Abnormal Development - Hydatidiform Mole: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 22: | Line 22: | ||
|-bgcolor="F5FAFF" | |-bgcolor="F5FAFF" | ||
| | | | ||
* '''Risk of recurrent molar pregnancies following complete and partial hydatidiform moles'''<ref name="PMID26202916"><pubmed>26202916</pubmed></ref> "What is the risk of further molar pregnancies for women with one or more hydatidiform moles (HM) in relation to molar subtype. SUMMARY ANSWER: Women with a complete hydatidiform mole (CM) have a 1 in 100 and 1 in 4 risk of further CM after one or two consecutive CM, respectively, while women with a partial hydatidiform mole (PM) have only a small increase in risk for further molar pregnancies. WHAT IS KNOWN ALREADY: Women with a molar pregnancy have an increased risk of further HM. A small subgroup of women with recurrent HM has an autosomal recessive condition, familial recurrent hydatidiform moles (FRHM), that predisposes them to molar pregnancies | * '''Risk of recurrent molar pregnancies following complete and partial hydatidiform moles'''<ref name="PMID26202916"><pubmed>26202916</pubmed></ref> "What is the risk of further molar pregnancies for women with one or more hydatidiform moles (HM) in relation to molar subtype. SUMMARY ANSWER: Women with a complete hydatidiform mole (CM) have a 1 in 100 and 1 in 4 risk of further CM after one or two consecutive CM, respectively, while women with a partial hydatidiform mole (PM) have only a small increase in risk for further molar pregnancies. WHAT IS KNOWN ALREADY: Women with a molar pregnancy have an increased risk of further HM. A small subgroup of women with recurrent HM has an autosomal recessive condition, familial recurrent hydatidiform moles (FRHM), that predisposes them to molar pregnancies." | ||
* '''NLRP7, Involved in Hydatidiform Molar Pregnancy (HYDM1), Interacts with the Transcriptional Repressor ZBTB16'''<ref name="PMID26121690"><pubmed>26121690</pubmed>| [http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0130416 PLoS One.]</ref> "Mutations in the maternal effect gene NLRP7 cause biparental hydatidiform mole (HYDM1). HYDM1 is characterized by abnormal growth of placenta and lack of proper embryonic development. The molar tissues are characterized by abnormal methylation patterns at differentially methylated regions (DMRs) of imprinted genes. It is not known whether this occurs before or after fertilization, but the high specificity of this defect to the maternal allele indicates a possible maternal germ line-specific effect. ...Hence, the biological significance of the NLRP7-ZBTB16 interaction remains to be revealed. However, a clear effect of harvesting ZBTB16 to the cytoplasm when the NLRP7 protein is overexpressed may be linked to the pathology of the molar pregnancy disease." [[Molecular Development - Epigenetics]] | * '''NLRP7, Involved in Hydatidiform Molar Pregnancy (HYDM1), Interacts with the Transcriptional Repressor ZBTB16'''<ref name="PMID26121690"><pubmed>26121690</pubmed>| [http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0130416 PLoS One.]</ref> "Mutations in the maternal effect gene NLRP7 cause biparental hydatidiform mole (HYDM1). HYDM1 is characterized by abnormal growth of placenta and lack of proper embryonic development. The molar tissues are characterized by abnormal methylation patterns at differentially methylated regions (DMRs) of imprinted genes. It is not known whether this occurs before or after fertilization, but the high specificity of this defect to the maternal allele indicates a possible maternal germ line-specific effect. ...Hence, the biological significance of the NLRP7-ZBTB16 interaction remains to be revealed. However, a clear effect of harvesting ZBTB16 to the cytoplasm when the NLRP7 protein is overexpressed may be linked to the pathology of the molar pregnancy disease." [[Molecular Development - Epigenetics]] | ||
