2011 Group Project 1
| Note - This page is an undergraduate science embryology student group project 2011. |
Turner Syndrome
--Mark Hill 10:44, 8 September 2011 (EST) Some of the existing sub-sections have appropriate content, but there are also empty sub-sections, a total lack of referencing/citation and no glossary.
- The referencing issue needs urgent progress.
- Existing figures/table are appropriate. Table appears to be directly used from an uncited source.
- There needs to be more images in this work.
- Where is the student drawn figure?
Introduction
Turner syndrome (or Ullrich-Turner syndrome) is one of the most common chromosomal disorders, caused by complete or partial X monosomy in some or all cells. Approximately 1 in 2000 female live births, however the morbidity rate of spontaneous abortions is 10% and only about 1% of fetuses survive to term.
During normal fetal development, ovaries contain as many as 7 million oocytes. The oocytes gradually reduced to 400,000 during menarche and during menopause fewer than 10,000 remains. However, in Turner syndrome, the ovaries develop normally during embryogenesis but the absence of the second X chromosome leads to an accelerated loss of oocytes, which is complete by age 2 years. In this case genetically menopause occurs before menarche and the ovaries are reduced to atrophic fibrous strands, devoid of ova and follicles (streak ovaries). What is also affected is the development of somatic (nongonadal) tissues that reside on the missing/abnormal X chromosome. For example short stature is caused by a deletion of the Xp chromosome and the deletion of Xq causes gonadal dysfunction [1].
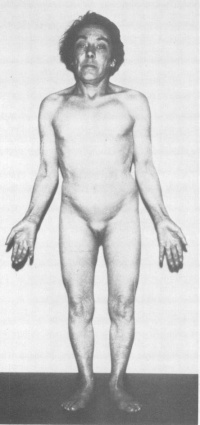
The most frequent clinical feature is short stature and gonadal dysgenesis. Other features may include coarctation of the aorta, renal anomalies, neck webbing, and lymphoedema. The affected organ systems and tissues may are effected to a lesser or greater extent amongst that are affected by turner syndrome. Each person who has turner syndrome all vary in their clinical phenotype. There has been increasing interest in this field because of the introduction in the treatment of turner syndrome with growth hormone. There has been improvement in the understanding of this condition because of the use of molecular genetic techniques. However, there still requires more work in this field. A multidisciplinary approach to treatment is important to improve the quality of life of girls with Turner Syndrome [2].
History
--Mark Hill 10:43, 8 September 2011 (EST) Where is this section's content?
Epidemiology
Turner Syndrome affects about 1 in 2000 live-born females. There are three types of karyotypic abnormalities but the most frequently seen is where the entire X chromosome is missing resulting in 45 X karyotype. The remaining third have structural abnormalities of the X chromosomes, and two thirds are mosaics. Whereby, the maternal X is retained in two-thirds of women and the paternal X in the remainder. The phenotype of Turner Syndrome is varies but it involves anomalies of the sex chromosome. It could be caused by the limited amount of genetic material in these abnormal chromosomes. Turner Syndrome can be transmitted from mother to daughter, and thus can it could be described as a heredity linked syndrome [3].
The loss of one of the sex chromosomes of turner syndrome occurs after the zygote has formed or just after the fusion of the gametes. In 70-80% of cases the retained X is from the mother. In such circumstances has lead to the different phenotypic expression of the genes present on the X chromosome depending upon if it came from the mother or father. The morphological differences from those retaining the maternal compared to retaining the paternal X is have shown to have a greater incidence of cardiovascular anomalies and neck webbing. The missing sex chromosome could be either an X or a Y. This has clinical implications because if the Y material is present there is a risk of up to 30% of gonadoblastoma developing in the dysgenetic gonads. This is because the 'gonadoblastoma locus' is on the Y chromosome which is believed to be situated on the long arm of the Y just below the centromere. Another factor affecting the phenotype in Turner syndrome is the inactivation of the abnormal X chromosomes. In a normal fetus there should be only one X chromosome that is active in each cell [4].
