ANAT2241 Female Reproductive System: Difference between revisions
mNo edit summary |
|||
| (5 intermediate revisions by the same user not shown) | |||
| Line 14: | Line 14: | ||
Examine the following virtual slides, and in course manual identify, draw and label the structures listed and note the function. | Examine the following virtual slides, and in course manual identify, draw and label the structures listed and note the function. | ||
Virtual Slides: [https://moodle.telt.unsw.edu.au/mod/book/view.php?id=789982&chapterid=100775 Female Reproductive System] | |||
[ | See also [[ANAT2241_Male_Reproductive_System|Male Reproductive System]] | ||
==Ovary== | |||
The external surface of the ovary has a '''cuboidal epithelium''' (germinal epithelium) overlying a '''dense connective tissue''' layer (tunica albuginea). The outer epithelium is continuous with the peritoneum (serosa) forming a peritoneal fold (mesovarium) between the anterior border of the ovary with the posterior layer of the broad ligament of the uterus. | |||
==Histology== | Ovary structure (regions) | ||
* '''cortex''' - cellular connective tissue containing the developing follicles. | |||
* '''medulla''' - loose connective tissue containing blood vessels, lymphatics and nerves. | |||
===Ovarian Follicle=== | |||
{| | |||
| | |||
Beginning at puberty, the ovarian primordial follicle goes through a number of developmental stages leading to the release of an oocyte at ovulation at about the middle of the menstrual cycle. | |||
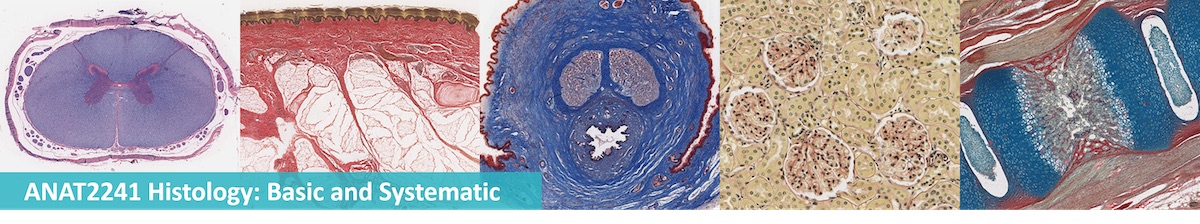
====Primordial Follicle==== | |||
* located in the cortex just beneath tunica albuginea. | |||
* One layer of flattened follicular cells surround the oocyte (about 30 µm in diameter). | |||
* nucleus of the oocyte is positioned eccentric in the cell. It appears very light and contains a prominent nucleolus. | |||
* most organelles of the oocyte aggregate in the centre of the cell, where they form the vitelline body. | |||
====Primary Follicle==== | |||
(preantral) | |||
* first morphological stage that marks the onset of follicular maturation | |||
* previously flattened cell surrounding the oocyte now form a cuboidal or columnar epithelium surrounding the oocyte. | |||
** cytoplasm has a granular appearance, reason also called '''granulosa cells'''. | |||
* continued proliferation of these cells will result in the formation of a stratified epithelium (with a distinct basement membrane) surrounding the oocyte. | |||
* '''zona pellucida''' becomes visible. | |||
** extracellular matrix formed by glycoproteins between interdigitating processes of oocyte and granulosa cells. | |||
* parenchymal cells of the ovary surrounding the growing follicle become organised in concentric sheaths, the '''theca folliculi'''. | |||
| [[File:Ovary follicle 01.jpg|400px]] | |||
|- | |||
| | |||
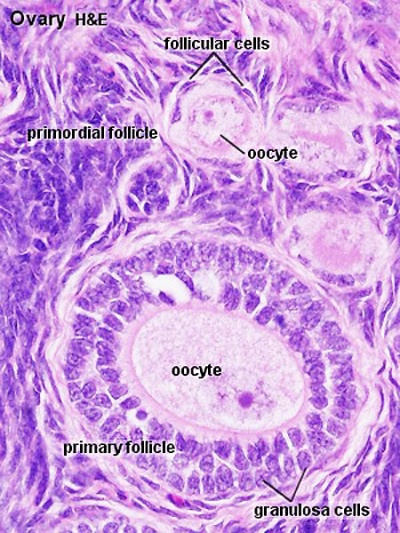
====Secondary Follicle==== | |||
(antral) | |||
* small fluid-filled spaces become visible between the granulosa cells as the follicle reaches a diameter of about 400 µm. | |||
* spaces enlarge and fuse to form the '''follicular antrum''' | |||
** defining feature of the secondary follicle. | |||
* oocyte is now located on one wall of the follicle in the '''cumulus oophorus'''. | |||
* theca folliculi differentiates to form 2 layers the '''theca interna''' and a '''theca externa''' | |||