* '''Minimally-aggressive gestational trophoblastic neoplasms'''<ref name="PMID22198244"><pubmed>22198244</pubmed></ref> "We have previously defined a new syndrome "Minimally-aggressive gestational trophoblastic neoplasms" in which choriocarcinoma or persistent hydatidiform mole has a minimal growth rate and becomes chemorefractory. Previously we described a new treatment protocol, waiting for hCG rise to >3000 mIU/ml and disease becomes more advanced, then using combination chemotherapy. Initially we found this treatment successful in 8 of 8 cases, here we find this protocol appropriate in a further 16 cases. Initially we used hyperglycosylated hCG, a limited availability test, to identify this syndrome. Here we propose also using hCG doubling rate to detect this syndrome." | * '''Minimally-aggressive gestational trophoblastic neoplasms'''<ref name="PMID22198244"><pubmed>22198244</pubmed></ref> "We have previously defined a new syndrome "Minimally-aggressive gestational trophoblastic neoplasms" in which choriocarcinoma or persistent hydatidiform mole has a minimal growth rate and becomes chemorefractory. Previously we described a new treatment protocol, waiting for hCG rise to >3000 mIU/ml and disease becomes more advanced, then using combination chemotherapy. Initially we found this treatment successful in 8 of 8 cases, here we find this protocol appropriate in a further 16 cases. Initially we used hyperglycosylated hCG, a limited availability test, to identify this syndrome. Here we propose also using hCG doubling rate to detect this syndrome." | ||
Revision as of 12:50, 3 August 2015
| Embryology - 16 Apr 2024 |
|---|
| Google Translate - select your language from the list shown below (this will open a new external page) |
|
العربية | català | 中文 | 中國傳統的 | français | Deutsche | עִברִית | हिंदी | bahasa Indonesia | italiano | 日本語 | 한국어 | မြန်မာ | Pilipino | Polskie | português | ਪੰਜਾਬੀ ਦੇ | Română | русский | Español | Swahili | Svensk | ไทย | Türkçe | اردو | ייִדיש | Tiếng Việt These external translations are automated and may not be accurate. (More? About Translations) |
Introduction
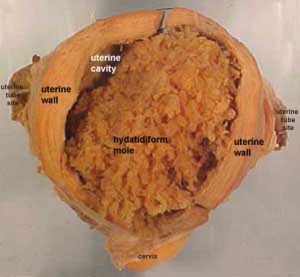
(hydatiform mole, hydatid mole, molar pregnancy, gestational trophoblastic disease) A type of fertilisation abnormality, when only the conceptus trophoblast layers proliferates and not the embryoblast, no embryo develops, this is called a "hydatidiform mole". Due to the continuing presence of the trophoblastic layer, this abnormal conceptus can also implant in the uterus or ectopically. The trophoblast cells will secrete human chorionic gonadotropin (hCG), as in a normal pregnancy, and may appear maternally and by pregnancy test to be "normal". Prenatal diagnosis by ultrasound analysis demonstrates the absence of a embryo.
There are several forms of hydatidiform mole: partial mole, complete mole and persistent gestational trophoblastic tumor. Many of these tumours arise from a haploid sperm fertilizing an egg without a female pronucleus (the alternative form, an embryo without sperm contribution, is called parthenogenesis). The tumour has a "grape-like" placental appearance without enclosed embryo formation. Following a first molar pregnancy, there is approximately a 1% risk of a second molar pregnancy.
- The incidence of hydatidiform mole varies between ethnic groups, and typically occurs in 1 in every 1500 pregnancies.
- All hydatidiform mole cases are sporadic, except for extremely rare familial cases.
- A maternal gene has been identified for recurrent hydatidiform mole (chromosome 19q13.3-13.4 in a 15.2 cM interval flanked by D19S924 and D19S890).[1]
- Links: Hydatidiform Mole | Fertilization | Meiosis | Oocyte Development | Week 2 - Abnormalities | Placenta - Abnormalities | Abnormal Development
Some Recent Findings
|
| More recent papers |
|---|
|
This table allows an automated computer search of the external PubMed database using the listed "Search term" text link.
More? References | Discussion Page | Journal Searches | 2019 References | 2020 References Search term: Hydatidiform Mole <pubmed limit=5>Hydatidiform Mole</pubmed> |
Mole Types

Complete Mole
Only paternal chromosomes.
- Chromosomal genetic material from the ovum (egg) is lost, by an unknown process.
- Fertilization then occurs with one or two sperm and an androgenic (from the male only) conceptus (fertilized egg) is formed.
- With this conceptus the embryo (fetus, baby) does not develop at all but the placenta does grow.
