2010 BGD Practical 3 - Gametogenesis: Difference between revisions
| (45 intermediate revisions by 2 users not shown) | |||
| Line 3: | Line 3: | ||
==Introduction== | ==Introduction== | ||
Gametes are formed in the gonads; male '''testis''' and female '''ovary''' by the mechanism of meiotic cell division. The generation of gametes, and their regulation, is substantially different in males and females. After puberty, gonads also synthesis and secrete sex hormones into the bloodstream required for development of the secondary sex characteristics. | Gametes are formed in the gonads; male '''testis''' and female '''ovary''' by the mechanism of meiotic cell division. The generation of gametes, and their regulation, is substantially different in males and females. After puberty, gonads also synthesis and secrete sex hormones into the bloodstream required for development of the secondary sex characteristics. | ||
===Practical Audio=== | |||
{| border='0px' | |||
|- | |||
| [[File:Mark_Hill.jpg|60px|left]] | |||
| | |||
BGD Cycle A 2010 Audio - Dr Mark Hill Monday 12th May 2010 12-2pm G2G4. | |||
:Note - this is a live unedited recording from the practical and may contain errors in either descriptions or content. | |||
[[Media:BGD2010-Embryo Lab 120510-303.mp3|listen Part 3]] | [[:File:BGD2010-Embryo Lab 120510-303.mp3|download]] (1.5 Mb MP3 12:03) | |||
|- | |||
|} | |||
== Female Gametogenesis == | == Female Gametogenesis == | ||
| Line 15: | Line 30: | ||
===Female Abnormalities=== | ===Female Abnormalities=== | ||
[[File:Trisomy21female.jpg|thumb|Trisomy 21 female karyotype]] | |||
Meiotic non-disjunction resulting in aneuploidy, most are embryonic lethal and not seen. The potential for genetic abnormalities increase with maternal age. | Meiotic non-disjunction resulting in aneuploidy, most are embryonic lethal and not seen. The potential for genetic abnormalities increase with maternal age. | ||
| Line 31: | Line 46: | ||
In males, sperm continues to be generated throughout life from a stem cell population in the testis. Spermatozoa maturation involves two processes meiosis and spermiogenesis | In males, sperm continues to be generated throughout life from a stem cell population in the testis. Spermatozoa maturation involves two processes meiosis and spermiogenesis | ||
[[File:Male_gametogenesis.jpg|600px]] | [[File:Male_gametogenesis.jpg|600px]] | ||
The above figure compares meiosis to the female (the polar bodies have been removed and labelling updated). | |||
<gallery> | <gallery> | ||
File:Historic-testis.jpg|Historic testis drawing | File:Historic-testis.jpg|Historic testis drawing | ||
| Line 37: | Line 55: | ||
File:Human-spermatozoa.jpg|Human spermatozoa | File:Human-spermatozoa.jpg|Human spermatozoa | ||
</gallery> | </gallery> | ||
===Human Spermatozoa Development=== | |||
* Spermatogenesis process of spermatagonia mature into spermatazoa (sperm). | * Spermatogenesis process of spermatagonia mature into spermatazoa (sperm). | ||
* Continuously throughout life occurs in the seminiferous tubules in the male gonad- testis (plural testes). | * Continuously throughout life occurs in the seminiferous tubules in the male gonad- testis (plural testes). | ||
* At puberty spermatagonia activate and proliferate (mitosis). | * At puberty spermatagonia activate and proliferate (mitosis). | ||
* about 48 days from entering meiosis until morphologically mature spermatozoa | |||
* about 64 days to complete spermatogenesis, depending reproduction time of spermatogonia | |||
* follicle stimulating hormone (FSH) - stimulates the spermatogenic epithelium | |||
* luteinizing-hormone (LH) - stimulates testosterone production by Leydig cells | |||
[[File:Spermatozoa animation icon.jpg|200px|link=Development_Animation_-_Spermatozoa]] | [[File:Human-spermatozoa_EM01.jpg|600px]] | ||
{| | |||
|- | |||
| [[File:Spermatozoa animation icon.jpg|200px|link=Development_Animation_-_Spermatozoa]] | |||
