User:Z5001524
Introduction
During pregnancy, the maternal bloodstream does not only contain maternal cells but also fetal cells and fetal DNA. Hence, the fetus will expose its cells and DNA into the maternal blood and the DNA is generally known as cell-free fetal DNA (cffDNA) [1]. The fetal cells include nucleated red blood cells, fetal trophoblast cells, mesenchymal stem cells and leucocytes and they will circulate through the maternal blood stream freely. However, the analysis of the fetal cells in maternal blood has been a challenge due to the scarcity of them in the circulation (1:10,000-1:1,000,000). Therefore, recent studies focus more on cffDNA, which has a proportion of 2-6% of the DNA in maternal blood [2][3]. Although the understanding of their functions in the maternal blood is still limited (especially fetal cells), the current comprehension of cffDNA facilitate the diagnosis of many birth defects and abnormalities to lower the risk of miscarriage [1].
Origin and microchimerism of cffDNA
The fetal DNA originate from trophoblast cells [4]. After implantation, the trophoblast cells will start to form the placenta. During this formation process, some trophoblast cells will undergo apoptosis and the DNA of the fetus will be fragmented. Eventually, they will be able to distribute and migrate into the maternal circulation through passing the intervillus space, which is filled with maternal blood [5]. This has explained the increase in the number of fetal DNA in the maternal blood after implantation and presence of fetal DNA can be detected starting from the 4 week of gestation [6]. However, the detection of fetal DNA in maternal blood in diagnostic tests is only reliable from 7 weeks of gestation onwards [7]. The levels of cffDNA in the maternal blood increase with gestational age and rise by approximately 64 fetal genomes per ml of maternal bloodstream between the first trimester and third trimester [8]. It will then reach its peak within last 8 weeks of gestation and decline after delivery [9].
More information on: Implantation| Placenta Development
Potential functions of fetal cells in the maternal blood
The functions of these cells that exist in maternal blood are still a mystery. However, it has been deduced that these cells would contribute in tolerating the maternal immune system and alter the immune system cells from attacking the fetus [10].
Furthermore, the fetal cells in the bloodstream will also migrate to maternal organs such as lung and heart and the studies have found out the fetal cells and the placental cells have the ability to differentiate and repair the injuries in both the lungs and heart[11].
Fetal stem cells have also been deduced to have the functions of alleviating rheumatoid arthritis and as a preventative effect on breast cancer [9]. Although these cells are found in tumors, there are no specific findings that explain whether its effect is in preventing or restricting the growth of tumors [12].
More information on: Rheumatoid arthritis| Breast cancer| Fetal cells differentiation in heart
Prenatal diagnosis uses
Problems of common diagnostic tests
Chorionic villus sampling and amniocentenses are the common diagnostic methods used to detect whether the fetus has [Down Syndrome] and other abnormalities. Although these methods have very low false positive rates, the tests can only be conducted and indicate accurate results at a relatively late period. Besides, these two tests are invasive prenatal testings and both carry a chance of miscarriage or harming the fetus [13].
More information on Chorionic villus sampling | Prenatal Diagnosis | Amniocentesis
Uses of maternal blood in non-invasive prenatal testing
As the cffDNA has been discovered in maternal blood, this enables the testing of the fetal genome from the collection of the maternal blood. This testing is regarded as a non-invasive prenatal testing (NIPT). The fetal blood group, sex and also chromosomal abnormalities can also be determined by this testing.
Some examples of cffDNA testing [14].
Fetal rhesus D type --- The identification of the fetal blood status from maternal blood to indicate the risk of having haemolytic disease.
Fetal sex --- The determination of Y chromosomes sequences such as DYS or SRY. Male fetus with chances of having an X-linked disorder can be primarily tested with cffDNA testing to determine whether the fetus needs an invasive diagnostic test such as polymerase chain reaction(PCR).
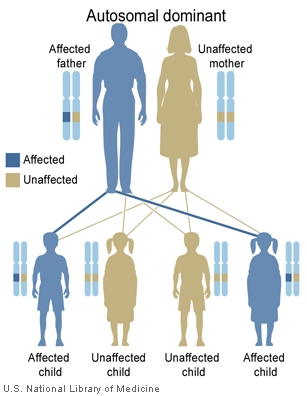
Single gene disorders --- The detection and elimination of the condition of the paternal allele inherited from a father with an autosomal dominant condition such as Huntington's disease.
Further reading on Non-invasive prenatal testing for chromosomal abnormality using maternal plasma DNA
Disadvantages of cffDNA testing[10]
Since this test is used to screen disease nonspecifically for chromosomal aneuploidies, the pregnant women will be constantly informed about the findings, even those which are uncertain. These uncertain findings may lead to unnecessary worries. Besides, the similar situation also applies to ultrasound scanning and other microarray analyses. However, this problem can be solved when there is a better understanding of genetic diseases and, therefore, a specific and detailed examination will be established.
