2011 Lab 8 - Postnatal: Difference between revisions
(Created page with "{{2011Lab8}} {{2011Lab8}} {{Glossary}} {{Footer}}") |
|||
| (5 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{2011Lab8}} | {{2011Lab8}} | ||
==Introduction== | |||
This section gives a very brief overview of genital postnatal changes that occur in neonatal, childhood and through to puberty. For sexual development at puberty, we will use resources available online from '''Endocrinology: An Integrated Approach''' (NCBI Bookshelf). | |||
==Newborn== | |||
{| | |||
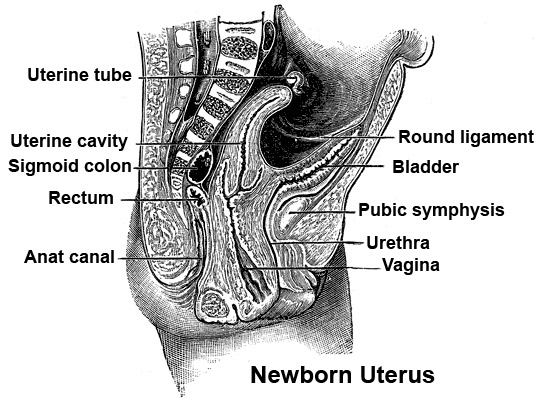
| [[File:Newborn_uterus.jpg]] | |||
Newborn uterus anatomy | |||
| | |||
* Female tract abnormalities tend to be rarer and when they do occur are also more difficult to detect. | |||
* Male abnormalities are more likely and easily detected asociated with fusion of the urogenital folds, undescended testes or hernia. | |||
* This topic will be discussed on the next abnormalities will be discussed in detail on the next page. | |||
|- | |||
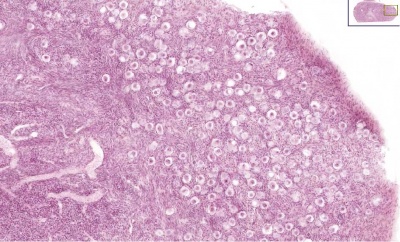
| [[File:Infant_ovary.jpg|400px]] | |||
| * Ovary - Primordial follicle numbers are highest late fetal to around birth (estimated 2.5 - 7 million) and then decreasing by apopotic cell death. | |||
* At puberty there remain only about 400,000 and only about 10% of these will be released through reproductive life. | |||
(Based on data from: Hassold, etal., Environ Mol Mutagen 1996. 28: 167-175) | |||
|} | |||
==Puberty== | |||
{| | |||
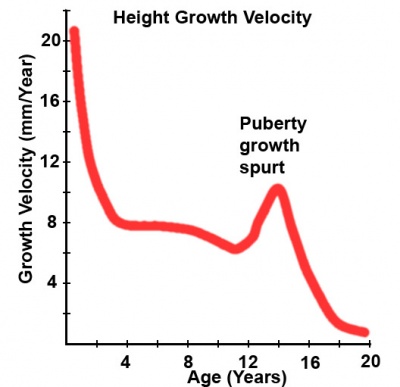
| [[File:Puberty growth.jpg|400px]] | |||
| Latin, ''pubertas'' = "adulthood" | |||
In the teen years the endocrine changes that signal sexual development trigger changes in primary sex organs and the development of secondary sexual characteristics. | |||
* Hypothalamic expression of gonadotropin releasing hormone (GnRH) is a known puberty trigger. | |||
* Recent research suggests that an earlier signal could come from increased neuronal and hypothalamic expression of a peptide family (kisspeptins) and their receptor (G protein-coupled receptor GPR54) in the hypothalamus. | |||
* GnRH then signals the pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH) to start sexual development. | |||
Puberty can occur over a broad range of time and differently for each sex: | |||
* '''girls''' - age 7 to 13 | |||
* '''boys''' - age 9 to 15 | |||
* Early onset of puberty (precocious) occurs more frequently in girls than boys, in contrast late onset (delayed) occurs more frquently in boys than girls. | |||
* The physical characteristics that can be generally measured are: genital stage, pubic hair, axillary hair, menarche, breast, voice change and facial hair. | |||
* In 1976, Tanner and Whitehouse established a series of descriptive stages (Tanner Stages) for primary and secondary sexual characteristic development at puberty. | |||
'''Study the [http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=endocrin&part=A972&rendertype=box&id=A1059 Tanner stages] comparing the male and female physiological changes.''' | |||
|} | |||
:'''Links:''' [[Puberty Development]] | [http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=endocrin&part=A972&rendertype=box&id=A1059 Tanner stages] | |||
===Female - Hypothalamus Pituitary Gonad (HPG) Axis=== | |||
{| | |||
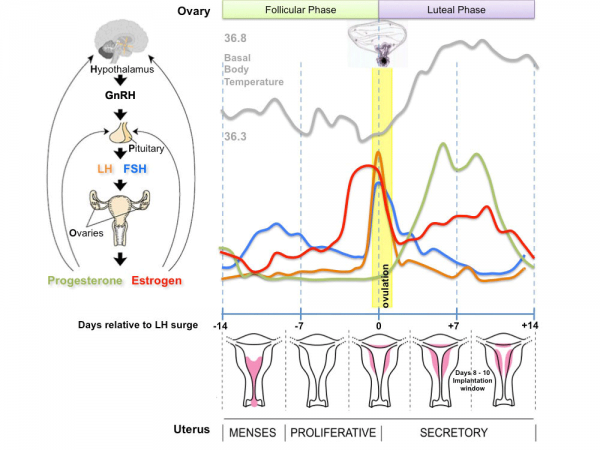