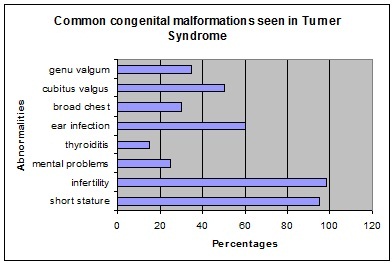
Abnormalities associated with Turner Syndrome
Etiology
--Mark Hill 10:43, 8 September 2011 (EST) Where is this section's content?
Turner Syndrome has also been linked to an increased risk of diabetes mellitus [5]
Clinical manifestations
Turner syndrome is associated with a cognitive phenotype. This includes a low IQ score, nonverbal learning disability, visuoperception deficit and attention deficity disorder. Problems with nonverbal learning involve the difficulty in mathematics. When calculating they are slow. Difficulty in both visuoperception and visuo-constructional tasks is observed when identifying and locating becomes difficult due to poor visual working memory. One other contributing factor to this is the delay in selecting visuospatial tasks. The incidence rate of attention skills and impulsivity in girls with turner syndrome is higher then children in the general population with ADHD [6].
Diagnostic Procedures
Diagnostic Definition
Turner syndrome is diagnosed through both evaluation of physical features and by analysis of the second sex chromosome, which in Turner syndrome is completely or partially absent (with or without cell line mosaicism). The two criteria must be met for classification of Turner syndrome, hence if physical characteristics are not present even when the cytogenetic criterion is met, the patient is not diagnosed as having Turner syndrome.[7] In addition if the homeobox gene, SHOX (short stature homeobox), is not present or if there is a deletion prior to the junction between Xp22.2 and Xp22.3 the patient is also diagnosed with Turner syndrome.[8] Turner syndrome may be diagnosed prenatally and/or postnatally, as outlined below.
Prenatal Diagnosis
The prenatal diagnostic tool for Turner syndrome is karyotype screening. If Turner syndrome is diagnosed prenatally, karyotype screening should be conducted postnatally for confirmation of this diagnoses. Turner syndrome is frequently diagnosed after karyotype screening during chorionic villous sampling or amniocentesis. The table below outlines various prenatal tests and the indications that may be present in babies with Turner syndrome.[9][10] Although these techniques and the indications they reveal may highlight Turner syndrome signs, they should not be used as sole diagnostic tools.
| Technique | Turner syndrome indications | Image |
| Ultrasound |
-Increased nuchal translucency (also in several trisomy syndromes) - Coarctation of the aorta -Left-sided cardiac defects -Renal anomalies -Growth retardation |
|
| Maternal serum screening |
-Abnormal α-fetoprotein levels -Abnormal inhibin Alevels -Abnormal hCGlevels -Abnormal unconjugated estriol levels |
Postnatal Diagnosis
In postnatal diagnosis, karyotype investigation is undertaken for the individual. When a female presents with the following clinical findings, explained in table below, it is recommended that chromosomal analysis is undertaken, so that Turner syndrome may be eliminated:
| Age | Phenotypic manifestations | Image |
| Baby/infant | -Oedema of the hands or feet
-Nuchal folds -Left-sided cardiac mutations, especially of the aorta -Low hairline -Low set ears -Small mandible |
|
| Child |
-Short stature with declining growth velocity (growth velocity <10th percentile for age) -Markedly elevated levels of Follicle-stimulating hormone -Nail hypoplasia -Hyperconvex uplifted nails -Multiple pigmented benign birthmarks/moles -Characteristic facies -Short fourth metacarpal -High arched palate -Extensive and chronic inflammation/infection of the ear |
|
| Adolescence | -Absence of breast development by 13 yr of age
-Pubertal arrest -Primary or secondary amenorrhea with elevated levels of Follicle-stimulating hormone -Unexplained short stature |
Since an absence of the physical signs of puberty and/or growth failure are often seen as normal variations in the population, these possible indications of Turner syndrome may not be further investigated by many clinicians.[11] When karyotyping in order to exclude natural cell variation, a sufficient number of cells should be assessed. Whilst a sample of blood will often reveal Turner syndrome, an evaluation of a second tissue sample like the skin is recommend.[12] DNA hybridisation or fluorescent in situ hybridisation should be conducted using a Y centromeric or short arm probe to detect for any additional Y or X chromosomal material. If there is any of the Y chromosome present, this may initiate gonadoblastoma development, another primary indicator of Turner syndrome. Hence the individual should have both a vaginal sonograph and colour Doppler sonograph of their gonads to detect whether any Y chromosome fragments are present. These tests should be repeated regularly to monitor the patient for any malignancy, if a gonadectomy is not undertaken.