** theca interna - spindle-shaped or polyhedral cells start to produce estrogens (also increased vascularization). | |||
** theca externa - highly cellular connective tissue with smooth muscle cells. | |||
* oocyte of the secondary follicle reaches a diameter of about 125 µm. | |||
* follicle itself reaches a diameter of about 10-15 mm. | |||
====Preovulatory Follicle==== | |||
(Graafian, tertiary, mature follicle) | |||
* increases further in size (in particular in the last 12h before ovulation). | |||
* '''stigma''' (macula pellucida) ovarian surface swelling formed by enlarging follicle. | |||
** thinning of the capsule, progressive restriction of the blood flow. | |||
* prior to ovulation the cumulus oophorus separates from the follicular wall. | |||
* oocyte floats freely in the follicular antrum, follicular fluid. | |||
** still surrounded by granulosa cells which form the corona radiata. | |||
* '''Ovulation''' - follicle ruptures at the stigma, oocyte, supporting cells and follicular fluid released from the ovary. | |||
| [[File:Ova20he.jpg|400px]] | |||
|} | |||
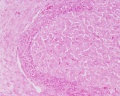
===Corpus Luteum=== | |||
{| | |||
| | |||
* Cells work together in the production of ovarian hormones that support the initial pregnancy. | |||
* Initial growth of the corpus luteum requires leutenizing hormone ( LH) from the adenohypophysis. | |||
* Later growth of the corpus luteum requires human chorionic gonadotrophin (hCG) from the implanting conceptus (trophoblast cells). | |||
* Progesterone is synthesized from cholesterol by both the large and small luteal cells upon luteal maturation. | |||
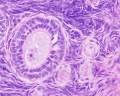
====Theca Lutein Cells==== | |||
* the darker stained cells. | |||
* derived from the theca interna of the original follicle. | |||
* lack microvilli on the surface. | |||
* lack the aromatase enzyme. | |||
* produce androgens for the granulosa lutein cells to convert. | |||
====Granulosa Lutein Cells==== | |||
* the lighter stained cells. | |||
* derived from the granulosa cells of the original follicle. | |||
* contain aromatase enzyme. | |||
* produce estrogen and progesterone from the androgens produced by the theca lutein cells. | |||
<gallery> | |||
Ovary corpus luteum.jpg|ovary overview | |||
File:Corpus luteum.jpg|low power | |||
File:Ovary_histology_002.jpg|theca and granulosa lutein cells | |||
</gallery> | |||
{{Corpus luteum links}} | |||
| [[File:Corpus_luteum_lutein_cells.jpg|400px]] | |||
|} | |||
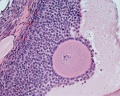
===Corpus Albicans=== | |||
[[File:Ovary_histology_003.jpg|corpus albicans|thumb|corpus albicans]] | |||
Hormone secretion in the corpus luteum ceases within 14 days after ovulation if the oocyte is not fertilised. In this case, the corpus luteum degenerates into a corpus albicans - whitish scar tissue within the ovaries. | |||
===Ovary Histology=== | |||
<gallery> | |||
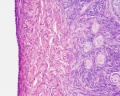
File:Ovary_histology_007.jpg|Tunica Albuginea x20 | |||
File:Ovary_histology_008.jpg|Tunica albuginea, Germinal epithelium x40 | |||
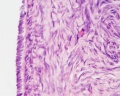
File:Ovary_histology_005.jpg|Primary follicle, primordial follicle, oocyte, x40 | |||
File:Ovary_histology_006.jpg|Secondary follicle, cumulus oophorus, zona pelucida, granulosa cells, oocyte x20 | |||
File:Ovary_histology_004.jpg|Corpus luteum, theca lutein cells, granulosa lutein cells, Loupe | |||
File:Ovary_histology_001.jpg|Corpus luteum, theca lutein cells, granulosa lutein cells, x10 | |||
