#ovary|ovary]] (female gonad). Mammalian meiosis will only be completed within the oocyte if [[F#fertilization|fertilization]] occurs. | ||
* '''oogonia''' - (Greek, ''oo'' = egg) diploid germ cells within the [[O#ovary|ovary]] (female gonad) which provide the primary oocytes for oocyte (egg) formation. In humans, all oogonia form primary oocytes within the [[O#ovary|ovary]] before birth. | * '''oogonia''' - (Greek, ''oo'' = egg) diploid germ cells within the [[O#ovary|ovary]] (female gonad) which provide the primary oocytes for oocyte (egg) formation. In humans, all oogonia form primary oocytes within the [[O#ovary|ovary]] before birth. | ||
* '''oolemma''' - (zona pellucida, vitelline membrane) | |||
* '''oophorus''' - (Greek, ''oo'' = egg + ''phorus'' = carrying, egg-bearing) cumulus oophorus, used to describe the granulosa cells within the follicle that tether or link the oocyte to the wall of the follicle. | * '''oophorus''' - (Greek, ''oo'' = egg + ''phorus'' = carrying, egg-bearing) cumulus oophorus, used to describe the granulosa cells within the follicle that tether or link the oocyte to the wall of the follicle. | ||
* '''ovulation''' - release of the oocyte from the mature follicle. In humans generally a single oocyte is released from a cohort of several maturing follicles. | * '''ovulation''' - release of the oocyte from the mature follicle. In humans generally a single oocyte is released from a cohort of several maturing follicles. | ||
Revision as of 10:55, 4 August 2014
| Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 |
Introduction
This page covers gametogenesis within the ovary. With the help of the tutors and other students you will work your way through identifying features described in the text.
Begin by looking at the ovary and the formation of the follicle containing the egg which matures and is released upon ovulation. The images are arranged in series so that progressive stages of the maturing follicle can be seen. The final image on this current page is a link to a movie showing follicle development and ovulation. Use the series of images of the cat ovary below to identify the key features described in the associated text.
Note: This should be a revision of the Female Histology Practical (support page) you have already completed. If you have trouble with the terms, there is a glossary at the bottom of each page.
Oogenesis
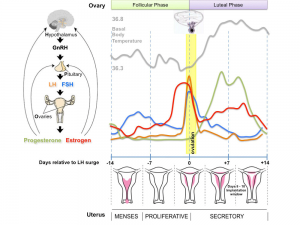
The graph below shows the changes in human germ cell numbers in the ovary with age, peaking at several million (occuring in early fetal development) and then decreasing by apopotic cell death. At puberty there remain only about 400,000 and only about 10% of these will be released through reproductive life. (More? Menstrual Cycle)
In the developing human ovary, oocytes remain at the diplotene stage of the first meiosis from fetal life through postnatal childhood, until puberty when the lutenizing hormone (LH) surges stimulate the resumption of meiosis.
Whole Ovary
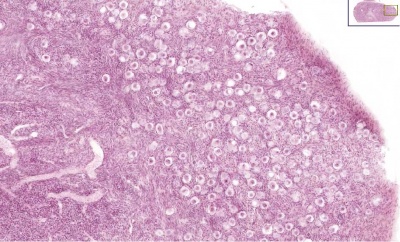
Ovary (cat, cross-section) showing histology and maturation of follicle.
Image (low magnification) showing cortical primordial follicles with primary (preantral) and secondary (antral) follicles lying deeper. Mesovarium at lower right and blood vessels in medullary region.
At this magnification, the overall organization of the ovary can be observed, cortex/medulla organization and arrangement of the maternal blood vessels, but few specific follicle details can be seen.
The next image is of the ovarian cortical region.
Ovary Cortex (low power)
Ovary cortex showing primordial follicles.
At the top of the image, is the outside of the ovary.
The thick connective tissue outer layer is the tunica albuginea. Over which a single layer of cells called the germinal epithelium (not visible) cover the surface of the ovary.
The next layer contains the earliest primordial follicles, single cells with pale cytoplasm and darkly stained nuclei.
The next layer contains many growing follicles at various stages of maturity and development. There is also evidence of degeneration as atretic follicles.
At the bottom of the image, is the medullary region of the ovary. Note the large number of maternal blood vessels which are the circulatory conduits for the estrogens and progesterones produced by the theca surrounding the ovarian follicles.
Note: germinal epithelium, tunica albuginea, primordial and atretic follicles. Note larger preantral follicle with (from the centre out) nucleus of maturing oocyte, oocyte cytoplasm, zona pellucida (pink ring), follicle cells, stromal cells.