Some Recent Findings
- Significance of maternal and cord blood nucleated red blood cell count in pregnancies complicated by preeclampsia [15] "Until the sixth and seventh weeks of gestation, all fetal red blood cells are nucleated. By the twelfth week of gestation, nucleated red blood cell counts decline...This study was undertaken to assess the extent to which NRBCs were associated with adverse neonatal outcome in preeclampsia and healthy pregnant women and see if this count is a reliable marker to predict early neonatal outcome. Another aspect of the study was determination of the difference between the cord blood NRBC counts of preeclamptic and healthy pregnant patients. Maternal NRBC count was studied as in some studies it was postulated that disturbed fetomaternal cell trafficking in preeclampsia leads to raised maternal NRBCs...Cord blood nucleated red blood cells are significantly raised in preeclampsia and are associated with adverse early neonatal outcome. Neonates with elevated cord blood NRBC counts are more likely to have IUGR, low birth weight, neonatal ICU admission, respiratory distress syndrome, and assisted ventilation. Below the count of 13/100 leucocytes, adverse neonatal outcomes are quite less likely."
- The cell-free fetal DNA fraction in maternal blood decreases after physical activity[16] "This study’s objective is to determine whether physical activity has an effect on the proportion of cell-free DNA (cfDNA) arising from the fetus (fetal fraction)...The main finding of this study is that 30 min of physical activity(bicycling with a pulse of 150 beats per minute) decreased the fetal fraction. This was mainly caused by an increased concentration of cfDNA, whereas the concentration of cffDNA remained mostly unaffected...Physical activity shortly before blood sampling decreases the fetal fraction, so it should be recommended that pregnant women having noninvasive prenatal screening on the basis of fetal fraction avoid physical activity at least within 30 min prior to blood sampling."
- The immunology of pregnancy: Regulatory T cells control maternal immune tolerance toward the fetus[10] "Regulatory T (Treg) cells, a subset of suppressor CD4+ T cells, play a dominant role in the maintenance of immunological self-tolerance by preventing immune and autoimmune responses against self-antigens...Different factors such as cytokines, adipokines, pregnancy hormones and seminal fluid have immunoregulatory activity and influence the success of pregnancy by increasing Treg cell number and activity. The development of strategies capable of modulating immune responses toward fetal antigens through Treg cell manipulation, could have an impact on the induction of tolerance against fetal antigens during immune-mediated recurrent abortion."
References
- ↑ 1.0 1.1 <pubmed>10472878</pubmed>
- ↑ <pubmed>24466384</pubmed>
- ↑ <pubmed>9504651</pubmed>
- ↑ Nigam A, Saxena P, Prakash A & Acharya AS. (2012). Detection of fetal nucleic acid in maternal plasma: A novel noninvasive prenatal diagnostic technique. Journal of Internation Medical Sciences Academy, 25(3), 199.
- ↑ Smets, E. M. L., Visser, A., Go, A. T. J. I., van Vugt, J. M. G., & Oudejans, C. B. M. (2006). Novel biomarkers in preeclampsia. Clinica Chimica Acta, 364(1–2), 22-32. doi:http://dx.doi.org/10.1016/j.cca.2005.06.011
- ↑ Nigam A, Saxena P, Prakash A & Acharya AS. (2012). Detection of fetal nucleic acid in maternal plasma: A novel noninvasive prenatal diagnostic technique. Journal of Internation Medical Sciences Academy, 25(3), 199.
- ↑ Nigam A, Saxena P, Prakash A & Acharya AS. (2012). Detection of fetal nucleic acid in maternal plasma: A novel noninvasive prenatal diagnostic technique. Journal of Internation Medical Sciences Academy, 25(3), 199.
- ↑ Nigam A, Saxena P, Prakash A & Acharya AS. (2012). Detection of fetal nucleic acid in maternal plasma: A novel noninvasive prenatal diagnostic technique. Journal of Internation Medical Sciences Academy, 25(3), 199.
- ↑ 9.0 9.1 <pubmed>20663958</pubmed>
- ↑ 10.0 10.1 <pubmed>24996040</pubmed>
- ↑ <pubmed>22223204</pubmed>
- ↑ Society for the Study of Reproduction. (2012, June 6). Three types of fetal cells can migrate into maternal organs during pregnancy: Some mothers literally carry pieces of their children in their bodies. ScienceDaily. Retrieved July 20, 2014 from www.sciencedaily.com/releases/2012/06/120606155802.htm
- ↑ Soothill, PW & Lo, YMD. (2014). Non-invasive prenatal testing for chromosomal abnormality using maternal plasma DNA. Scientific Impact Paper, (15)
- ↑ Soothill, PW & Lo, YMD. (2014). Non-invasive prenatal testing for chromosomal abnormality using maternal plasma DNA. The Obstetrician & Gynaecologist, 16(2), 148-148. doi:10.1111/tog.12099)
- ↑ <pubmed>24734183</pubmed>
- ↑ <pubmed>24496666</pubmed>