File:Ovary_histology_002.jpg|Corpus luteum, theca lutein cells, granulosa lutein cells, x40 | |||
File:Ovary_histology_003.jpg|Corpus albicans, primary follicle, primordial follicle, granulosa cells, oocyte x20 | |||
</gallery> | |||
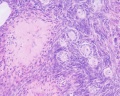
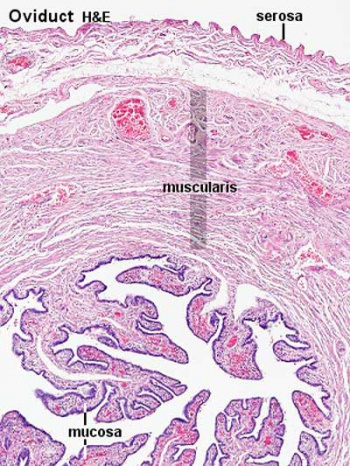
==Uterine Tube== | |||
(oviduct, Fallopian tube) | |||
* uterine tube acts as a conduit for the oocyte, from the ovaries to the uterus. | |||
* consists of a mucosa and a muscularis. | |||
* peritoneal surface of the oviduct is lined by a serosa and subjacent connective tissue. | |||
{| | |||
! Overview | |||
! Mucosa | |||
|- | |||
| [[File:Uterine_tube_histology_02.jpg|350px]] | |||
| [[File:Uterine_tube_histology_03.jpg|350px]] | |||
|- | |||
| width=350px| | |||
===Muscularis=== | |||
* inner circular muscle layer and an outer longitudinal layer. | |||
* inner longitudinal layer is present in the isthmus and the intramural part. | |||
* peristaltic muscle action for the transport of spermatozoa and oocyte. | |||
| width=350px| | |||
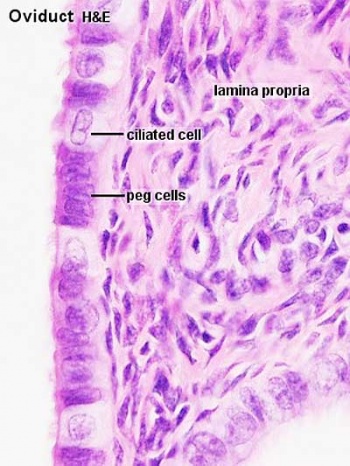
===Mucosa=== | |||
* ciliated and secretory epithelium resting on a cellular lamina propria. | |||
* number of ciliated cells and secretory cells varies along the tube. | |||
* secretory activity varies during the menstrual cycle, and resting secretory cells are also referred to as peg-cells. Some of the secreted substances are thought to nourish the oocyte and the very early embryo. | |||
|} | |||
===Tube Regions=== | |||
[[File:Week1_001_icon.jpg|800px]] | |||
{| | |||
! infundibulum | |||
! ampulla | |||
! isthmus | |||
! intramural | |||
|- | |||
| width=150px valign=top| funnel-shaped (up to 10 mm in diameter) end of the oviduct. Finger-like extensions of its margins, the fimbriae, are closely applied to the ovary. Ciliated cells are frequent. | |||
| width=150px valign=top| mucosal folds, or plicae, and secondary folds which arise from the plicae divide the lumen of the ampulla into a very complex shape. Fertilization usually takes place in the ampulla. | |||
| width=250px valign=top| narrowest portion (2-3 mm in diameter) of the tube located in the peritoneal cavity. Mucosal folds are less complex and the muscularis is thick. An inner, longitudinal layer of muscle is present in the isthmus. | |||
| width=150px valign=top| penetrates the wall of the uterus. The mucosa is smooth, and the inner diameter of the duct is very small. | |||
|} | |||
==Uterus== | |||
* parts - body (upper two-thirds) and cervix. | |||
* walls - mucosal layer, the endometrium, and a fibromuscular layer, the myometrium. | |||
* peritoneal surface of the uterus is covered by a serosa. | |||
===Myometrium=== | |||
* smooth muscle fibres form several layers with preferred orientations. | |||
* muscular tissue hypertrophies during pregnancy. | |||
* GAP-junctions between cells become more frequent. | |||
===Endometrium=== | |||
* simple columnar epithelium (ciliated cells and secretory cells) and an underlying thick connective tissue stroma. | |||
* mucosa is invaginated to form many simple tubular uterine glands. | |||
** glands extend through the entire thickness of the stroma. | |||
* stromal cells of the endometrium are embedded in a network of reticular fibres. | |||
===Menstrual cycle=== | |||
* hormones alter the endometrium. | |||
* only the uterus body mucosa takes part in the menstrual cycle. | |||
