2011 Group Project 6
| Note - This page is an undergraduate science embryology student group project 2011. |
Tetralogy of Fallot
--Mark Hill 15:50, 8 September 2011 (EST) This has reasonable sub-heading structure, but several sections still lack any content, which they should by now. There are only 2 figures and the text in places is verbose, and very poorly structured for ease of reading/understanding.
- Introduction - No text here? This is where the reader starts and it should grab their attention to your topic.
- History - Good early background. Quoted text should be indented. You have included only a few time points in the disease up to 1945-50's and only broadly thereafter. The text is also very clinically technical, suggesting that you have just copied without understanding the content itself.
- Signs and Symptoms - this should have subsections for each description.
- Genetics/Aetiology - No text here?
- Pathophysiology and Abnormalities - Seems to overlap with the Signs and Symptoms content.
- Diagnostic Tests - you name the tests but do not describe how they work or what they show, this could easily be illustrated.
- Treatment/Management - I think this should be far better structured in layout and content.
- Prognosis - No text here?
- Future Directions - No text here?
Introduction
--Mark Hill 15:50, 8 September 2011 (EST) No text here?
History
In 1671, Niels Stenson was the first to describe Tetralogy of Fallot anatomically. However, the precise descriptions of the anatomy of Tetralogy of Fallot was done in 1784 by William Hunter at St Georges Hospital Medical School in London. His description is as follows [1]:
“…the passage from the right ventricle into the pulmonary artery, which should have admitted a finger, was not so wide as a goose quill; and there was a hole in the partition of the two ventricles, large enough to pass the thumb from one to the other. The greatest part of the blood in the right ventricle was driven with that of the left ventricle into the aorta, or great artery, and so lost all the advantage which it ought to have had from breathing”[2]
Hunter’s description of the defected heart’s anatomy along with its resulting physiology was further specified and advanced by Etienne-Louis Fallot. However it was Maude Abbott from Canada who coined the term ‘Tetralogy of Fallot’ in 1924. The first procedures for Tetralogy of Fallot were around from the 1950s. Due the advances in the areas of ‘diagnosis, perioperative and surgical treatment and postoperative care’, children born with Tetralogy of Fallot now have a great chance to survive to adulthood[3]
In retrospective studies it shows how surgical procedures have improved because in the 1950’s to today’s times, the mortality rate from surgery dropped from 50% to less than 2%. It was in 1945 that Blalock and Taussig explained the ‘systemic artery-to-pulmonary artery shunt’ and in 1954 that Varco and Lillehei repaired a TOF heart whilst doing a open-heart surgery.[4]
During such surgeries in the past the surgeons will actually now put a shunt between the pulmonary artery and a systemic artery of a child with Tetralogy of Fallot as this will allow some improvement to the oxygenation of the blood in the infant. It will be later when the individual grows up that the shunt will be removed then the heart will be repaired. Now surgeons prefer to repair the heart in the initial operation to repair the infants heart. [5]
Epidemiology
Tetralogy of Fallot makes up around 7%-10% of Cardiac Congenital Defects as studies show that it occurs in 3 out of 10000 live births that are delivered. After the Neonatal age, Tetralogy of Fallot is the most frequent cause of cyanotic heart disease. Moreover, Tetralogy of Fallot slightly affects more males then females.[6]
From studies conducted in regards to mortality rates in respect to congenital heart disease in the US between 1979-2005, there was a 40% reduction in mortality that was linked to Tetralogy of Fallot. It is thought that this reduction in mortality was associated to the ‘earlier recognition and treatment of heart failure and arrythmia’ which allowed this change to occur.[7]
Signs and Symptoms
The most important sign of TOF patients is Cyanosis. This is when the lips, fingernails and skin of the patient turns into a bluish colour. Sometimes babies who have TOF can enter into ‘tet spells’, in which there is a sudden drop in oxygen saturation of the blood, causing the baby to turn blue. These tets spells become apparent when the baby does certain activities such as crying. In addition to the tet spells the baby could pass out, become unresponsive to their parents calling or touch, can develop fatigue and finally have dyspnoea. Furthermore, children of TOF would develop fatigue quickly and possibly pass out, thus surgeons now repair TOF hearts during infancy and not at adult to prevent such events.[8]
Another common sign of TOF is heart murmur which occurs due to the defected heart’s abnormal blood flow through it. However it should be mentioned that heart murmur is not a hallmark for Congenital Heart Defects as many hearts of healthy children also have murmurs.Furthermore, children of TOF don’t grow at the rate of normal children as whilst breastfeeding in infancy, the babies would get tired quicker and whilst the infant grows up, normal functionability of the heart and oxygen saturated blood is needed for proper growth. Also, TOF children may also have clubbing. [9] This clubbing would be evident as there would be enlargenemt of the bone or the skin around the fingernails of the patient. [10]
It should also be mentioned that pulmonary insufficiency symptoms developed from a TOF heart varies in the degree of pulmonary insufficiency found in that individual. Thus the symptoms that could be presented are of a wide range which could from decline in function to palpitations. Moreover, late symptoms could also develop from the insufficiency which includes right heart failure, exertional dyspnea, syncope and palpitations. In an event of which right ventricular failure occurs, signs to indicate it include elevated jugular venous pressure, ascites, hepatomegaly, jugular venous distension and peripheral edema.[11]
Genetics/Aetiology
--Mark Hill 16:05, 8 September 2011 (EST) No text here?