Treatment
The most common abnormality is short stature as bone age is delaged due to the lack of estrogen. This could be treated with the completion of growth hormone therapy.
For young girls use a low dose of natural estrogen to promote and maintain secondary sex characteristics. However recommended to be used when she is approaching puberty in terms of social circumstances as physical sex appearance becomes apparent among her peers.
Evaluation and Management for Turner Syndrome
| MANAGEMENT | METHOD | FEATURE |
| Orthopedic evaluation | Physical examination | Congential hip dislocation |
| Cardiac evaluation and management | Echocardiogram | BAV or COA |
| renal anatomy evaluation | Renal ultrasound | Rotational abnormalities |
| Blood pressure | Physical examination | Hypertension |
| Speech | Speech therapist | Hypertension |
| Speech | Speech therapist | Speech loss |
| Inner ear | Therapist | Hearing loss |
| Outer ear | Observation | Malformation of the outer ear |
| Middle ear | Ventilation tubes | Otitis media |
| Thyroid function | Levels of TSH | Primary hypothyroidism |
| Hearing | Karyotyping | Hearing problems |
| Plastic surgery | Elective surgery | Keloid |
| Vision | Physical examination | Ptosis |
| Orthodontic exam | Orthodontist | Dental abnormalities |
| Weight | Counselling | Obesity |
| Lyphedema | Therapy | Occur and recur at any age |
| Glucose intolerance | Growth promotion | Diabetes |
Current/future research possibilities
Current research is being conducted in the following areas:
Future research could be directed in the following areas:
Glossary
A
A-fetoprotein
Amniocentesis
B
Brachycephaly
C
Coarctation
Chorionic villous sampling
Cubitus valgus is where an individual's elbows are turned in.
Cystic hygroma
Cytogesis refers to cell formation and/or differentiation.
D
DNA-DNA hybridisation is a technique used to compare the similarities and differences between two sets of genes.
Doppler sonography uses the doppler effect to help image and measure the blood flow pattern.
E
Estriol
G
Gonadoblastoma is an abnormal proliferation of gonadal cells, that may or may not be malignant.
H
hCG levels
Hypoplasia is when an organ or tissue is not completely developed.
I
Inhibin A levels
K
Karyotype is an individual's set of chromosomes, both their number and appearance.
M
Mosaicism is when a particular type or all cells of an individual do not have the same genetic makeup. This is caused by a mutation during embryonic cell division.
O
Oligohydramnios
P
Polyhydramnios
S
SHOX gene is the short stature homeobox gene, that when deficient frequently results in short stature.[13]
Sonography is a medical technique that employs ultrasound frequencies to visualise a patient's internal bodily structure.
V
Virilization is the development of phenotypic sex differences.
References
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1273980/?log$=activity
- ↑ http://eje-online.org/content/151/6/657.long
- ↑ http://eje-online.org/content/151/6/657.long
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1511250/?page=2
- ↑ <pubmed>PMC2741724</pubmed>
- ↑ http://jcem.endojournals.org/content/84/12/4345.long
- ↑ <pubmed>11443168</pubmed>
- ↑ <pubmed>21325865</pubmed>
- ↑ <pubmed>3118376</pubmed>
- ↑ <pubmed>1511250</pubmed>
- ↑ <pubmed>20361125</pubmed>
- ↑ <pubmed>1511250</pubmed>
- ↑ <pubmed>21325865</pubmed>
2011 Projects: Turner Syndrome | DiGeorge Syndrome | Klinefelter's Syndrome | Huntington's Disease | Fragile X Syndrome | Tetralogy of Fallot | Angelman Syndrome | Friedreich's Ataxia | Williams-Beuren Syndrome | Duchenne Muscular Dystrolphy | Cleft Palate and Lip