* endometrial layers (based on changes) | |||
# basalis - remains during menstruation, functions as a regenerative zone for the functionalis. | |||
# functionalis - lost during menstruation, functions as the site of cyclic changes in the endometrium. | |||
<gallery> | |||
File:Uterus proliferative phase.jpg|Proliferative phase | |||
File:Uterine_gland_proliferative_phase.jpg|Gland - proliferative phase | |||
File:Uterus_secretory_phase.jpg|Secretory phase | |||
File:Uterine_gland_secretory_phase.jpg|Gland - secretory phase | |||
</gallery> | |||
{{Uterus_Histology}} | |||
:'''Links:''' [[Menstrual Cycle - Histology]] | |||
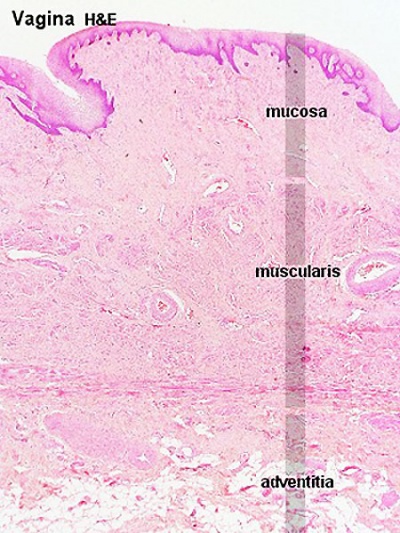
==Vagina== | |||
{| | |||
| valigh=top|The wall of the vagina fibromuscular tube consists of 3 layers: | |||
# mucosa | |||
# muscularis | |||
# adventitia | |||
===Mucosa=== | |||
* stratified squamous epithelium | |||
** deep stratum basalis, intermediate stratum spinosum, superficial layers of flat eosinophilic cells | |||
** rests on a cellular lamina propria (many leukocytes). | |||
* towards the muscularis some vascular cavernous spaces may be seen (erectile tissue). | |||
===Muscularis=== | |||
* inner circular and outer longitudinal layers of smooth muscle | |||
* '''bulbospongiosus muscle''' - (striated) forms an inferior sphincter around the vagina | |||
===Adventitia=== | |||
* adventitia bordering the muscularis is fairly dense and contains many elastic fibres. | |||
* outer part of the adventitia loose connective tissue with a prominent venous plexus. | |||
| [[File:Vagina_histology_01.jpg|400px]] | |||
|} | |||
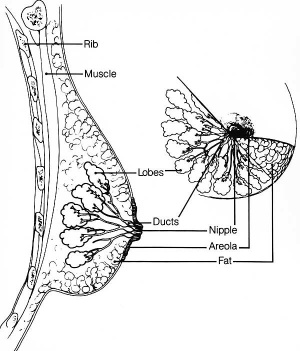
==Mammary Gland== | |||
[[File:Mammary_anatomy.jpg|thumb|Adult female mammary anatomy cartoon]] | |||
The mammary glands are modified glands of the skin and their development is similar to that of sweat glands. | |||
* compound branched alveolar glands, secretory unit is the '''alveolus''' | |||
* consist of 15-25 lobes separated by dense interlobar connective tissue and fat. | |||
* each lobe contains an individual gland. | |||
* lactiferous duct - excretory duct of each lobe with own opening on the nipple. | |||
===Alveolus=== | |||
* inner layer of cuboidal '''secretory epithelial cells''' | |||
** merocrine secretion, protein micelles are release by exocytosis. | |||
* outer layer of '''myoepithelial cells''' | |||
** located between the secretory cells and the surrounding basal lamina. | |||
** contraction helps force the milk from the secretory alveoli into the ducts. | |||
Note - plasma cells in the stroma also secrete antibodies (dimeric IgA) and released into the milk, to provides passive immunity to the suckling young. | |||
{| | |||
! lactiferous duct | |||
! lactating mammary gland | |||
|- | |||
| [[File:Lactiferous_duct_01.jpg|300px]] | |||
| [[File:Mammary_gland_01.jpg|300px]] | |||
|} | |||
:'''Links:''' [[Integumentary_System_-_Mammary_Gland_Development|Mammary Gland Development]] | [[Normal_Development_-_Milk|Milk]] | |||
==Terms== | |||
* '''corona radiata''' - layer of cells of cumulus oophorus remaining attached to zona pellucida of oocyte after ovulation. | |||
* '''corpus''' - (Latin, ''corpus'' = body). | |||
* '''corpus albicans''' - (Latin, ''corpus'' = body + ''albicans'' = "whitish") a degenerating corpus luteum in the ovary. | |||