Pathophysiology and Abnormalities
The four pathological features of tetralogy of fallot are:
- Pulmonary stenosis
- Overriding aorta
- Ventricular septal defect
- Right ventricular hypertrophy
These features result from the disruption of the aortic and pulmonary outflow tracts. The severity of symptoms is determined by the extent of right ventricular outflow obstruction.
- Pulmonary stenosis - Pulmonary stenosis may be caused by a narrowing of the pulmonary valve (valvular stenosis) or the outflow tract of the right ventricle (infundibular stenosis). The narrowing of either the valve or the infundibulum obstructs the flow of blood from the right ventricle into the pulmonary circulation. Consequently, this results in a reduced flow of oxygenated blood in the systemic circulation. If the degree of pulmonary stenosis is mild, a left to right shunt forms. (The higher pressure in the left ventricle causes blood to pass through the septal defect into the right ventricle). However, if the pulmonary stenosis is significant, a right to left shunt will form. This occurs because the stenosis raises the pressure in the right ventricle and forces blood directly into the left ventricle. This is important because deoxygenated blood can now enter the systemic circulation and problems such as cyanosis, dizziness and fainting can occur. The pathophysiology of pulmonary stenosis usually worsens with age because the pulmonary orifice stays the same size despite an increase in the size of the heart.
- Overriding aorta - Instead of being positioned directly over the left ventricle, the aorta is displaced anterosuperiorly. The aortic valve is located directly above the interventricular septal defect allowing blood from both the left and right ventricles to pass through the aortic valve. This biventricular connection allows both oxygenated (from left ventricle) and deoxygenated blood (from right ventricle) to enter the systemic circulation. The degree to which the overriding aorta is continuous with the right ventricle determines the severity of symptoms.
- Ventricular septal defect - The interventricular septum dividing the left and right ventricles is incomplete at its superior, membranous end. During ventricular contraction, blood from the left ventricle is forced into the right ventricle and then re-enters the pulmonary circulation. This extra volume of blood places pressure of the pulmonary system and compensatory pulmonary hypertension and right ventricular hypertrophy may occur. If the right ventricular pressure exceeds that of the left, the left to right shunt is reversed and the patient will experience cyanosis because deoxygenated blood is bypassing the lungs and entering the systemic circulation.
- Right ventricular hypertrophy - Hypertrophy of the right ventricle is a compensatory response to pulmonary stenosis. Because the pulmonary outflow tract is narrowed, the right ventricle must pump harder to meet the oxygen demands of the body.
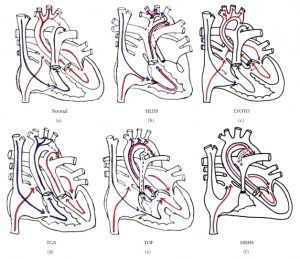
Due to such pathological features in Tetralogy of Fallot, the diagram on the right shows the blood flow in a normal and Tetralogy of Fallot heart.
Diagnostic Tests
Procedures used to diagnose tetralogy of fallot may include an evaluation of signs and symptoms, echocardiography, electrocardiography and chest x-ray.
Signs and symptoms include cyanosis, difficulty feeding and gaining weight, clubbing of fingers and toes, dyspnea on exertion, low oxygen saturation and heart murmur (along the left sternal border, a palpable thrill may be felt and a harsh systolic ejection murmur may be heard).
Echocardiography is used to assess cardiac dimensions including septal wall thickness and interventricular defects, cardiac valves and their functioning and valvular regurgitation.
Electrocardiograms are used to detect abnormal heart rhythms caused by damage to the cardiac conduction fibres.
Chest x-rays are used to detect right ventricular hypertrophy (right ventricle appears larger than normal giving the heart a boot-like appearance).
Treatment/Management
The treatment for TOF consists of medical therapy, surgery & palliative procedures.
Medical therapy:
Medical therapy is usually used to prepare the infant/adult for surgery. The degree of therapy and what is used for treatment, depends upon the degree of cyanosis found in the patient.
- Patients with acute cyanosis usually carry out knee to chest exercise positions in order to decrease the amount of deoxygenated blood entering circulation. This along with providing oxygen & intravenous morphine to provides more blood flow to the lungs and also decrease ventilator drive.
- Patients with severe cyanosis are usually administered intravenous propranolol, which allows for decreases in the muscle spasms that occur in the infundibulum (which causes RVOTO).
