Advanced - Abnormalities
| Begin Advanced | Heart Fields | Heart Tubes | Cardiac Looping | Cardiac Septation | Outflow Tract | Valve Development | Cardiac Conduction | Cardiac Abnormalities | Molecular Development |
| Cardiac Embryology | Begin Basic | Begin Intermediate | Begin Advanced |
Congenital Heart Disease (CHD) is a broad term for a variety of cardiac and vasculature pre-natal defects. They affect about 8-10 of every 1,000 births in the United States. This increases considerably to 75 in 1,000 births if trivial lesions are included and even more so in those stillborn or spontaneously aborted. Cardiovascular abnormalities are the most common form of birth defect, comprising around 20% of all congenital malformations. In addition, given the increasing survival of patients with CHD, treated or untreated, it is expected that large numbers of adults will maintain CHD in the future. Hence CHD becomes a significant part of the clinical environment. The table below outlines some of the common obstructive, septal and hypoplastic defects in order of their incidence.
| Diagram | Abnormality | Epidemiology | Description |
|---|---|---|---|
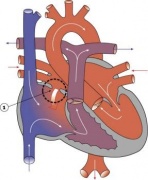
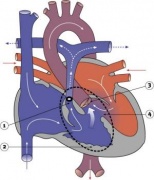
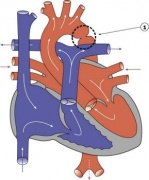
| Ventricular Septal Defect | 25% of CHD; more frequent in males | Result from growth failure of the membranous IV septum or endocardial cushions leading to a lack of closure of the IV foramen. Many VSDs are actually from defects in the outflow tract septum. 30-50% close spontaneously; large VSDs result in dyspnoea and cardiac failure in infancy. | |
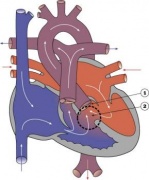
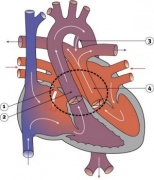
| Tetralogy of Fallot | 9-14% of CHD | Comprises a classic group of four defects: pulmonary stenosis, VSD, dextroposition of the aorta and right ventricle hypertrophy. An additional ASD creates a ‘pentalogy’ of Fallot. Results in cyanosis. | |
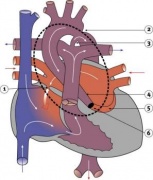
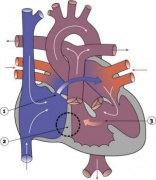
| Transposition of the Great Vessels | 10-11% of CHD | The most common form of transposition is where the aorta arises from the right ventricle while the pulmonary trunk arises from the left. This occurs either via abnormal rotation of the arterial pole or abnormal development of the outflow septum. In order for a newborn to survive prior to surgery there must be mixing of systemic and pulmonary circulations through a VSD, ASD or patent ductus arteriosus. It is the most common cause of cyanotic heart disease in newborns and is surgically corrected. | |
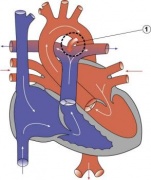
| Atrial Septal Defect | 6-10% of CHD; more common in females | The atrial septal myocardium is derived from multiple sources making various places susceptible to defects. The most common is a patent foramen ovale. Others include an ostium secundum defect and ostium primum defect (where there is usually some defect with the AV cushions as well). Defects in the sinus venosus act as ASDs yet are really defects in the wall separating the right pulmonary veins and SVC. A common atrium results from a complete lack of atrial septation. ASDs are generally acyanotic due to a left-to-right shunt. | |
| Pulmonary Atresia & Pulmonary Stenosis | 10% of CHD | Unequal division of trunks causes cusps to fuse to form a dome with a narrow/non-existent lumen and hence obstruction to blood flow from the right ventricle to the pulmonary artery. The most common side of stenosis/obstruction is at the pulmonary valve itself (rather than distal or proximal to the valve). Heart-lung transplantation may be the only therapy. | |
| Patent Ductus Arteriosus | 6-8% of CHD; 2-3 times more common in females; common in preterm newborns | Failure of contraction of the muscular wall of the DA. This imposes greater pressure on the pulmonary circulation. Many will close spontaneously, however if this does not occur, surgical closure is advised to prevent the development of congestive heart failure. | |
| Aortic Stenosis | 7% of CHD | Stenosis is caused either by a muscular obstruction below the aortic valve, obstruction at the valve itself or aortic narrowing above the valve. The most common site is at the valve itself which results from a persistence of endocardial tissue that normally degenerates. Results in LV hypertrophy and heart murmurs. | |
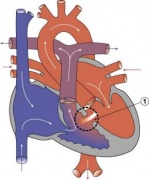
| Hypoplastic Left Heart Syndrome | 4-8% of CHD | The left ventricle is incapable of supporting the systemic circulation, hence the right ventricle maintains both pulmonary and systemic circulations aided by an ASD. Other defects such as stenosis or atresia of the mitral and aortic valves, anomalous pulmonary venous connections and hypoplasia of the aortic arch can be responsible for hypoplastic left heart syndrome. Infants usually die within weeks. | |
| Coarctation of the Aorta | 5-7% of CHD | Aortic constriction in the region of the ductus arteriosus. It is associated with patent ductus arteriosus, VSD and aortic stenosis. Closure of the ductus arteriosus in neonates with a coarctation imposes a greater afterload on the left ventricle which can lead to congestive heart failure. Treatment aims at maintaining the ductus arteriosus via prostaglandins. | |
| Partial/Total Anomalous Pulmonary Venous Connection | <4% of CHD; more common in females | In partial anomalous pulmonary venous drainage (PAPVD) a portion of the pulmonary venous blood flow returns to the right atrium. When over 50% of the veins return to the right atrium the condition is clinically significant. All types of total anomalous pulmonary venous connection (TAPVC) (those compatible with survival) are accompanied by an atrial septal defect. Pulmonary veins in TAPVC tend to open into one of the systemic veins before returning to the right atrium. The overloaded pulmonary circuit leads to cyanosis, tachypnoea and dyspnoea. Treatment is via surgical redirection. | |
| Tricuspid Atresia | 1-3% of CHD | Complete lack of formation of the tricuspid valve which results in an hypoplastic right ventricle. The pulmonary circulation can be maintained via a VSD, and an ASD is necessary for survival. Results in cyanosis and tachypnoea. Treatment is initially via administration of prostaglandins followed by surgery to place a shunt to maintain the pulmonary circulation. | |
| Double Outlet Right Ventricle | 1-1.5% of CHD | Both large arteries arise wholly or mainly from the right ventricle. This defect is considered to be present if the aorta obtains 50% of its blood from the right ventricle. The defect arises due to absence of the secondary heart field such that myocardium is not added to the outflow tract during looping. Arrangement of the atrioventricular valves, coronary arteries and the ventriculoarterial connections as well as clinical manifestations are variable. | |
| Interrupted Aortic Arch | Very rare | An extreme form of coarctation of the aorta involving a gap in the ascending or descending thoracic aorta that results from abnormal proliferation/migration/function of neural crest cells. Different types of interrupted aortic arch are defined based on their relation to the arterial branches of the aortic arch. It is greatly associated with other defects such as a patent ductus arteriosus or VSD. It is treated with prostaglandin to maintain ductus arteriosus followed by surgery. |
| Back to the Conduction System | Next: Molecular Control | |
| Go to this section in the intermediate level |