* '''corpus luteum''' - (Latin, ''corpus'' = body + ''luteum'' = yellow) major endocrine organ which is the remains of ovarian follicle after ovulation; yellow in ovary of cow where de Graaf (q.v.) first saw it. | |||
* '''cortex''' - (Latin = rind, or bark) outer layer of an organ. | |||
* '''cumulus oophorus''' - (Latin = ''cumulus'' = a little mound + Greek ''oon'' = egg + ''phorus'' = bearing) part of the wall of an ovarian follicle surrounding and carrying the oocyte. | |||
* '''fimbria''' - (Latin, ''fimbria'' = a fringe) the fringed open ovarian end of the uterine tube. | |||
* '''follicle''' - (Latin, ''folliculus'' = little bag). | |||
* '''hilum''' - or hilus (Latin,= a trifle; depression in a seed) a depression at vascular entrance/exit of a gland or organ. | |||
* '''mesovarium''' - short peritoneal fold connecting the anterior border of the ovary with the posterior layer of the broad ligament of the uterus. | |||
* '''medulla''' - (Latin, ''medulla'' = pith, marrow) the inner portion of an organ, in contrast to cortex. | |||
* '''menstrual''' - (Latin, ''menstruus'' = monthly) relating to the monthly female sexual cycle. | |||
* '''mucosa''' - (Latin, = mucous membrane) thin layer which lines body cavities and passages formed by epithelium and lamina propria. | |||
* '''oocyte''' - (Greek, ''öon'' = egg + ''kytos'' = hollow vessel (cell) the female germ cell in the ovary. | |||
* '''parenchyma''' - (Greek," + enkeim = to pour in) the essential functional cells of an organ as opposed to its stroma. | |||
* '''salpinx''' - (Greek, = a trumpet) the uterine tube. | |||
* '''serosa''' - (Latin, ''serum'' = whey; a pale fluid) a serous membrane lining body cavities. | |||
* '''stroma''' - (Greek, = a cover, table-cloth, bedding) term for the internal supporting frame-work of a tissue, or organ, as opposed to its parenchyma. | |||
* '''tunica albuginea''' - a dense, white, fibrous sheath enclosing a part or organ. | |||
* '''uterine tube''' - (oviduct, Fallopian tube) | |||
* '''uterus''' - (Latin, = womb, from ''uter'' = a large goatskin bag used as a wine-skin). | |||
* '''zona pellucida''' - (Latin, ''zona'' = a girdle + ''perlucere'' = to shine through) the refractile layer of glycoclayx (ECM) surrounding oocyte in a growing ovarian follicle. | |||
---- | |||
:'''Links:''' [[Genital_-_Female_Development|Female]] | [[Ovary Development|Ovary]] | [[Oocyte Development|Oocyte]] | [[Uterus Development|Uterus]] | [[Vagina Development|Vagina]] | |||
{{Histology Glossary}} | |||
===Ovary Histology=== | ===Ovary Histology=== | ||
Latest revision as of 08:45, 9 August 2019
| ANAT2241 This practical support page content is not part of the virtual science practical class and provides additional information for student self-directed learning purposes. All practical class pages are located on Moodle - ANAT2241 |
General Objective
To know the histological and cytological structure of the major organs of the female reproductive system.
Specific Objectives
- To describe the microanatomy of the ovary and to identify: peritoneal mesothelium, developing ovarian follicles, Graafian and atretic follicles.
- To know the layers of the wall of the uterine tube (Fallopian tube or oviduct).
- To know the structure of the uterus and the morphological changes of the endometrium during the menstrual cycle.
- To know the structure of the mammary glands.
Learning Activities
Examine the following virtual slides, and in course manual identify, draw and label the structures listed and note the function.