Ovary Cortex Primordial and Primary Follicles
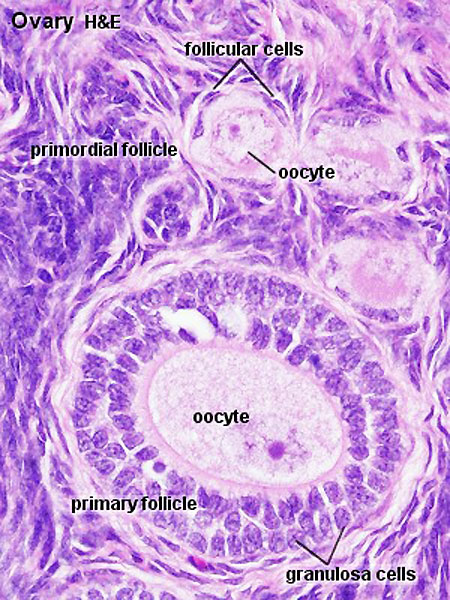
View of cortical ovary region showing primordial follicles and a single preantral follicle, with atretic follicle to its left. Bottom of picture shows outer cells of antral follicle.
High power view of ovary cortical region showing primordial follicles and a single preantral follicle.
Features: germinal epithelium, tunica albuginea, preantral follicle, nucleus of oocyte, oocyte cytoplasm, zona pellucida, Call-Exner body, stratum granulosa, basement membrane, theca, blood vessels surrounding follicle in theca layer.
Ovary Cortex and Medulla
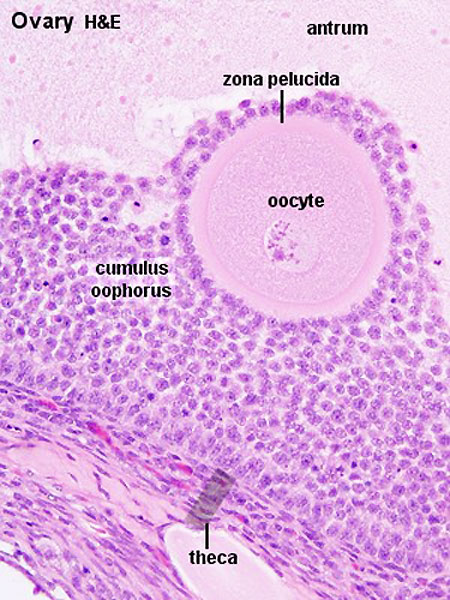
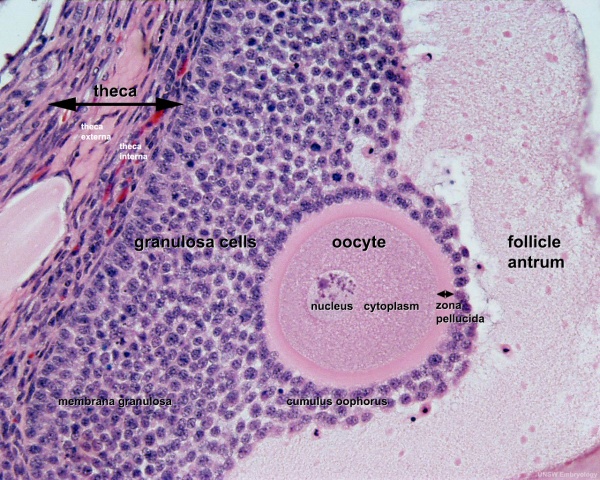
Low power view of ovary cortex and medullary region and high power image within an antral follicle.
In the low power image note 3 stages of follicle development (primordial, preantral and antral).
Features:
- cortical primordial follicles
- oocyte
- follicular cells
- stromal cells
- preantral follicle- zona pellucida, stratum granulosa, theca
- early preovulatory follicle (Graafian) - oocyte, zona pellucida, corona radiata, cumulus oophorus, liquor folliculi, stratum granulosa, theca interna, theca externa, blood vessels surrounding follicle
Follicle Development
The development of a primordial follicle to a preovulatory follicle takes in excess of 120 days. After it has become a primary follicle of about 0.2 mm diameter it takes about 65 days to develop into a preovulatory follicle. Cohorts of follicles continually develop but only one is most sensitive to hormonal stimulation and is "selected", becoming the dominant follicle. All others in this cohort will undergo atresia.
Fertility Treatments
Superovulation therapy is a fertility drug treatement (oral clomiphene citrate and/or injectable FSH with or without LH) aimed at stimulating development/release of more than one follicle during a single menstrual cycle.