| '''Mature human spermatozoa''' | |||
* 60 µm long, actively motile | |||
* divided into 3 main regions (head, neck and tail) | |||
* head - (flattened, 5 µm long by 3 µm wide) the nucleus and acrosome. Posterior part of nuclear membrane forms the basal plate. | |||
* neck - (1 µm) attached to basal plate, transverse oriented centriole, contains nine segmented columns of fibrous material, continue as outer dense fibres in tail. | |||
* tail - 3 parts a middle piece, principal piece and end piece | |||
** middle piece - (5 µm long) [[A#axonema|axonema]] and dense fibres surrounded by mitochondria | |||
** principal piece - (45 µm long) fibrous sheath interconnected by regularly spaced circumferential hoops | |||
** end piece - (5 µm long) [[A#axonema|axonema]] surrounded by small amount of cytoplasm and plasma membrane | |||
|- | |||
|} | |||
'''Links:''' [http://www.ncbi.nlm.nih.gov | '''Links:''' [[Spermatozoa Development]] | [http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=mboc4&part=A3729 MBoC - Sperm] | [http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=mboc4&part=A3729&rendertype=figure&id=A3735 MBoC - Highly simplified drawing of a cross-section of a seminiferous tubule in a mammalian testis] | [http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=mboc4&part=A3729&rendertype=figure&id=A3736 MBoC - Cytoplasmic bridges in developing sperm cells and their precursors] | ||
===Puberty=== | ===Puberty=== | ||
| Line 57: | Line 94: | ||
===Ejeculate=== | ===Ejeculate=== | ||
[[File:Azoospermia.jpg|thumb|Azoospermia - Non-obstructive azoospermia (NOA) and Obstructive azoospermia (OA)]] | |||
*release of spermatozoa and accessory gland secretions from the male genital tract (3.5 ml) | *release of spermatozoa and accessory gland secretions from the male genital tract (3.5 ml) | ||
* 200-600 million sperm, by volume less than 10 % spermatozoa | * 200-600 million sperm, by volume less than 10 % spermatozoa | ||
| Line 72: | Line 109: | ||
{| border='0px' width=90% | {| border='0px' width=90% | ||
|- | |-bgcolor="lightsteelblue" | ||
| | | | ||
| '''Female Oogenesis''' | | '''Female Oogenesis''' | ||
| Line 107: | Line 144: | ||
{{Template:2010BGDLab3}} | {{Template:2010BGDLab3}} | ||
== | ==Additional Information== | ||
'''The information below is not part of today's Practical.''' | |||
* Male Histology - covered in a later practical class | |||
* Genetic Information | |||
* Gynaecological cancer information, as they are an important clinical topic specific to these reproductive organs. | |||
===Male Histology=== | |||
'''Links:''' [http://www.lab.anhb.uwa.edu.au/mb140/CorePages/MaleRepro/malerepro.htm Male Reproductive Tract Histology] | |||
===Genetics=== | |||
<gallery> | |||
* ''' | File:Autosomal_dominant_inheritance.jpg|Autosomal dominant inheritance | ||
* ''' | File:Autosomal recessive inheritance.jpg|Autosomal recessive inheritance | ||
* ''' | File:X-Linked_dominant_(affected_father).jpg|X-Linked dominant (affected father) | ||
File:X-Linked_dominant_(affected_mother).jpg|X-Linked dominant (affected mother) | |||
File:X-Linked_recessive_(affected_father).jpg|X-Linked recessive (affected father) | |||
* ''' | File:X-Linked recessive (carrier mother).jpg|X-Linked recessive (carrier mother) | ||
* ''' | File:Mitochondrial_inheritance.jpg|Mitochondrial genome inheritance | ||
File:Codominant inheritance.jpg|Codominant inheritance | |||
</gallery> | |||
* ''' | |||
* ''' | {{Template:GHR Inheritance}} | ||
* ''' | |||
===Gynaecological Cancers=== | |||
* ''' | '''Main Types:''' Ovarian cancer (ICD-10 code C56) | Cervical cancer (ICD-10 code C53) | Uterine cancer (ICD-10 codes C54 and C55) | Other gynaecological cancers (ICD-10 codes C51, C52, C57 and C58) | ||
* ''' | [http://www.aihw.gov.au/publications/index.cfm/title/11158 Ovarian cancer in Australia: an overview, 2010] | ||