Virtual Slides: Female Reproductive System
See also Male Reproductive System
Ovary
The external surface of the ovary has a cuboidal epithelium (germinal epithelium) overlying a dense connective tissue layer (tunica albuginea). The outer epithelium is continuous with the peritoneum (serosa) forming a peritoneal fold (mesovarium) between the anterior border of the ovary with the posterior layer of the broad ligament of the uterus.
Ovary structure (regions)
- cortex - cellular connective tissue containing the developing follicles.
- medulla - loose connective tissue containing blood vessels, lymphatics and nerves.
Ovarian Follicle
Corpus Luteum
Theca Lutein Cells
Granulosa Lutein Cells
|

|
Corpus Albicans
Hormone secretion in the corpus luteum ceases within 14 days after ovulation if the oocyte is not fertilised. In this case, the corpus luteum degenerates into a corpus albicans - whitish scar tissue within the ovaries.
Ovary Histology
Uterine Tube
(oviduct, Fallopian tube)
- uterine tube acts as a conduit for the oocyte, from the ovaries to the uterus.
- consists of a mucosa and a muscularis.
- peritoneal surface of the oviduct is lined by a serosa and subjacent connective tissue.
Tube Regions
| infundibulum | ampulla | isthmus | intramural |
|---|---|---|---|
| funnel-shaped (up to 10 mm in diameter) end of the oviduct. Finger-like extensions of its margins, the fimbriae, are closely applied to the ovary. Ciliated cells are frequent. | mucosal folds, or plicae, and secondary folds which arise from the plicae divide the lumen of the ampulla into a very complex shape. Fertilization usually takes place in the ampulla. | narrowest portion (2-3 mm in diameter) of the tube located in the peritoneal cavity. Mucosal folds are less complex and the muscularis is thick. An inner, longitudinal layer of muscle is present in the isthmus. | penetrates the wall of the uterus. The mucosa is smooth, and the inner diameter of the duct is very small. |
Uterus
- parts - body (upper two-thirds) and cervix.
- walls - mucosal layer, the endometrium, and a fibromuscular layer, the myometrium.
- peritoneal surface of the uterus is covered by a serosa.
Myometrium
- smooth muscle fibres form several layers with preferred orientations.
- muscular tissue hypertrophies during pregnancy.
- GAP-junctions between cells become more frequent.
Endometrium
- simple columnar epithelium (ciliated cells and secretory cells) and an underlying thick connective tissue stroma.
- mucosa is invaginated to form many simple tubular uterine glands.
- glands extend through the entire thickness of the stroma.
- stromal cells of the endometrium are embedded in a network of reticular fibres.
Menstrual cycle
- hormones alter the endometrium.
- only the uterus body mucosa takes part in the menstrual cycle.
- endometrial layers (based on changes)
- basalis - remains during menstruation, functions as a regenerative zone for the functionalis.
- functionalis - lost during menstruation, functions as the site of cyclic changes in the endometrium.
- Uterus Histology Links: Labeled - proliferative phase | Labeled - gland proliferative phase | Labeled - secretory phase | Unlabeled - secretory phase | Unlabeled - late secretory phase | Labeled - gland secretory phase | Menstrual Cycle | Uterine Gland | Uterus Development
- Links: Menstrual Cycle - Histology
Vagina
Mammary Gland
The mammary glands are modified glands of the skin and their development is similar to that of sweat glands.
- compound branched alveolar glands, secretory unit is the alveolus
- consist of 15-25 lobes separated by dense interlobar connective tissue and fat.
- each lobe contains an individual gland.
- lactiferous duct - excretory duct of each lobe with own opening on the nipple.
Alveolus
- inner layer of cuboidal secretory epithelial cells
- merocrine secretion, protein micelles are release by exocytosis.
- outer layer of myoepithelial cells
- located between the secretory cells and the surrounding basal lamina.
- contraction helps force the milk from the secretory alveoli into the ducts.
Note - plasma cells in the stroma also secrete antibodies (dimeric IgA) and released into the milk, to provides passive immunity to the suckling young.
| lactiferous duct | lactating mammary gland |
|---|---|

|

|
- Links: Mammary Gland Development | Milk
Terms
- corona radiata - layer of cells of cumulus oophorus remaining attached to zona pellucida of oocyte after ovulation.
- corpus - (Latin, corpus = body).