Follicle Classification
The above images show the histological changes that occur with follicle development (folliculogenesis). In humans, this entire process occurs over the timecourse of at least 3 menstrual cycles. This means that within the ovary during each cycle (at any point in time) many follicles can be either developing (folliculogenesis), regressing (atresis) and only a single follicle will be selected as ready for release. The selected follicle readied for release, generally one of the largest antral follicle, and can be classifed or described as: an antral preovulatory follicle or Graafian follicle or type 8 follicle (depending upon the classification used).
Classification systems - There are several different nomenclatures for the stages of follicle maturation (shown below) all of which makes the literature very confusing.
The simplest is primordial, preantral, antral, Preovulatory (Graaffian). You can also use the 5 step follicle classification: Primordial, Primary, Secondary, Tertiary, Preovulatory. Note that some classifications refer to the antral follicle as a secondary follicle and do not use the term tertiary follicle.
Primordial Follicle
Alternative nomenclature: small follicle or type 1, 2, 3 (25 cells) less than 50 micron diameter
Primary Follicle
Alternative nomenclature: preantral follicle or type 4 (26-100 cells), type 5 (101-300 cells) up to 200 micron diameter
Secondary Follicle
Alternative nomenclature: small antral type 6 (301-500 cells), small antral 500 micron diameter.
Tertiary Follicle
Alternative nomenclature: large antral type 7 (501-1000 cells) large antral 1000-6000 micron diameter.
Preovulatory Follicle
Alternative nomenclature: largest antral follicle or Graafian follicle or type 8 (>1000 cells) greater than 6000 micron diameter
Atresia
At any one time the majority of follicles are destined not to complete maturation and at any stage (from type 4-7) degeneration of the follicle can occur, this process is called atresia.
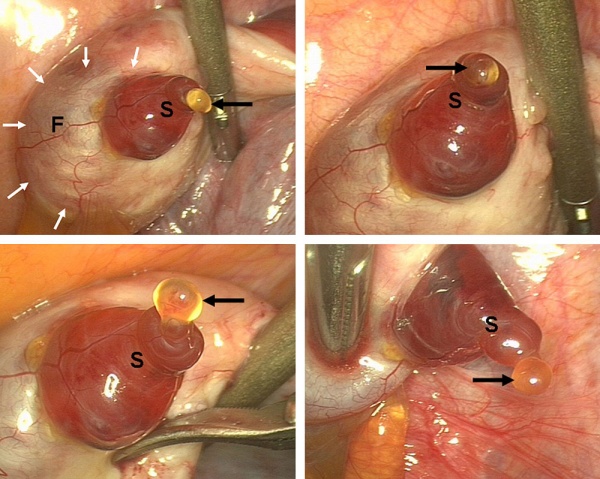
Ovulation
Human Ovulation
|
|
Movie showing process of ovulation (release of oocyte and follicular fluid). Click on image or links to start movie.
Note that following ovulation the remnant of the follicle will degenerate if implantation does not occur (non-pregnant) forming a corpus albicans or following implantation (pregnancy) a corpus luteum which provides endocrine support to the uterus.
An endocrine signal (hCG human Chorionic Gonadotropin) from the implanting conceptus syncitiotrophoblasts maintains the corpus luteum, which in turn supports the uterine functional lining, preventing menstruation.
| Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 |
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Terms
- antral follicle - (secondary) the stage following preantral in the decription of the sequence ovarian follicle development.
- antrum - (L. a cave), cavity; a nearly-closed cavity or bulge. In the ovary this refers to the follicular fluid-filled space within the follicle.
- atretic follicle - An ovarian follicle that fails to mature and degenerates. Also called "atresia" refering to the process of degeneration of the ovarian follicle. This process can occur at any stage of follicle development (folliculogenesis).
- clomiphene citrate - drug taken orally to promote the process of follicle/egg maturation.
- corona radiata - Layer of follicle cells of cumulus oophorus remaining attached to zona pellucida of oocyte after ovulation. Also called granulosa cells.
- corpus albicans - (L. corpus = body, L. albicans = whitish); a degenerating corpus luteum in ovary.
- corpus luteum - (L. corpus = body, L. luteum = yellow) The remains of ovarian follicle after ovulation that acts as an endocrine organ supporting pregnancy and preventing menstruation (loss of the endometrial lining). de Graaf first observed it in the ovary of a cow as a yellow structure.
- cortical - (L. corticalis) at the outside (like the bark of a tree), usually combined with medulla meaning the core.
- cumulus oophorus - (L. cumulus = a little mound G. oon = egg + phorus = bearing); part of the wall of an ovarian follicle surrounding and carrying the ovum (oocyte).
- follicle - (L. folliculus = little bag,dim. of L. follis). A structure which develops in the ovary and contains a developing egg (oocyte).