| [[File:Menstrual_cycle.png|600px]] | |||
| | |||
'''Female''' | |||
* '''menarche''' (the first menstruation or a period) usually occurs after the other secondary sex characteristics | |||
* cycles will continue until '''menopause''' (permanent cessation of reproductive fertility). | |||
* The diagram shows the hormonal regulation pathway from the brain to the ovary and subsequent impact on uterine changes during the menstral cycle. | |||
'''GnRH''' = gonadotropin-releasing hormone (GnRH). This peptide hormone is a decapeptide (10 amino acids) with a short half life (<15 minutes). | |||
'''LH''' = Luteinizing Hormone | |||
'''FSH''' = Follicle Stimulating Hormone | |||
A similar endocrine axis is also found for regulation of the male gonad. | |||
|} | |||
===Male - Testosterone=== | |||
{| | |||
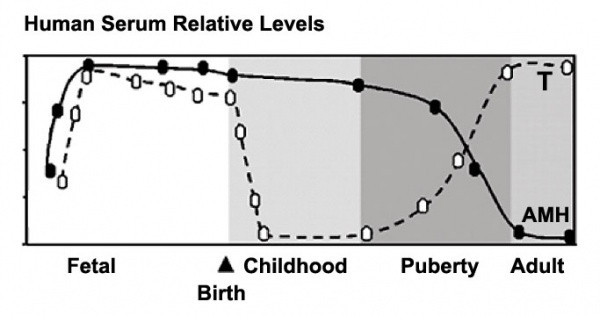
| [[File:Male_testosterone_and_AMH_level_graph.jpg|600px]] | |||
| | |||
'''Male''' | |||
Testosterone and Anti-Müllerian Hormone (AMH) relative levels<ref><pubmed>16544032</pubmed>| [http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0004-27302005000100005&lng=en&nrm=iso&tlng=en Arq Bras Endocrinol Metabol.]</ref> | |||
* Sertoli cells - AMH production. | |||
* Leydig cells - Testosterone production | |||
* Spermatogonia - mitosis | |||
* Spermatozoa - maturation | |||
|} | |||
==Additional Information== | |||
'''Endocrinology: An Integrated Approach.''' Nussey S, Whitehead S. Oxford: BIOS Scientific Publishers; 2001. | |||
* [http://www.ncbi.nlm.nih.gov/books/NBK29/#A1058 Puberty] | |||
* [http://www.ncbi.nlm.nih.gov/books/NBK29/#A1098 Endocrine changes in puberty] | |||
* [http://www.ncbi.nlm.nih.gov/books/NBK29/#A1101 Precocious sexual development] | |||
* [http://www.ncbi.nlm.nih.gov/books/NBK29/#A1104 Delayed puberty] | |||
==References== | |||
<references/> | |||
Latest revision as of 08:45, 22 September 2011
| 2011 Lab 8: Introduction | Sex Determination | Early Embryo | Late Embryo | Fetal | Postnatal | Abnormalities | Quiz | Online Assessment |
Introduction
This section gives a very brief overview of genital postnatal changes that occur in neonatal, childhood and through to puberty. For sexual development at puberty, we will use resources available online from Endocrinology: An Integrated Approach (NCBI Bookshelf).
Newborn
Puberty
|
Latin, pubertas = "adulthood"
In the teen years the endocrine changes that signal sexual development trigger changes in primary sex organs and the development of secondary sexual characteristics.
Puberty can occur over a broad range of time and differently for each sex:
|
- Links: Puberty Development | Tanner stages
Female - Hypothalamus Pituitary Gonad (HPG) Axis
Male - Testosterone
|
Male Testosterone and Anti-Müllerian Hormone (AMH) relative levels[1]
|
Additional Information
Endocrinology: An Integrated Approach. Nussey S, Whitehead S. Oxford: BIOS Scientific Publishers; 2001.
References
- ↑ <pubmed>16544032</pubmed>| Arq Bras Endocrinol Metabol.
| 2011 Lab 8: Introduction | Sex Determination | Early Embryo | Late Embryo | Fetal | Postnatal | Abnormalities | Quiz | Online Assessment |
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
Cite this page: Hill, M.A. (2024, April 19) Embryology 2011 Lab 8 - Postnatal. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2011_Lab_8_-_Postnatal
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G