:"Ovarian cancer was the most common cause of gynaecological cancer death and the sixth most common cause of cancer-related death among Australian women in 2006." | |||
* ''' | [http://www.aihw.gov.au/publications/index.cfm/title/11158 Cervical screening in Australia 2006-2007] | ||
* ''' | :"Incidence and mortality of cervical cancer in Australia remain low, consistent with the Program’s aim to reduce incidence and mortality. There were 9.2 new cases per 100,000 women in 2005, and 1.9 deaths per 100,000 women in 2006 (aged 20-69 years). Incidence for Aboriginal and Torres Strait Islander women has been estimated to be more than double (ABS & AIHW 2008), and mortality found to be five times that of other Australian women." | ||
Links: [http://www.aihw.gov.au/publications/index.cfm/title/11158 Ovarian cancer in Australia: an overview, 2010] | [http://www.aihw.gov.au/publications/index.cfm/title/11687 Australian Gynaecological cancer projections 2010-2015] | |||
==Terms== | |||
* '''sperm''' - See [[S#spermatozoa|spermatozoa]]. The male haploid reproductive cell, often used generically (and incorrectly) to describe these cells and the fluid of the ejaculate. Term is a shortened form of scientifically correct term [[S#spermatazoa|spermatazoa]]. | |||
* '''sperm annulus''' - (Jensen's ring; Latin, ''annulus'' = ring) A region of the mammalian sperm flagellum connecting the midpiece and the principal piece. The annulus is a septin-based structure formed from SEPT1, 4, 6, 7 and 12. Septins are polymerizing GTPases that can act as a scaffold forming hetero-oligomeric filaments required for cytokinesis and other cell cycle roles. | |||
* '''spermatid''' - Intermediate cell in spermatozoa development, within the testis seminiferous tubule they lie in the luminal cell layer to the [[S#secondary spermatocyte|secondary spermatocyte]]. These small cells are haploid and in [[S#spermiogenesis|spermiogenesis]] change their cellular structure and shape to form [[S#spermatozoa|spermatozoa]]. | |||
:(More? [[Spermatozoa Development]] | [[Testis Development]] | [[Fertilization]] | [[2009 Lecture 2|Lecture - Cell Division/Fertilization]]) | |||
* '''spermatogenesis''' - (Greek, ''genesis'' = origin, creation, generation) The term used to describe the process of diploid spermatagonia division and differentiation to form haploid spermatazoa within the testis (male gonad). The process includes the following cellular changes: meiosis, reoorganization of DNA, reduction in DNA content, reorganization of cellular organelles, morphological changes (cell shape). The final process of change in cell shape is also called [[S#spermiogenesis|spermiogenesis]]. | |||
* '''spermiogenesis''' - (Greek, ''genesis'' = origin, creation, generation) The maturation process of the already haploid [[S#spermatid|spermatids]] into the mature [[S#spermatozoa|spermatozoa]] shape and organization. This process involves reorganization of cellular organelles ([[E#endoplasmic reticulum|endoplasmic reticulum]], [[G#golgi apparatus|Golgi apparatus]], [[M#mitochondria|mitochondria]]), cytoskeletal changes (microtubule organization) and morphological changes (cell shape, acrosome and tail formation). The process of maturation of the [[S#spermatid|spermatids]] into spermatozoa: chromatin condenses, nucleus becomes smaller, the [[G#golgi apparatus|Golgi apparatus]] is modified to form the [[A#acrosome|acrosome]], microtubules are reorganised to form the tail, mitochondria are relocated to the initial segment of the tail and the majority of cell cytoplasm is discarded. | |||
* '''spermatogonia''' - These cells form in the embryo from the [[P#primordial germ cell|primordial germ cell]] and are located in the seminiferous tubule adjacent to the basal membrane. The cells can either divide and separate to renew the stem cell population, or they divide and stay together as a pair ([[A#Apr spermatogonia|Apr spermatogonia]]) connected by an intercellular cytoplasmic bridge to begin to differentiate and eventually form [[S#spermatazoa|spermatazoa]]. | |||