- follicle stimulating hormone - (FSH, gonadotropin) A glycoprotein hormone secreted by anterior pituitary (adenohypophysis gonadotrophs, a subgroup of basophilic cells) and acts on gametogenesis and other systems in both males and females. Females, FSH acts on the ovary to stimulate follicle development. Males, acts on the testis Sertoli cells to increase androgen-binding protein (ABP) that binds androgens and has a role in spermatogenesis.
- follicular fluid - the fluid found in the antrum of a secondary follicle. Secreted by cells in the wall of the follicle. This fluid is released along with the oocyte at ovulation.
- germinal epithelium - cellular component covering surface of ovary, it is continuous with mesothelium covering mesovarium. Note that it is a historical misnomer, as it is not the actual site of germ cell formation.
- Graafian follicle - named after Regnier de Graaf (1641-1673), an historic Dutch physician embryologist who studied pregnancy using rabbits.
- granulosa cells - the supporting cells that surround the developing egg within the follicle thecal layers.
- luteinizing hormone - (LH, gonadotropin, lutropin, Interstitial Cell Stimulating Hormone, ICSH) glycoprotein hormone releasd from anterior pituitary hormone that acts on the gonad and has a role in male and female reproduction. Female, LH triggers ovulation (release of the oocyte). Male, LH stimulates testis interstital cell (Leydig cell) production of testosterone. Have been used clinically in humans for the treatment of female infertility.
- mesovarium - mesentry of the ovary formed from a fold of the broad ligament that attaches the ovary.
- medullary - (L. medius = in the middle) relating to the medulla; pith, marrow, inner portion of an organ. Usually combined with cortex (cortical) meaning the outer layer.
- oocyte - (Greek, oo = egg, ovum) The term used to describe the haploid egg or ovum formed within the ovary (female gonad) and released to enter the uterine tube and be transported to the uterus. The mature oocyte is the cell released from the ovary during ovulation.
- oocyte retrieval - (egg retrieval) A clinical in vitro fertilization (IVF) procedure to collect the eggs contained in the ovarian follicles.
- oogenesis - (Greek, oo = egg + genesis = origin, creation, generation) process of diploid oogonia division and differentiation into an haploid oocyte (egg) within the ovary (female gonad). Mammalian meiosis will only be completed within the oocyte if fertilization occurs.
- oogonia - (Greek, oo = egg) diploid germ cells within the ovary (female gonad) which provide the primary oocytes for oocyte (egg) formation. In humans, all oogonia form primary oocytes within the ovary before birth.
- oolemma - (zona pellucida, vitelline membrane)
- oophorus - (Greek, oo = egg + phorus = carrying, egg-bearing) cumulus oophorus, used to describe the granulosa cells within the follicle that tether or link the oocyte to the wall of the follicle.
- ovulation - release of the oocyte from the mature follicle. In humans generally a single oocyte is released from a cohort of several maturing follicles.
- preantral follicle - (primary) the stage following primordial in the description of the sequence ovarian follicle development.
- primary follicle - (preantral) the stage following primordial in the description of the sequence ovarian follicle development.
- primordial follicle - the first stage in the description of the sequence ovarian follicle development. Present in the ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. The primordial follicle is the oocyte and the surrounding follicular cells.
- primordial germ cell - oocyte present in the primordial follicle ovary from birth, located in the stroma of the ovary cortex beneath the tunica albuginea. The primordial follicle is the oocyte and the surrounding follicular cells.
- secondary follicles - the stage following primary in the description of the sequence ovarian follicle development.
- stromal cells - in the ovary, cells surrounding the developing follicle that form a connective tissue sheath (theca folliculi). This layer then differentiates into 2 layers (theca interna, theca externa). This region is richly vascularized and involved in hormone secretion.
- superovulation therapy - a fertility drug treatement (oral clomiphene citrate and/or injectable FSH with or without LH) aimed at stimulating development/release of more than one follicle during a single menstrual cycle.
- tertiary follicle - (preovulatory, Graffian) the stage following secondary in the description of the sequence ovarian follicle development.
- theca folliculi - stromal cells in the ovary, cells surrounding the developing follicle that form a connective tissue sheath. This layer then differentiates into 2 layers (theca interna, theca externa). This region is vascularized and involved in hormone secretion.
- theca externa - stromal cells forming the outer layer of the theca folliculi surrounding the developing follicle. Consisting of connective tissue cells, smooth muscle and collagen fibers.
- theca interna - stromal cells forming the inner layer of the theca folliculi surrounding the developing follicle. This vascularized layer of cells respond to LH (leutenizing hormone) synthesizing and secreting androgens which are processed into estrogen.
