2010 BGD Practical 3 - Implantation: Difference between revisions
(→Terms) |
|||
| Line 36: | Line 36: | ||
* '''bilaminar'''- having 2 layers | * '''bilaminar'''- having 2 layers | ||
* '''blastocyst-''' the developmental stage following morula, as this stage matures, the zona pellucia is lost allowing the conceptus to adplant and then implant into the uterine wall. | * '''blastocyst-''' the developmental stage following morula, as this stage matures, the zona pellucia is lost allowing the conceptus to adplant and then implant into the uterine wall. | ||
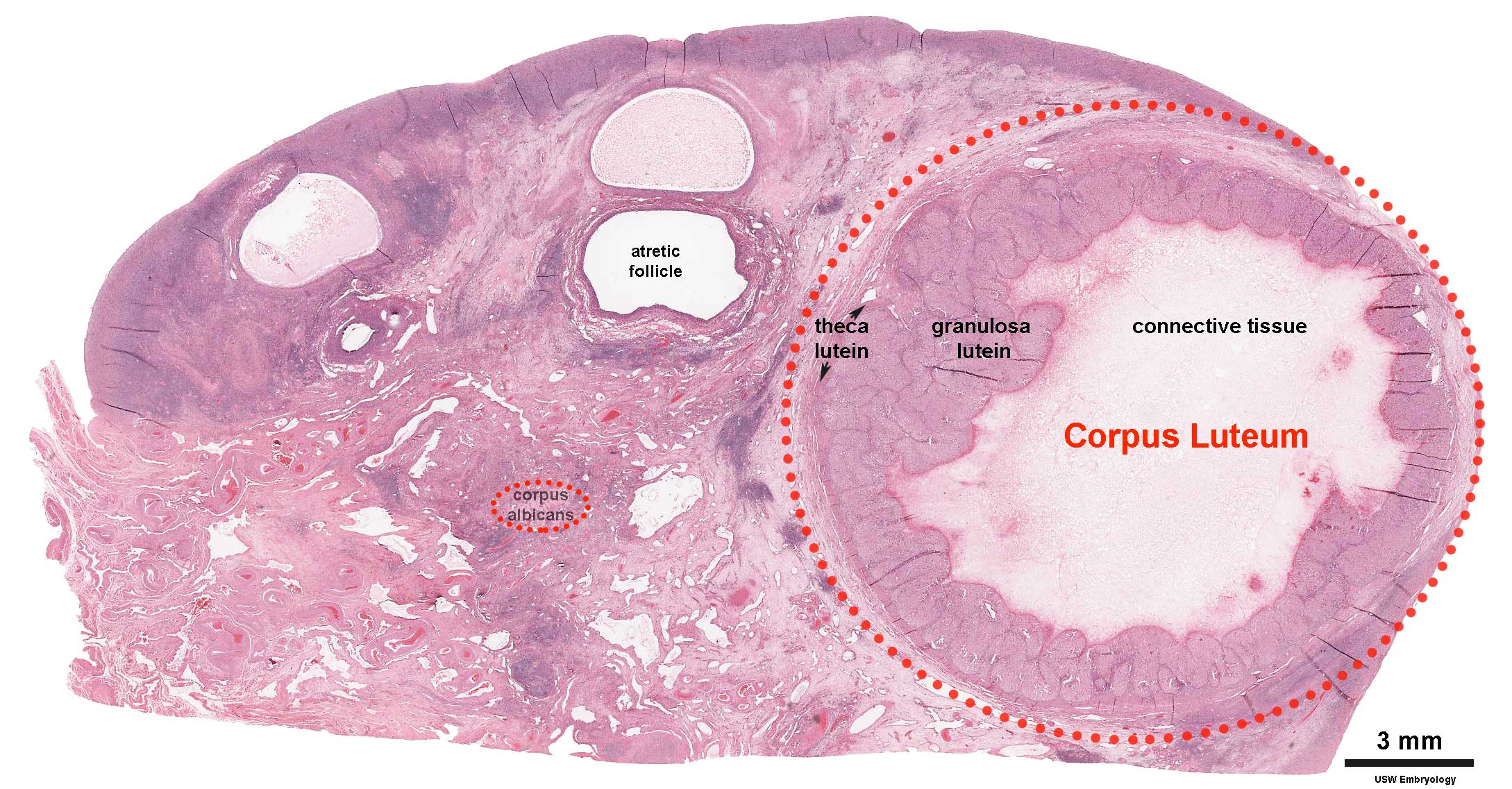
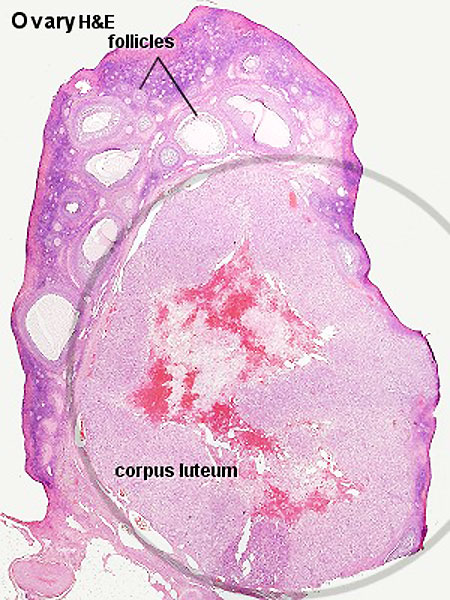
* ''' | * '''corpus albicans''' - (Latin, ''corpus'' = body, ''albicans'' = whitish) The histological structure formed by [[L#luteolysis|luteolysis]] of the [[C#corpus_luteum|corpus luteum]] in the [[O#ovary|ovary]]. If implantation does not occur and the hormone hCG is not released the corpus luteum degenerates and the structure is white, not yellow, because of the absence of steroid hormone synthesis/accumulation. | ||
* ''' | * '''corpus luteum''' - (Latin, ''corpus'' = body, ''luteum'' = yellow) The remains of ovarian [[F#follicle|follicle]] formed after ovulation that acts as an endocrine organ (produce progesterone and oestrogens) supporting pregnancy and preventing menstruation (loss of the endometrial lining). Formed during the [[L#luteal phase|luteal phase]] ([[S#secretory phase|secretory phase]]) of the [[M#menstrual cycle|menstrual cycle]] by proliferation of both follicular granulosa cells (granulosa lutein cells) and thecal cells (theca lutein cells), which produce [[P#progesterone|progesterone]] and [[O#oestrogen|oestrogens]]. If fertilization and pregnancy does not occur, the corpus luteum degenerates to form the [[C#corpus albicans|corpus albicans]]. Regnier de Graaf (1641 – 1673) first observed it in the [[O#ovary|ovary]] of a cow as a yellow structure, the yellow colour is caused by accumulation of steroidal hormones. (More? [[Menstrual Cycle]] | [[Ovary Development]] | [http://embryology.med.unsw.edu.au/Notes/week2_9.htm Week 2 Ovary] | [http://embryology.med.unsw.edu.au/Notes/week1_3a.htm Week 1 - Oogenesis]) | ||