* '''spermatozoa''' - (spermatozoon, singular term) The male haploid gamete cell produced by meiosis in the testis (male gonad) seminiferous tubule. In humans, produced from puberty onwards and develop from the diploid stem cell the [[S#spermatogonia|spermatogonia]]. The developmental meiosis is called [[S#spermatogenesis|spermatogenesis]] and the final morphologiccal (shape) change is called [[S#spermeiogenesis|spermeiogenesis]]. The mature human spermatozoon formed from the [[S#spermatid|spermatid]] has a head, neck and tail and is about 60 µm long. At ejaculation these cells undergo [[C#capacitation|capacitation]] are activated and become motile. | |||
* '''spermatozoa head''' - Following [[S#spermiogenesis|spermiogenesis]], the first region of the [[S#spermatozoa|spermatozoa]] containing the haploid nucleus and acrosome. In humans, it is a flattened structure (5 µm long by 3 µm wide) with the posterior part of nuclear membrane forming the basal plate region. The human [[S#spermatozoa|spermatozoa]] is about 60 µm long, actively motile and divided into 3 main regions ([[S#spermatozoa head|head]], [[S#spermatozoa neck|neck]] and [[S#spermatozoa tail|tail]]). | |||
* '''spermatozoa neck''' - Following [[S#spermiogenesis|spermiogenesis]], the second region of the [[S#spermatozoa|spermatozoa]] attached to basal plate, transverse oriented centriole, contains nine segmented columns of fibrous material, continue as outer dense fibres in tail. In humans, it forms a short structure (1 µm). The human [[S#spermatozoa|spermatozoa]] is about 60 µm long, actively motile and divided into 3 main regions ([[S#spermatozoa head|head]], [[S#spermatozoa neck|neck]] and [[S#spermatozoa tail|tail]]). | |||
* '''spermatozoa tail''' - Following [[S#spermiogenesis|spermiogenesis]], the third region of the [[S#spermatozoa|spermatozoa]] that has a ([[S#spermatozoa head|head]], [[S#spermatozoa neck|neck]] and [[S#spermatozoa tail|tail]]). The tail is also divided into 3 structural regions a middle piece, a principal piece and an end piece. In humans: the middle piece (5 µm long) is formed by [[A#axonema|axonema]] and dense fibres surrounded by mitochondria; the principal piece (45 µm long) fibrous sheath interconnected by regularly spaced circumferential hoops; the final end piece (5 µm long) has an [[A#axonema|axonema]] surrounded by small amount of cytoplasm and plasma membrane. | |||
* '''spermatogonial stem cells''' - (SSCs) The [[S#spermatagonia|spermatagonia cells]] located beside the seminiferous tubule basal membrane that either divide and separate to renew the stem cell population, or they divide and stay together as a pair ([[A#Apr spermatogonia|Apr spermatogonia]]) connected by an intercellular cytoplasmic bridge to differentiate and eventually form [[S#spermatazoa|spermatazoa]]. | |||
* '''sperm protein 56''' - A component of the spermatozoa acrosomal matrix released to the sperm surface during [[C#capacitation|capacitation]]. | |||
[[Category:Meiosis]] [[Category:Gametogenesis]] | |||
{{Template:BGDFooter2010}} | {{Template:BGDFooter2010}} | ||
Latest revision as of 11:33, 6 May 2012
Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 | Quiz
Introduction
Gametes are formed in the gonads; male testis and female ovary by the mechanism of meiotic cell division. The generation of gametes, and their regulation, is substantially different in males and females. After puberty, gonads also synthesis and secrete sex hormones into the bloodstream required for development of the secondary sex characteristics.
Practical Audio
|
BGD Cycle A 2010 Audio - Dr Mark Hill Monday 12th May 2010 12-2pm G2G4.
listen Part 3 | download (1.5 Mb MP3 12:03) |
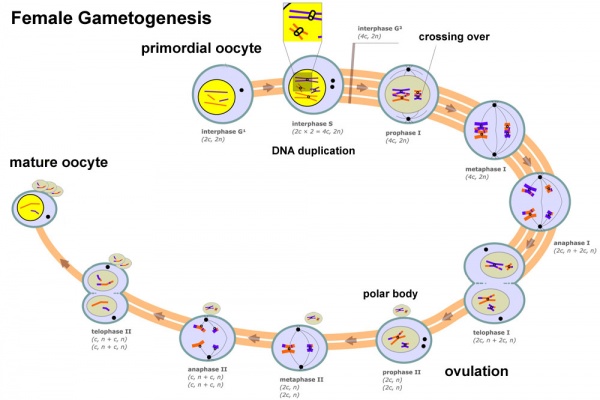
Female Gametogenesis
In females, the total number of eggs ever to be produced are present in the newborn female.