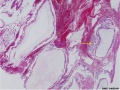
- placenta it is abnormal and forms lots of cysts and has no blood vessels.
- These cysts look like a cluster of grapes and that is why it is called a hydatidiform ("grape-like") mole.
- A hydatidiform mole miscarries by about 16 to 18 weeks gestational age.
- Since the diagnosis can be made by ultrasound before that time, it is better to have an evacuation of the uterus (D & C) so that there is no undue bleeding and no infection.
- Human chorionic gonadotropin (hCG) levels will assist in making the diagnosis.
Partial Mole
Three sets of chromosomes instead of the usual two and this is called triploidy.
- chromosomal (genetic) material from the ovum (egg) is retained and the egg is fertilized by one or two sperm.
- with partial mole there are maternal chromosomes and there is a fetus.
- the three sets of chromosomes means the fetus is always grossly abnormal and will not survive.
(Text modified from: International Society for the Study of Trophoblastic Diseases, see also JRM Gestational Trophoblastic Disease)
Tumour Growth
Like any tumour, unless removed there is a risk of progression:
- Stage I: Tumor confined to uterus (non-metastatic)
- Stage II: Tumor involving pelvic organs and/or vagina
- Stage III: Tumor involving lungs, with or without involving pelvic structures and/or vagina
- Stage IV: Tumor involving distant organs
Choriocarcinoma
A highly malignant epithelial tumour often associated with hydatidiform mole.
Placental Mesenchymal Dysplasia
A rare disorder due to a similar "grape-like" placental appearance, this rare disorder has been mistaken both clinically and macroscopically for a partial hydatidiform molar pregnancy. Characterized by an increased size placenta with cystic villi and dilated vessels. This disorder also has a high incidence of intrauterine growth restriction (IUGR) and fetal death.
Twin Pregnancy Mole
Hydatidiform mole and co-existent healthy fetus is a very rare condition with only 30 cases documented in detail in the literature.[7]
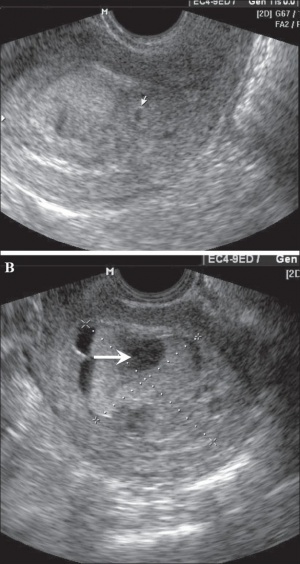
Ectopic Molar Pregnancy
Left-sided unruptured ampullary ectopic pregnancy at laparoscopy.[8]
- Links: Ectopic Implantation
References
Reviews
<pubmed>22085657</pubmed> <pubmed>21293291</pubmed> <pubmed>20367628</pubmed> <pubmed>20673583</pubmed>
Articles
<pubmed></pubmed>
OMIM
Search PubMed
Search PubMed Now: Hydatidiform Mole
Additional Images
Historic Images
| Historic Disclaimer - information about historic embryology pages |
|---|
| Pages where the terms "Historic" (textbooks, papers, people, recommendations) appear on this site, and sections within pages where this disclaimer appears, indicate that the content and scientific understanding are specific to the time of publication. This means that while some scientific descriptions are still accurate, the terminology and interpretation of the developmental mechanisms reflect the understanding at the time of original publication and those of the preceding periods, these terms, interpretations and recommendations may not reflect our current scientific understanding. (More? Embryology History | Historic Embryology Papers) |
External Links
External Links Notice - The dynamic nature of the internet may mean that some of these listed links may no longer function. If the link no longer works search the web with the link text or name. Links to any external commercial sites are provided for information purposes only and should never be considered an endorsement. UNSW Embryology is provided as an educational resource with no clinical information or commercial affiliation.
- PubMed Health Hydatidiform mole
- International Society for the Study of Trophoblastic Diseases
- Sydney Gynaecological Oncology Group Gestational Trophoblastic Disease
- The Journal of Reproductive Medicine Gestational Trophoblastic Disease (1998)
- Dana-Farber Cancer Institute Gynecologic Oncology Program
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 16) Embryology Abnormal Development - Hydatidiform Mole. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/Abnormal_Development_-_Hydatidiform_Mole
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G |