- corpus albicans - (Latin, corpus = body + albicans = "whitish") a degenerating corpus luteum in the ovary.
- corpus luteum - (Latin, corpus = body + luteum = yellow) major endocrine organ which is the remains of ovarian follicle after ovulation; yellow in ovary of cow where de Graaf (q.v.) first saw it.
- cortex - (Latin = rind, or bark) outer layer of an organ.
- cumulus oophorus - (Latin = cumulus = a little mound + Greek oon = egg + phorus = bearing) part of the wall of an ovarian follicle surrounding and carrying the oocyte.
- fimbria - (Latin, fimbria = a fringe) the fringed open ovarian end of the uterine tube.
- follicle - (Latin, folliculus = little bag).
- hilum - or hilus (Latin,= a trifle; depression in a seed) a depression at vascular entrance/exit of a gland or organ.
- mesovarium - short peritoneal fold connecting the anterior border of the ovary with the posterior layer of the broad ligament of the uterus.
- medulla - (Latin, medulla = pith, marrow) the inner portion of an organ, in contrast to cortex.
- menstrual - (Latin, menstruus = monthly) relating to the monthly female sexual cycle.
- mucosa - (Latin, = mucous membrane) thin layer which lines body cavities and passages formed by epithelium and lamina propria.
- oocyte - (Greek, öon = egg + kytos = hollow vessel (cell) the female germ cell in the ovary.
- parenchyma - (Greek," + enkeim = to pour in) the essential functional cells of an organ as opposed to its stroma.
- salpinx - (Greek, = a trumpet) the uterine tube.
- serosa - (Latin, serum = whey; a pale fluid) a serous membrane lining body cavities.
- stroma - (Greek, = a cover, table-cloth, bedding) term for the internal supporting frame-work of a tissue, or organ, as opposed to its parenchyma.
- tunica albuginea - a dense, white, fibrous sheath enclosing a part or organ.
- uterine tube - (oviduct, Fallopian tube)
- uterus - (Latin, = womb, from uter = a large goatskin bag used as a wine-skin).
- zona pellucida - (Latin, zona = a girdle + perlucere = to shine through) the refractile layer of glycoclayx (ECM) surrounding oocyte in a growing ovarian follicle.
- Histology Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | ANAT2241 Support | Histology | Histology Stains | Embryology Glossary
Ovary Histology
Ovary histology: Tunica Albuginea x20 | Tunica albuginea, Germinal epithelium x40 |
Primary follicle, primordial follicle, oocyte, x40 | Secondary follicle, cumulus oophorus, zona pelucida, granulosa cells, oocyte x20 | Corpus luteum, theca lutein cells, granulosa lutein cells, Loupe | Corpus luteum, theca lutein cells, granulosa lutein cells, x10 | Corpus luteum, theca lutein cells, granulosa lutein cells, x40 | Corpus albicans, primary follicle, primordial follicle, granulosa cells, oocyte x20 | Menstrual Cycle | Ovary Development
Menstrual Histology
Menstrual Cycle - Histology (images are listed in sequence and uterine endometrium from dilatation and curettage)
- Uterine Endometrium: menstrual | mid-proliferative | late proliferative | secretory | late secretory
- Vaginal Smear: early proliferative | mid-proliferative | late proliferative | secretory | late secretory
Links: Menstrual Cycle - Histology | Menstrual Cycle | Papanicolaou stain
Course Links
- Histology Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | ANAT2241 Support | Histology | Histology Stains | Embryology Glossary
| Common Histology Stains | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Practical Support
- Pages can be accessed from any internet connected computer.
ANAT2241 Support Links: The Virtual Microscope | Covering and Lining Epithelia | Glandular Epithelia | CT Components | CT Types | Bone, Bone Formation and Joints | Muscle | Nervous | Blood | Eye | Cardiovascular | Respiratory | Integumentary | Gastrointestinal | Gastrointestinal Organs | Lymphatic and Immune | Endocrine | Urinary | Female Reproductive | Male Reproductive | Histology Stains | Histology Drawings | Practicals Health and Safety 2013 | Moodle - 2019
ANAT2241 This practical support page content is not part of the science practical class and provides only background information for student self-directed learning purposes.
Cite this page: Hill, M.A. (2024, April 18) Embryology ANAT2241 Female Reproductive System. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/ANAT2241_Female_Reproductive_System
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G