- All eggs are arrested at an early stage of the first meiotic division as a primary oocyte (primordial follicle). Following purberty, during each menstrual cycle, pituitary gonadotrophin stimulates completion of meiosis 1 the day before ovulation.
- In meiosis 1, a diploid cell becomes 2 haploid (23 chromosomes) daughter cells, each chromosome has two chromatids. One cell becomes the secondary oocyte the other cell forms the first polar body.
- The secondary oocyte then commences meiosis 2 which arrests at metaphase and will not continue without fertilization.
- At fertilization meiosis 2 completes, forming a second polar body. Note that the first polar body may also undergo this process forming a third polar body.
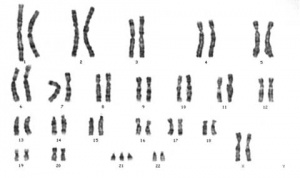
Female Abnormalities
Meiotic non-disjunction resulting in aneuploidy, most are embryonic lethal and not seen. The potential for genetic abnormalities increase with maternal age.
- Autosomal chromosome aneuploidy
- trisomy 21 - Down syndrome
- trisomy 18 - Edwards syndrome
- trisomy 13 - Patau syndrome
- Sex chromosome aneuploidy
- monosomy X - Turner's Syndrome
- trisomy X - Triple-X syndrome
- 47 XXY - Klinefelter's Syndrome
Male Gametogenesis
In males, sperm continues to be generated throughout life from a stem cell population in the testis. Spermatozoa maturation involves two processes meiosis and spermiogenesis
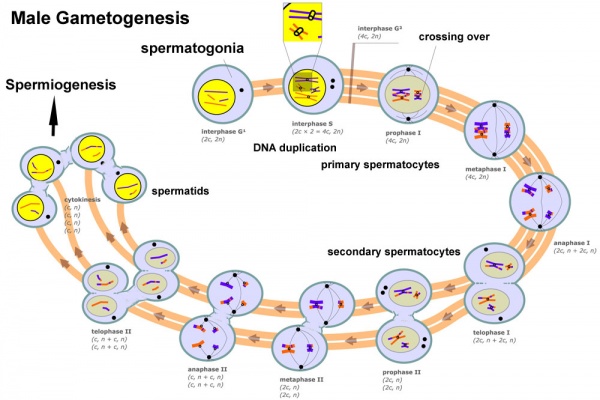
The above figure compares meiosis to the female (the polar bodies have been removed and labelling updated).
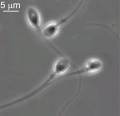
Human Spermatozoa Development
- Spermatogenesis process of spermatagonia mature into spermatazoa (sperm).
- Continuously throughout life occurs in the seminiferous tubules in the male gonad- testis (plural testes).
- At puberty spermatagonia activate and proliferate (mitosis).
- about 48 days from entering meiosis until morphologically mature spermatozoa
- about 64 days to complete spermatogenesis, depending reproduction time of spermatogonia
- follicle stimulating hormone (FSH) - stimulates the spermatogenic epithelium
- luteinizing-hormone (LH) - stimulates testosterone production by Leydig cells
Links: Spermatozoa Development | MBoC - Sperm | MBoC - Highly simplified drawing of a cross-section of a seminiferous tubule in a mammalian testis | MBoC - Cytoplasmic bridges in developing sperm cells and their precursors
Puberty
- In humans at puberty, hormonal and morphological changes occur within the gonad and other systems (secondary sex characteristics).
- Within the testis the immature Sertoli cells cease to proliferate and differentiate.
- Spermatogonium proliferate and spermatogenesis begins.
- It takes about 70 days for cells to mature from the diploid spermatogonium to a primary spermatocyte.