* '''inner cell mass'''- the clump of cells found inside the blastocyst. These cells will go in to form the embryo, these are the "stem cells" (we here about in the media) that are totipotential, they can form any tissue in the embryo. Mature oocyte-the female germ cell released at ovulation from the ovary. | * '''inner cell mass'''- the clump of cells found inside the blastocyst. These cells will go in to form the embryo, these are the "stem cells" (we here about in the media) that are totipotential, they can form any tissue in the embryo. Mature oocyte-the female germ cell released at ovulation from the ovary. | ||
* '''morula''' &endash;(L. morus = mulberry) early stage of development (12-15 cells) Followed by formation of a cavity in the mass (blastocyst stage). (More? Week 1 Notes) | * '''morula''' &endash;(L. morus = mulberry) early stage of development (12-15 cells) Followed by formation of a cavity in the mass (blastocyst stage). (More? Week 1 Notes) | ||
Revision as of 15:29, 9 May 2010
Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 | Quiz
Introduction
Hatching leaves the blastocyst now free of the zona pellucida and should have occured approximately at the end of the uterine tube or in the body of the uterus. It is now floating in the uterine glands rich mucus secretion and able to directly access this nutrition for continued growth.
The blastocyst initially weakly adheres to the endometrial wall rolling across its surface. Increased adhesion may lead to attachment, adplantation, on the inner cell mass side of the blastocyst. This will be the site where implantation will begin and the placenta will develop.
Trophoblast cells at the site of adplantation proliferate and form an additional layer the syncitiotrophoblast layer. This layer of cells rapidly divide, secrete enzymes that degrade the endometrial extracellular matrix and secrete human Chorionic Gonadotropin (hCG).