- Asymptomatic patients do not require any particular medical treatment.
Palliative Procedures:
Total corrective surgery is the most advantageous option for young infants. However, in some instances, infants suffering from pulmonary atresia or other anomalies (in addition to TOF) may require a palliative method instead because the anomaly changes the candidate’s capability to having total corrective surgery. In some instances, infants with very small pulmonary arteries cannot tolerate corrective surgery and require palliation instead.
The main aim of palliative surgery is to increase pulmonary blood flow and allow for growth and possibly total correction of the pulmonary artery.
By far, the most common procedure is the Blalock-taussig Shut. This shunt is placed between the pulmonary and subclavian arteries.
The major advantage of the Blalock-taussig shunt is that it directs partial oxygenated blood from the subclavian artery to the pulmonary artery (hence the lungs for oxygenation), therefore relieving cyanosis. Due to this feature, the shunt has an excellent success rate.
Other shunts such as the Potts, Waterston and Glenn shunts are either not used or infrequently used today.
Surgery:
Today Tetralogy of fallot can only be treated with open-heart surgery, which is usually performed before 6 months of age. The goal of surgery is to be able to treat the four congenital abnormalities associated with TOF. It is also advantageous to perform this surgery at an early age and not wait until the child is older, however the specific timing of the operation is still under some controversy. Surgeries occur under cardiopulmonary bypass (CPB) and are performed either through the atrium (Transatrial) or from the right atrium/from the pulmonary artery (transatrial-transpulmonary). Surgical approaches are the most common in patients of all ages.
If a patient has had palliative procedures, these shunts must be isolated and taken down, before the actual operation can commence.
In the surgery itself, the surgeon:
- Widens the narrowed pulmonary blood vessels and the pulmonary valve itself, hence allowing for greater blood flow to the lungs.
- Repairs the ventricular septal defect using a patch to cover the hole in the septum.
Fixing these two defects also solves the other two defects (the hypertrophy of the right ventricle wall and provides oxygenated blood to the aorta). When the surgery is carried out during infancy, the incision heals in roughly 6 weeks.
Prognosis
--Mark Hill 16:05, 8 September 2011 (EST) No text here?
Future Directions
--Mark Hill 16:05, 8 September 2011 (EST) No text here?
Glossary
Annular hypoplasia – (need definition)
Arrythmia - (dysrhythmia) Term refers to cardiac abnormality of heartbeat either fast, slow, or irregular.
Ascites – term refers to when there is excess fluid in the space between the tissues lining the abdomen and abdominal organs (the peritoneal cavity).
Clubbing – term refers to changes in the areas under and around the toenails and fingernails, and in the nails themselves that may occur with some disorders
Cyanosis - Clinical term referring to a blue coloration of the skin and mucous membranes due to the presence of deoxygenated hemoglobin. Can be due to several different causes including cyanotic heart disease.
Cyanotic heart disease - Clinical term referring to a congenital heart abnormality (defect) resulting in lack of oxygen that causes cyanosis, a blue coloration of the skin and mucous membranes due to the presence of deoxygenated hemoglobin.
Dyspnoea – term refers to Shortness of breath, difficult or laboured breathing
Edema/Oedema - term for swelling caused by the accumulation of abnormally large amounts of fluid in the spaces between the body's cells or in the circulatory system.
Hepatomegaly – term refers to swelling of the liver beyond its normal size
Murmur – term refers to blowing, whooshing, or rasping sounds heard during a heartbeat. The sound is caused by turbulent blood flow through the heart valves or near the heart
Palpitation – term refers to unusually or abnormally rapid or violent beating of the heart
Shunt – refers to a channel through which blood or other bodily fluid is diverted from its normal path by surgical reconstruction or by a synthetic tube
Stenosis - Term used to describe an abnormal narrowing, usually in relation to a tube. For example, blood vessel, gastrointestinal tract or respiratory tract.
Syncope – refers to brief loss of consciousness associated with transient cerebral anemia, as in heart block, sudden lowering of the blood pressure, etc.; fainting.
References
- ↑ <pubmed>19683809</pubmed>
- ↑ <pubmed>19683809</pubmed>
- ↑ <pubmed>19683809</pubmed>
- ↑ <pubmed>21251297</pubmed>
- ↑ <pubmed>21048055</pubmed>
- ↑ <pubmed>20091166</pubmed>
- ↑ <pubmed>19853711</pubmed>
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/tof/signs.html
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/tof/signs.html
- ↑ http://www.nlm.nih.gov/medlineplus/ency/article/001567.htm
- ↑ <pubmed>21048055</pubmed>
2011 Projects: Turner Syndrome | DiGeorge Syndrome | Klinefelter's Syndrome | Huntington's Disease | Fragile X Syndrome | Tetralogy of Fallot | Angelman Syndrome | Friedreich's Ataxia | Williams-Beuren Syndrome | Duchenne Muscular Dystrolphy | Cleft Palate and Lip