- This maturation occurs in waves along the seminiferous tubules.
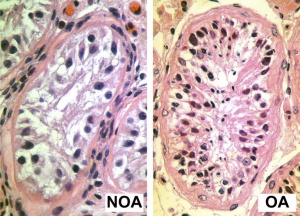
Ejeculate
- release of spermatozoa and accessory gland secretions from the male genital tract (3.5 ml)
- 200-600 million sperm, by volume less than 10 % spermatozoa
- Accessory Gland secretions - 60 % seminal vesicle, 30 % prostate and 10 % bulbourethral
Male Abnormalities
- Oligospermia - (Low Sperm Count) less than 20 million sperm after 72 hour abstinence from sex
- Azoospermia - (Absent Sperm) blockage of duct network
- Immotile Cilia Syndrome - lack of sperm motility
Differences in Mammalian Meioses
| Female Oogenesis | Male Spermatogenesis | |
| Meiosis initiated | once in a finite population of cells | continuously in mitotically dividing stem cell population |
| Gametes produced | 1 / meiosis | 4 / meiosis |
| Meiosis completed | delayed for months or years | completed in days or weeks |
| Meiosis Arrest | arrest at 1st meiotic prophase | no arrest differentiation proceed continuously |
| Chromosome Equivalence | All chromosomes exhibit equivalent transcription and recombination during meiotic prophase | Sex chromosomes excluded from recombination and transcription during first meiotic prophase |
| Gamete Differentiation | occurs while diploid (in first meiotic prophase) | occurs while haploid (after meiosis ends) |
Practical 3: Oogenesis and Ovulation | Gametogenesis | Fertilization | Early Cell Division | Week 1 | Implantation | Week 2 | Extraembryonic Spaces | Gastrulation | Notochord | Week 3 | Quiz
Additional Information
The information below is not part of today's Practical.
- Male Histology - covered in a later practical class
- Genetic Information
- Gynaecological cancer information, as they are an important clinical topic specific to these reproductive organs.
Male Histology
Links: Male Reproductive Tract Histology
Genetics
- Inheritance Pattern images: Genetic Abnormalities | autosomal dominant | autosomal recessive | X-linked dominant (affected father) | X-Linked dominant (affected mother) | X-Linked recessive (affected father) | X-Linked recessive (carrier mother) | mitochondrial inheritance | Codominant inheritance | Genogram symbols | Genetics
Gynaecological Cancers
Main Types: Ovarian cancer (ICD-10 code C56) | Cervical cancer (ICD-10 code C53) | Uterine cancer (ICD-10 codes C54 and C55) | Other gynaecological cancers (ICD-10 codes C51, C52, C57 and C58)
Ovarian cancer in Australia: an overview, 2010
- "Ovarian cancer was the most common cause of gynaecological cancer death and the sixth most common cause of cancer-related death among Australian women in 2006."
Cervical screening in Australia 2006-2007
- "Incidence and mortality of cervical cancer in Australia remain low, consistent with the Program’s aim to reduce incidence and mortality. There were 9.2 new cases per 100,000 women in 2005, and 1.9 deaths per 100,000 women in 2006 (aged 20-69 years). Incidence for Aboriginal and Torres Strait Islander women has been estimated to be more than double (ABS & AIHW 2008), and mortality found to be five times that of other Australian women."
Links: Ovarian cancer in Australia: an overview, 2010 | Australian Gynaecological cancer projections 2010-2015
Terms
- sperm - See spermatozoa. The male haploid reproductive cell, often used generically (and incorrectly) to describe these cells and the fluid of the ejaculate. Term is a shortened form of scientifically correct term spermatazoa.
- sperm annulus - (Jensen's ring; Latin, annulus = ring) A region of the mammalian sperm flagellum connecting the midpiece and the principal piece. The annulus is a septin-based structure formed from SEPT1, 4, 6, 7 and 12. Septins are polymerizing GTPases that can act as a scaffold forming hetero-oligomeric filaments required for cytokinesis and other cell cycle roles.
- spermatid - Intermediate cell in spermatozoa development, within the testis seminiferous tubule they lie in the luminal cell layer to the secondary spermatocyte. These small cells are haploid and in spermiogenesis change their cellular structure and shape to form spermatozoa.