Implantation Dynamics
The uterine epithelium (white cells) are invaded by the trophoblast cells (green, syncitiotrophoblasts) with the inner cell mass now having 2 layers: an epiblast (blue) and hypoblast (yellow). The blastoceol is covered in cytotrophoblast cells (green).
Later in the movie the amniotic cavity forms adjacent to the epiblast layer(blue) and spaces in the syncitiotrophoblast layer are filled with maternal blood, lacunae.
Identify the embryoblast and trophoblast layers of the conceptus.
Carnegie Stage 4 represents the beginning of implantation. The blastocyst initially attached to the uterine endometrium (adplantation), syncitiotrophoblasts then secrete enzymes that digest extracellular matrix, allowing the blastocyst to sink into the uterine wall, eventually being completely enclosed within the uterine wall. Note the majority of growth occurs in the trophoblastic shell. The inner cell mass divides initially into 2 layers; epiblast and hypoblast (bilaminar embryo). Hypoblast cells migrate around the original blastoceol cavity forming the primary yolk sac. A second cavity (amniotic) forms between the inner cell mass and the cytotrophoblast shell; this cavity is lined by epiblast cells.
Corpus Luteum
An endocrine signal (hCG human Chorionic Gonadotropin) secreted from the implanting conceptus syncitiotrophoblast cells maintains the ovarian corpus luteum, which in turn provides hormonal support to the uterine functional lining, preventing menstruation.
Following ovulation
- If implantation does not occur (non-pregnant), the remnant of the ovulating follicle will degenerate forming a corpus albicans.
- If implantation occurs (pregnancy), the remnant of the ovulating follicle will be maintained forming a corpus luteum.
If implantation does not begin until very late in the current menstrual cycle, or not at all, then that cycle will continue with loss of both the functional layer and the conceptus. Many human fertilization events never form an embryo or develop as a pregnancy.
Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 | Quiz
Terms
- bilaminar- having 2 layers
- blastocyst- the developmental stage following morula, as this stage matures, the zona pellucia is lost allowing the conceptus to adplant and then implant into the uterine wall.
- corpus albicans - (Latin, corpus = body, albicans = whitish) The histological structure formed by luteolysis of the corpus luteum in the ovary. If implantation does not occur and the hormone hCG is not released the corpus luteum degenerates and the structure is white, not yellow, because of the absence of steroid hormone synthesis/accumulation.
- corpus luteum - (Latin, corpus = body, luteum = yellow) The remains of ovarian follicle formed after ovulation that acts as an endocrine organ (produce progesterone and oestrogens) supporting pregnancy and preventing menstruation (loss of the endometrial lining). Formed during the luteal phase (secretory phase) of the menstrual cycle by proliferation of both follicular granulosa cells (granulosa lutein cells) and thecal cells (theca lutein cells), which produce progesterone and oestrogens. If fertilization and pregnancy does not occur, the corpus luteum degenerates to form the corpus albicans. Regnier de Graaf (1641 – 1673) first observed it in the ovary of a cow as a yellow structure, the yellow colour is caused by accumulation of steroidal hormones. (More? Menstrual Cycle | Ovary Development | Week 2 Ovary | Week 1 - Oogenesis)
- inner cell mass- the clump of cells found inside the blastocyst. These cells will go in to form the embryo, these are the "stem cells" (we here about in the media) that are totipotential, they can form any tissue in the embryo. Mature oocyte-the female germ cell released at ovulation from the ovary.
- morula &endash;(L. morus = mulberry) early stage of development (12-15 cells) Followed by formation of a cavity in the mass (blastocyst stage). (More? Week 1 Notes)
- parental genomes- the male (sperm) and female (oocyte) DNA which contributes to the embryo's cells.
- polar bodies- 3 exclusion bodies which contain the DNA not used by the embryo. Contributed to initially by the meiotic division of the oocyte.
- pronuclei- the male (sperm) and female (oocyte) nuclei within the fertilized oocyte, prior to their combination to form the new embryo's nuclei.
- trilaminar embryonic disc- the 3 layered embryo stage.
- Trophoblasts- (Gr. trophe = nutrition) outer layer of cells on blastocyst that will generate the embryonic part of the placenta.
- zona pellucida- glycoprotein shell that surrounds the oocyte through to blastula stage of development.
- Zygote- The first cell stage following fertilization of the oocyte by the sperm. This is the first cell of the conceptus which will divide into blastomeres.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
- 2010 BGD: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12
Cite this page: Hill, M.A. (2024, April 18) Embryology 2010 BGD Practical 3 - Implantation. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_BGD_Practical_3_-_Implantation
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G