- tunica albuginea - dense connective tissue layer lying between germinal epithelium and cortical region of ovary.
- uterus - site of embryo implantation and development. Uterine wall has 3 major layers: endometrium, myometrium, and perimetrium. Endometrium can be further divided into the functional layer (shed/lost during menstruation) and basal layer (not lost during menstruation).
- zona pellucida - extracellular layer lying directly around the oocyte underneath follicular cells. Has an important role in egg development, fertilization and blastocyst development. This thick extracellular matrix consists of glcosaminoglycans and 3 glycoproteins (ZP1, ZP2, ZP3).
Additional Information
| Additional Information - Content shown under this heading is not part of the material covered in this class. It is provided for those students who would like to know about some concepts or current research in topics related to the current class page. |
- Female Histology - covered in another Histology practical class. Virtual Slides
- Premature Ovarian Failure
- Menopause
- History of the Pap Smear
- Gynaecological cancer information, as they are an important clinical topic specific to these reproductive organs.
Premature Ovarian Failure
Premature Ovarian Failure (POF)[1] a clinical term describes the absence of normal ovarian function due to the depletion of the primordial follicle pool before 40 years of age a range of factors (autoimmune, iatrogenic, infections, genetic defects). This occurs in approximately 1% of women below 40 years of age.
Premature Ovarian Failure (POF) can be primary or secondary based on puberty.
- primary - absence of puberty, development and primary amenorrhea, generally caused by ovarian dysgenesis (45XO, Turner syndrome).
- secondary - normal puberty, usually present with the later disappearance of menstrual cycles.
Menopause
Term describes the physiological changes that accompany the age related loss of fertility. There is a decrease in ovarian follicle numbers, gradually elevated FSH levels, onset of cycle irregularity leading to the final cessation of menses.[2] A recent review[3] has looked at genetic factors that could affect the age at natural menopause and identified from linkage analyses (9q21.3 and chromosome 8 at 26 cM) and association studies genomic regions (19q13.42 and 20p12.3), containing two promising candidate genes (Bruck syndrome 1, BRKS1) and Menopause quantitative trait locus 3 (MENOQ3).[4].
History of the Pap Smear
(Papanicolaou smear, pap test, cervical smear) The text below is from the ABC - Great Moments In Science.
- "Luckily, we have the famous Pap Smear - an excellent way to find cancer of the cervix before it digs in locally and/or spreads throughout the body. The Pap Smear is named after a certain Dr. Papanicolaou - who did a Pap Smear on his wife virtually every day for 20 years.
- George Nikolas Papanicolaou was born in 1883 in Kymi, a small town overlooking the Aegean Sea on the Island of Euboea in Greece. His father, Nikolas Papanicolaou was both the Major of Kymi and a medical doctor. His older brother, Naso, had studied law, so his father convinced George to continue in the family medical tradition. So George studied medicine, and did well, graduating with a degree in honours in 1904............"
- Links: Menstrual Cycle - Histology | Dilatation and curettage (D&C) | ABC - Great Moments In Science
Gynaecological Cancers
Main Types: Ovarian cancer (ICD-10 code C56) | Cervical cancer (ICD-10 code C53) | Uterine cancer (ICD-10 codes C54 and C55) | Other gynaecological cancers (ICD-10 codes C51, C52, C57 and C58)
Ovarian cancer in Australia: an overview, 2010
- "Ovarian cancer was the most common cause of gynaecological cancer death and the sixth most common cause of cancer-related death among Australian women in 2006."
Cervical screening in Australia 2006-2007
- "Incidence and mortality of cervical cancer in Australia remain low, consistent with the Program’s aim to reduce incidence and mortality. There were 9.2 new cases per 100,000 women in 2005, and 1.9 deaths per 100,000 women in 2006 (aged 20-69 years). Incidence for Aboriginal and Torres Strait Islander women has been estimated to be more than double (ABS & AIHW 2008), and mortality found to be five times that of other Australian women."
- Links: Ovarian cancer in Australia: an overview, 2010 | Australian Gynaecological cancer projections 2010-2015
- ↑ <pubmed>16722528</pubmed>
- ↑ <pubmed>19589949</pubmed>| Endocr Rev
- ↑ <pubmed>20071357</pubmed>
- ↑ <pubmed>19448619</pubmed>
| Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 |
BGDA: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12 | Lecture Neural | Practical 14 | Histology Support - Female | Male | Tutorial
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 16) Embryology BGDA Practical 3 - Oogenesis and Ovulation. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/BGDA_Practical_3_-_Oogenesis_and_Ovulation
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G