- (More? Spermatozoa Development | Testis Development | Fertilization | Lecture - Cell Division/Fertilization)
- spermatogenesis - (Greek, genesis = origin, creation, generation) The term used to describe the process of diploid spermatagonia division and differentiation to form haploid spermatazoa within the testis (male gonad). The process includes the following cellular changes: meiosis, reoorganization of DNA, reduction in DNA content, reorganization of cellular organelles, morphological changes (cell shape). The final process of change in cell shape is also called spermiogenesis.
- spermiogenesis - (Greek, genesis = origin, creation, generation) The maturation process of the already haploid spermatids into the mature spermatozoa shape and organization. This process involves reorganization of cellular organelles (endoplasmic reticulum, Golgi apparatus, mitochondria), cytoskeletal changes (microtubule organization) and morphological changes (cell shape, acrosome and tail formation). The process of maturation of the spermatids into spermatozoa: chromatin condenses, nucleus becomes smaller, the Golgi apparatus is modified to form the acrosome, microtubules are reorganised to form the tail, mitochondria are relocated to the initial segment of the tail and the majority of cell cytoplasm is discarded.
- spermatogonia - These cells form in the embryo from the primordial germ cell and are located in the seminiferous tubule adjacent to the basal membrane. The cells can either divide and separate to renew the stem cell population, or they divide and stay together as a pair (Apr spermatogonia) connected by an intercellular cytoplasmic bridge to begin to differentiate and eventually form spermatazoa.
- spermatozoa - (spermatozoon, singular term) The male haploid gamete cell produced by meiosis in the testis (male gonad) seminiferous tubule. In humans, produced from puberty onwards and develop from the diploid stem cell the spermatogonia. The developmental meiosis is called spermatogenesis and the final morphologiccal (shape) change is called spermeiogenesis. The mature human spermatozoon formed from the spermatid has a head, neck and tail and is about 60 µm long. At ejaculation these cells undergo capacitation are activated and become motile.
- spermatozoa head - Following spermiogenesis, the first region of the spermatozoa containing the haploid nucleus and acrosome. In humans, it is a flattened structure (5 µm long by 3 µm wide) with the posterior part of nuclear membrane forming the basal plate region. The human spermatozoa is about 60 µm long, actively motile and divided into 3 main regions (head, neck and tail).
- spermatozoa neck - Following spermiogenesis, the second region of the spermatozoa attached to basal plate, transverse oriented centriole, contains nine segmented columns of fibrous material, continue as outer dense fibres in tail. In humans, it forms a short structure (1 µm). The human spermatozoa is about 60 µm long, actively motile and divided into 3 main regions (head, neck and tail).
- spermatozoa tail - Following spermiogenesis, the third region of the spermatozoa that has a (head, neck and tail). The tail is also divided into 3 structural regions a middle piece, a principal piece and an end piece. In humans: the middle piece (5 µm long) is formed by axonema and dense fibres surrounded by mitochondria; the principal piece (45 µm long) fibrous sheath interconnected by regularly spaced circumferential hoops; the final end piece (5 µm long) has an axonema surrounded by small amount of cytoplasm and plasma membrane.
- spermatogonial stem cells - (SSCs) The spermatagonia cells located beside the seminiferous tubule basal membrane that either divide and separate to renew the stem cell population, or they divide and stay together as a pair (Apr spermatogonia) connected by an intercellular cytoplasmic bridge to differentiate and eventually form spermatazoa.
- sperm protein 56 - A component of the spermatozoa acrosomal matrix released to the sperm surface during capacitation.
Glossary Links
- Glossary: A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | W | X | Y | Z | Numbers | Symbols | Term Link
- 2010 BGD: Lecture 1 | Lecture 2 | Practical 3 | Practical 6 | Practical 12
Cite this page: Hill, M.A. (2024, April 18) Embryology 2010 BGD Practical 3 - Gametogenesis. Retrieved from https://embryology.med.unsw.edu.au/embryology/index.php/2010_BGD_Practical_3_-_Gametogenesis
- © Dr Mark Hill 2024, UNSW Embryology ISBN: 978 0 7334 2609 4 - UNSW CRICOS Provider Code No. 00098G